Anticoagulants: Warfarin vs. DOACs - Safety, Side Effects, and What You Need to Know
Choosing Between Warfarin and DOACs: What Really Matters for Safety
If you’re on a blood thinner, you’ve probably heard the names warfarin and DOACs thrown around. Maybe your doctor switched you. Maybe you’re researching options. Either way, the question isn’t just which one works-it’s which one is safest for you.
Warfarin has been the go-to blood thinner for over 70 years. But since 2010, a new group of drugs-direct oral anticoagulants, or DOACs-has taken over. Today, nearly 8 out of 10 anticoagulant prescriptions in the U.S. are for DOACs. Why? Because for most people, they’re simpler and safer. But that doesn’t mean warfarin is obsolete. In fact, for some, it’s still the only safe choice.
How Warfarin Works-and Why It’s So Hard to Get Right
Warfarin doesn’t just thin your blood. It messes with your body’s vitamin K cycle, which is how your blood clots naturally. That’s powerful-but also unpredictable. Your dose depends on a blood test called INR, which needs to stay between 2.0 and 3.0. Too low, and you risk a clot. Too high, and you risk a bleed.
Getting that balance right isn’t easy. Most people need 6 to 12 INR checks in the first month alone. After that, it’s usually 2 to 4 per month. If you miss a test, your risk goes up. And it’s not just about frequency. Studies show that nearly 35% of warfarin users don’t stick to their monitoring schedule. That’s not laziness-it’s logistics. Getting blood drawn every few weeks is expensive, time-consuming, and stressful.
Then there are the interactions. Warfarin clashes with over 300 medications, from antibiotics to ibuprofen. Even your diet matters. A big bowl of kale or spinach? That’s vitamin K-and it can throw your INR off. One study found that 89% of patients on warfarin said dietary restrictions were their biggest hassle. That’s why many people feel like they’re walking on eggshells just to stay safe.
DOACs: The New Standard-and Why They’re Simpler
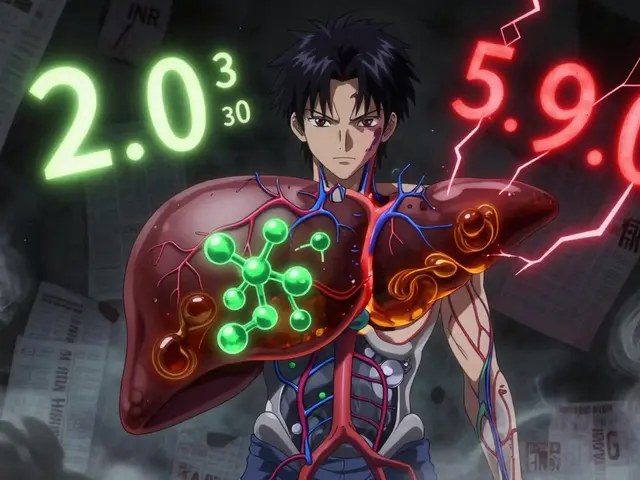
DOACs-like apixaban (Eliquis®), rivaroxaban (Xarelto®), dabigatran (Pradaxa®), and edoxaban (Savaysa®)-work differently. Instead of messing with vitamin K, they target specific clotting factors directly. Apixaban and rivaroxaban block factor Xa. Dabigatran blocks thrombin. That means fewer variables. No INR tests. No diet changes. No daily guessing games.
That simplicity shows up in real life. A 2023 study found that DOAC users had 32% higher adherence than warfarin users. For people under 45, that gap jumped to 41%. Why? Because they don’t have to rearrange their lives around blood tests. One patient on Reddit said, “I used to plan my whole week around my INR appointment. Now I just take my pill and forget about it.”
And the safety data backs it up. In atrial fibrillation patients, DOACs cut stroke risk by 30% and major bleeding by 28% compared to warfarin. The biggest win? Intracranial bleeding-bleeding in the brain. DOACs reduce that risk by half. That’s huge. A brain bleed is one of the most devastating complications of anticoagulation. For many, that alone makes DOACs the better choice.
When DOACs Aren’t the Answer
DOACs aren’t magic. They have limits. And if you fall into one of these categories, warfarin is still your best-or only-option.
- Mechanical heart valves: DOACs are dangerous here. Studies show they increase the risk of clots on the valve. Warfarin is the only approved option.
- Severe kidney failure (eGFR below 15): Most DOACs are cleared by the kidneys. If your kidneys are barely working, the drug builds up. Warfarin doesn’t rely on kidneys, so it’s safer.
- Severe mitral stenosis: This valve problem changes how blood flows. DOACs haven’t been proven safe here. Stick with warfarin.
- Dialysis patients: There’s still not enough data on DOACs in this group. Many doctors still choose warfarin.
And here’s a twist: even among DOACs, not all are equal. Apixaban has the lowest bleeding risk. Rivaroxaban has a slightly higher chance of stomach bleeding. Dabigatran is better at preventing clots but can cause more stomach upset. Your doctor doesn’t just pick a DOAC-they pick the right DOAC for your body.

Cost: The Hidden Barrier
Let’s be real. DOACs are expensive. A 30-day supply of apixaban costs around $587. Rivaroxaban? Over $520. Dabigatran? Nearly $490. Warfarin? $4.27.
That’s not a typo. Warfarin is over 100 times cheaper. For people without good insurance, that gap is life-changing. Some patients on forums say they’ve gone back to warfarin just to afford it. Others skip doses to make it last. That’s not safe. But it’s real.
Insurance can help-but not always. Some plans require you to try warfarin first. Others don’t cover certain DOACs unless you’ve failed others. If cost is a problem, talk to your doctor. There are patient assistance programs. Generic options are coming. And in some cases, the long-term savings from fewer hospital visits can outweigh the upfront cost.
Reversing the Blood Thinner: What Happens in an Emergency?
What if you fall and crack your head open? What if you need emergency surgery? With warfarin, you can give vitamin K or fresh frozen plasma to reverse it. It takes hours, but it works.
With DOACs, it’s different. There are specific reversal agents now. Idarucizumab (Praxbind®) reverses dabigatran. Andexanet alfa (Andexxa®) reverses apixaban and rivaroxaban. These are expensive, hard to get, and only available in hospitals. But they work fast-within minutes.
That’s a big upgrade from 10 years ago. But it’s not perfect. Edoxaban doesn’t have a dedicated reversal agent yet. And if you’re on a DOAC and end up in an ER that doesn’t stock these drugs, you’re stuck waiting for the drug to wear off. That’s why knowing what you’re on-and telling every doctor you see-is critical.
What Your Doctor Should Check Before Prescribing
It’s not just about picking the right drug. It’s about checking the right things first.
- Renal function: eGFR must be tested. DOACs need different doses based on kidney health. Some shouldn’t be used below a certain level.
- Drug interactions: St. John’s wort, rifampin, and certain antifungals can make DOACs less effective. Anti-seizure meds and HIV drugs can be dangerous.
- Body weight: Very low body weight (under 60 kg) may need lower doses of some DOACs.
- History of bleeding: If you’ve had a GI bleed before, apixaban is often preferred over rivaroxaban.
- Heart valve status: Mechanical valves? Warfarin only.
Too often, patients are started on DOACs without checking kidney function. That’s risky. A 2023 study found that 18% of DOAC prescriptions in primary care didn’t include an eGFR test. That’s not just a mistake-it’s a safety gap.

Real-Life Decisions: Who Wins?
Let’s put this in human terms.
Meet Maria, 72, with atrial fibrillation. She’s active, travels often, hates blood tests. Her doctor puts her on apixaban. She takes it once a day. No diet changes. No monthly trips to the lab. Her INR? Never checked. Her risk of stroke drops. Her risk of brain bleed drops. She sleeps better.
Now meet Raj, 68, with a mechanical mitral valve. He’s been on warfarin for 12 years. His INR is stable. He knows his numbers. He eats kale, but he times it. He’s had no clots, no bleeds. Switching him to a DOAC? Not an option. His life depends on warfarin.
One isn’t better than the other. It’s about matching the drug to the person.
What to Ask Your Doctor
If you’re on a blood thinner-or thinking about starting one-ask these questions:
- “Why are you recommending this drug over the other?”
- “What’s my kidney function? Does that affect my dose?”
- “Do I have a mechanical valve or severe mitral stenosis?”
- “What happens if I need emergency surgery?”
- “Is there a cheaper option? Are there patient assistance programs?”
- “What are the signs of bleeding I should never ignore?”
Don’t let them brush you off. This isn’t just a pill. It’s a daily decision that affects your life, your safety, and your future.
Bottom Line: Safety Isn’t One-Size-Fits-All
DOACs are safer and easier for most people. That’s why they’re the new standard. But warfarin still saves lives-for people with mechanical valves, severe kidney failure, or those who can’t afford DOACs.
The best anticoagulant isn’t the one with the fanciest name. It’s the one that fits your body, your lifestyle, and your risk profile. It’s the one you’ll actually take. And it’s the one your doctor checks for-not just once, but over and over.
Don’t assume your first prescription is your last. Ask questions. Revisit your plan. Your safety depends on it.


Georgia Green
i took warfarin for 3 years and honestly the diet stuff was the worst. i loved spinach but had to count leaves like it was a math problem. switched to eliquis and never looked back. no more needles every other week.
ps: i typoed that last sentence. forgive me.
Christina Abellar
This is such a clear breakdown. I appreciate how you laid out the trade-offs without pushing one over the other.
Eva Vega
The pharmacokinetic profiles of DOACs exhibit significantly reduced inter-individual variability compared to vitamin K antagonists, primarily due to their targeted inhibition of factor Xa or thrombin. This translates to more predictable anticoagulation without the need for routine coagulopathy monitoring.
Matt Wells
It is regrettable that so many patients are presented with oversimplified narratives regarding anticoagulant therapy. The clinical nuances-particularly regarding renal clearance thresholds and the absence of reversal agents for edoxaban-are too frequently glossed over in popular discourse.
George Gaitara
Y’all act like DOACs are some miracle cure. Newsflash: Big Pharma pushed them hard because they make 100x the profit. And now everyone’s on them and we’ve got a whole generation of people who don’t know how to read an INR. Who’s to blame? Not the doctors. Not the patients. The corporations.
Joyce Genon
Okay so let me get this straight. You’re telling me that people with mechanical valves are just out of luck because DOACs aren’t approved? That’s insane. What if someone can’t afford warfarin? What if they live in a rural area with no lab access? What if they’re undocumented and can’t get insurance? This isn’t medicine, it’s a class war disguised as a clinical guideline. And don’t even get me started on the fact that Andexxa costs $30,000 a dose. We’re literally letting people die because the system is broken. And you’re all just sitting here talking about INR levels like it’s a grocery list.
John Wayne
DOACs are just a marketing ploy wrapped in clinical trial data. The real reason they're preferred isn't safety-it's that doctors don't want to deal with INR logs. Convenience over care. And now we have patients who don't know how to manage their own health because they've been coddled with pills that 'just work.'
Julie Roe
I’ve been a nurse for 18 years and I’ve seen both sides. Warfarin patients often feel like they’re on a treadmill-always checking, always adjusting, always worried. DOAC patients? They breathe easier. But I also know the ones who can’t afford them. I’ve had patients skip doses to stretch their pills. I’ve had them cry because they chose between food and medicine. So yes, DOACs are better for most. But if we don’t fix the cost issue, we’re just trading one kind of suffering for another. It’s not just about the drug-it’s about the whole system. And we owe it to people to fix both.
jalyssa chea
why do doctors even bother with all this science when they just listen to big pharma ads anyway i bet most of them dont even check kidney function i saw my doc for 5 mins and he handed me a script for xarelto like it was coffee
Gary Lam
Man, I lived in Thailand for a year and they still use warfarin there. No fancy DOACs. Just cheap pills, a little bit of spinach, and a whole lot of trust. People there don’t have fancy labs but they’ve got community health workers who show up at their door with test kits. Maybe we need less tech and more human touch. Also, I’m pretty sure your doctor doesn’t care if you eat kale. He’s just trying to get out of the office by 5.
Peter Stephen .O
I’ve been on apixaban for two years now and it’s like my blood finally got a vacation. No more weekly blood draws, no more panic when I eat a salad, no more ‘did I take it today?’ anxiety. I used to feel like my body was a broken machine that needed constant tuning. Now? I just take it. And I sleep. I actually sleep. That’s the real win. And yeah, it’s pricey-but I’ve saved on ER visits and ambulance rides. That’s the hidden math. Also, shoutout to the docs who actually check eGFR. You’re the real MVPs.
Andrew Cairney
EVERYONE KNOWS THE GOVT IS HIDING THE TRUTH ABOUT DOACS. THEY’RE DESIGNED TO MAKE YOU DEPENDENT. THEY’RE LINKED TO THE 5G NETWORK AND CAUSE MICROBLOOD CLOTS. WHY DO YOU THINK THEY DON’T HAVE A REVERSAL AGENT FOR EDXOBA? BECAUSE THEY WANT YOU TO DIE SLOWLY SO THEY CAN COLLECT YOUR DATA. I KNOW A GUY WHO WORKED AT A PHARMA LAB AND HE SAID THEY’RE TESTING ON VETERANS. DON’T TRUST THE SYSTEM. #DOACCONSPIRACY #SAVEWAFARIN
Roberta Colombin
Thank you for writing this with such care and clarity. It is rare to see a medical topic presented without fear or hype. I hope this reaches those who need it most.
Dave Feland
The entire DOAC paradigm is a construct of the pharmaceutical-industrial complex. There is no evidence that they are safer than warfarin in the long term. The studies are funded by the manufacturers. The guidelines are written by consultants with stock options. And yet, the public is told this is ‘science.’ It’s not. It’s branding.
Ashley Unknown
I was on Xarelto for 11 months and then had a GI bleed that nearly killed me. They said it was ‘rare.’ But I’ve met 3 other people who had the same thing. And none of them had a history of ulcers. I think the drug is a ticking time bomb. And now my insurance won’t cover warfarin because I ‘failed’ the DOAC first. So I’m stuck paying $600 a month for a drug that almost killed me. And the system says that’s fair.