CF‑Related Liver Disease: Quick Guide for Patients and Families
If you or someone you love has cystic fibrosis (CF), the liver might be on your radar. Around 10‑15% of people with CF develop liver problems, and catching it early makes a big difference. This guide breaks down what CF‑related liver disease looks like, how doctors find it, and what you can do every day to stay healthier.
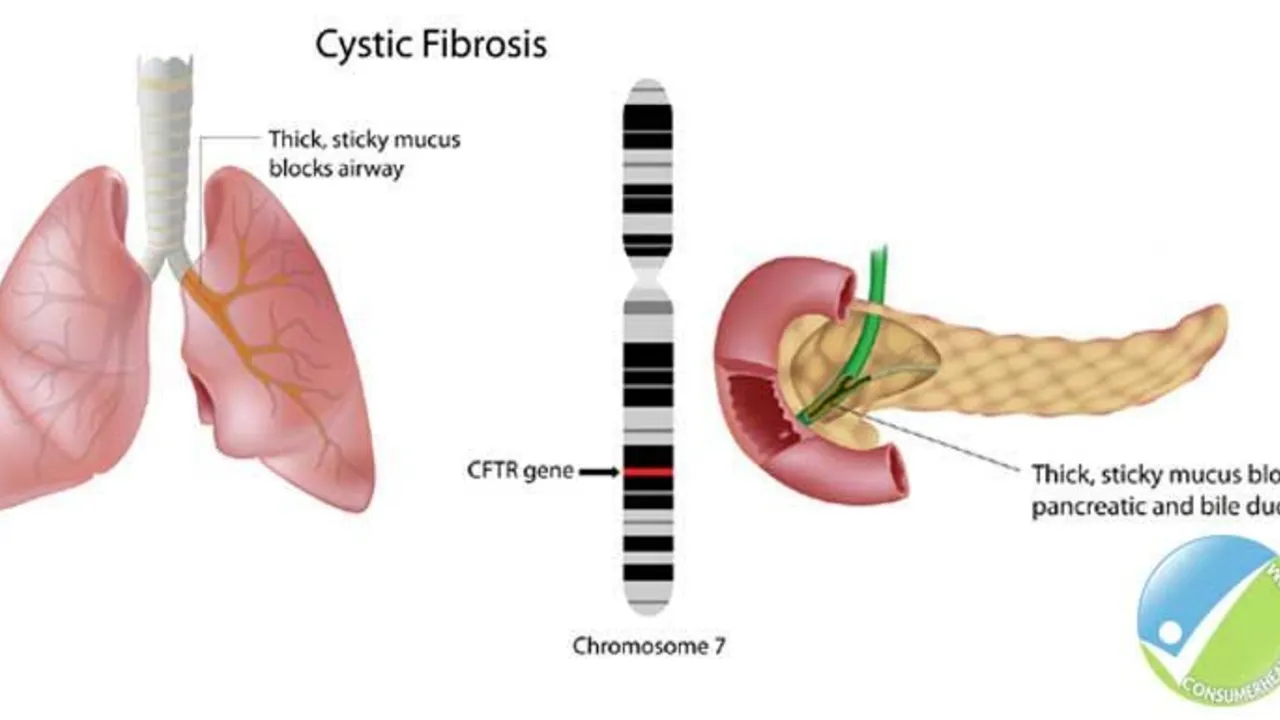
How CF Affects the Liver
CF is a genetic condition that creates thick, sticky mucus in the lungs, pancreas, and other organs. In the liver, that mucus can block tiny ducts that move bile out of the organ. When bile backs up, liver cells get irritated and scar tissue starts to form. Over time the scarring (called fibrosis) can turn into cirrhosis, which means the liver isn’t working as well as it should.
Typical signs show up slowly. You might notice a swollen belly, especially around the waist, or feel unusually tired. Some kids develop a yellow tint to the skin or eyes—called jaundice—because the liver can’t clear bilirubin. Blood tests often reveal higher liver enzymes, even before you feel anything.
Doctors use several tools to confirm the problem. An ultrasound is a quick, painless way to spot liver enlargement or early scarring. If the picture isn’t clear, a MRI or a specialized scan called elastography can measure how stiff the liver tissue is. In rare cases, a tiny tissue sample (biopsy) might be taken to see exactly how much damage has occurred.
Managing CF‑Related Liver Disease
There’s no one‑size‑fits‑all cure, but many steps can slow the disease and improve quality of life. Nutrition is a cornerstone: high‑calorie, high‑protein meals help the liver repair itself. Adding a daily vitamin K supplement can keep clotting normal, since the liver makes clotting factors.
Medication-wise, doctors often prescribe ursodeoxycholic acid (UDCA). UDCA helps thin the bile, making it flow more easily and reducing inflammation. Some patients also benefit from antibiotics that target gut bacteria, lowering the chance of infection that can worsen liver injury.
Regular monitoring is key. Schedule liver function tests every three to six months, and keep up with imaging studies as your doctor suggests. If fibrosis progresses to cirrhosis, you may need more aggressive treatment, including potential liver transplant evaluation. Transplant isn’t a first‑line option, but for advanced cases it can be life‑saving.
Lifestyle tweaks also help. Avoid alcohol completely— even a little can add stress to a vulnerable liver. Stay active with light‑to‑moderate exercise; moving around improves blood flow and helps the liver do its job. Keep vaccinations up to date, especially for hepatitis A and B, because infections can hit the liver hard.
Finally, lean on your care team. CF specialists, dietitians, and liver experts work best when they communicate. Bring up any new symptoms right away, and don’t hesitate to ask for clarification on meds or diet plans. The more informed you are, the easier it is to make decisions that keep the liver working.
CF‑related liver disease can feel scary, but with the right monitoring, nutrition, and treatment you can keep it under control. Stay proactive, stay connected with your doctors, and remember that many people with CF lead full, active lives despite liver challenges.