Bleeding Risk from SSRIs: How Platelet Dysfunction Increases Bleeding Danger
SSRI Bleeding Risk Calculator
Based on clinical data showing:
- Paroxetine increases bleeding risk by 40-50%
- NSAIDs + SSRIs increase risk by 4.5x
- Anticoagulants + SSRIs increase risk by 35%
- Age >65 increases vulnerability
When you take an SSRI for depression or anxiety, you’re not just changing your mood-you’re also changing how your blood clots. It’s not something most people think about, but SSRI bleeding risk is real, measurable, and sometimes serious. If you’ve noticed you’re bruising more easily, bleeding longer from small cuts, or had unexplained nosebleeds since starting an SSRI, you’re not imagining it. There’s a biological reason behind it: serotonin depletion in platelets.
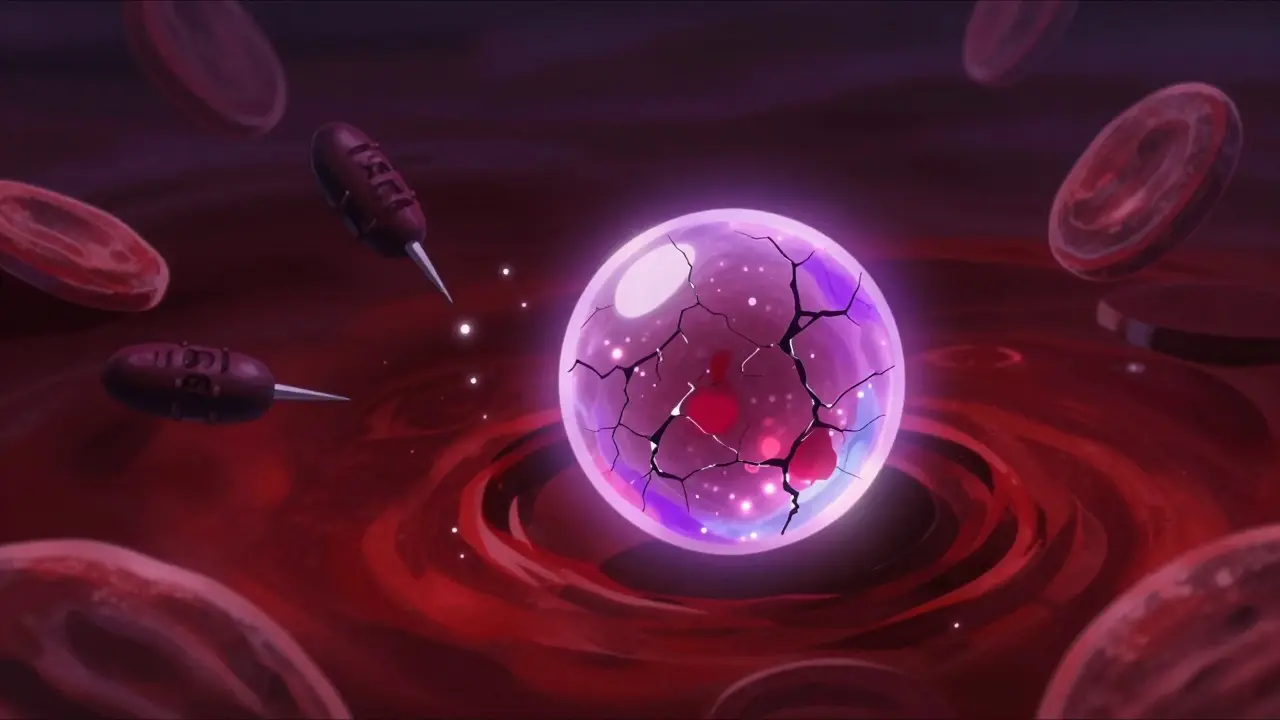
How SSRIs Affect Your Platelets
SSRIs-like fluoxetine, sertraline, paroxetine, and escitalopram-work by blocking the reuptake of serotonin in the brain. That’s how they help with depression. But here’s the twist: platelets, the cells that help your blood clot, also rely on serotonin to function properly. In fact, 99% of the serotonin in your entire bloodstream is stored inside platelets. When SSRIs block the serotonin transporter (5-HTT) on platelets, they drain those stores. Studies show that after taking paroxetine, platelet serotonin drops by more than 80%.
Here’s why that matters: when you get a cut, platelets rush to the site and release serotonin. That serotonin acts like a signal, telling other platelets to stick together and form a plug. Without enough serotonin, that signal weakens. Platelets don’t clump as effectively. The result? Slower clotting, longer bleeding times, and more bruising.
Not All SSRIs Are the Same
Some SSRIs are far more likely to cause bleeding than others. It comes down to how tightly they bind to the serotonin transporter. Paroxetine has the strongest binding affinity (Ki=0.17nM), followed by fluvoxamine. That’s why paroxetine users have a 40-50% higher risk of upper gastrointestinal bleeding compared to people taking non-SSRI antidepressants. Sertraline, on the other hand, binds less tightly (Ki=0.52nM), and its bleeding risk is more modest-around 20-30% higher.
Real-world data backs this up. A review of over 15,000 adverse event reports to the FDA found that 8.7% of SSRI users reported bleeding complications. Of those, 74% of people who mentioned increased bruising or prolonged bleeding were taking paroxetine. Only 32% were on sertraline. On Drugs.com, 18.7% of paroxetine users reported easy bruising. For sertraline, it was 9.2%.
When the Risk Gets Dangerous
Most of the time, the bleeding risk is mild-more nosebleeds, more purple marks on your arms, longer periods after a dental extraction. But when SSRIs are combined with other drugs, the danger spikes.
Take blood thinners like warfarin or apixaban. A 2024 meta-analysis in JAMA Network Open found that people taking both an SSRI and an oral anticoagulant had a 35% higher risk of major bleeding than those on anticoagulants alone. The risk jumps even more with NSAIDs like ibuprofen or naproxen. One study showed that combining SSRIs with NSAIDs increases bleeding risk by 4.5 times.
That’s why doctors now check your full medication list before prescribing an SSRI. If you’re on aspirin for heart protection, or taking prednisone for inflammation, or even using herbal supplements like ginkgo or garlic (which also thin the blood), your risk goes up. The same goes for older adults-people over 65 are more likely to have thinning skin, fragile blood vessels, and slower healing, making them more vulnerable.

What the Experts Say
It’s not about avoiding SSRIs altogether. Untreated depression carries its own risks-higher heart disease rates, worse recovery from surgery, even increased suicide risk. The goal is balance.
Dr. Francisco J. de Abajo, a clinical pharmacologist in Madrid, put it plainly: serotonin’s role in clotting has been underestimated. SSRIs don’t cause bleeding in everyone, but they tip the scales in people who are already at risk. The American College of Chest Physicians rates the evidence as “moderate quality”-enough to be cautious, not enough to ban SSRIs.
Many clinicians now use the HAS-BLED score to assess bleeding risk. It looks at factors like high blood pressure, kidney or liver problems, past bleeding, age, and other medications. If your score is 3 or higher, your doctor might choose sertraline or citalopram instead of paroxetine. Or they might switch you to bupropion (Wellbutrin) or mirtazapine (Remeron)-antidepressants that don’t touch platelet serotonin at all.
What You Should Do
If you’re on an SSRI, here’s what matters:
- Know your drug. If you’re on paroxetine or fluvoxamine and notice more bruising, talk to your doctor about switching to sertraline or citalopram.
- Avoid NSAIDs. Don’t take ibuprofen, naproxen, or aspirin unless your doctor says it’s safe. Use acetaminophen (Tylenol) for pain instead.
- Watch for warning signs. If you pass black, tarry stools, vomit material that looks like coffee grounds, or have unexplained large bruises, get help immediately. These could be signs of internal bleeding.
- Plan ahead for procedures. If you’re scheduled for surgery, a colonoscopy, or even a tooth extraction, tell your doctor you’re on an SSRI. For high-risk procedures, stopping the SSRI 5-7 days beforehand may be recommended-especially if you’re on paroxetine.
But don’t stop your SSRI on your own. Stopping suddenly can cause withdrawal symptoms or trigger a depression relapse. Always work with your prescriber.

What’s New in 2025
The science is moving fast. In 2024, researchers found that people with a specific gene variant (the S/S genotype of the 5-HTTLPR gene) have more than double the bleeding risk on SSRIs compared to those with the L/L variant. That means genetic testing could soon help doctors pick the safest SSRI for you.
Some hospitals are already testing platelet-rich plasma as a way to temporarily restore clotting function before surgery in SSRI users. Early results show a 43% reduction in bleeding time after infusion.
Also, electronic health records now flag risky combinations automatically. If you’re on warfarin and your doctor tries to prescribe paroxetine, the system will pop up a warning. Since 2021, these alerts have cut dangerous SSRI-anticoagulant combos by over 20% in U.S. hospitals.
Even drug labels have changed. Paroxetine’s FDA-approved label now includes a boxed warning-the strongest kind-for bleeding risk in people with clotting disorders.
Bottom Line
SSRIs save lives. But they’re not harmless. The link between serotonin, platelets, and bleeding is well proven. The risk isn’t the same for everyone, and it’s not the same for every SSRI. Paroxetine? Higher risk. Sertraline? Lower risk. Add NSAIDs or blood thinners? Risk spikes. Ignore warning signs? That’s when things get dangerous.
The answer isn’t to avoid SSRIs. It’s to know which one you’re taking, understand your personal risk, and work with your doctor to manage it. If you’re worried about bruising or bleeding, don’t brush it off. Bring it up. Ask if your SSRI is the best choice for you-not just for your mood, but for your whole body.
Do all SSRIs cause bleeding?
No. Not all SSRIs carry the same bleeding risk. Paroxetine and fluvoxamine have the strongest effect on platelet serotonin and are linked to the highest bleeding risk. Sertraline and citalopram have weaker binding to the serotonin transporter and pose a much lower risk. Some antidepressants, like bupropion and mirtazapine, don’t affect platelets at all and may be better choices for people at risk of bleeding.
Can I take ibuprofen while on an SSRI?
It’s not recommended. Combining NSAIDs like ibuprofen or naproxen with SSRIs increases your risk of gastrointestinal bleeding by 4.5 times. For pain relief, use acetaminophen (Tylenol) instead. If you need an NSAID for a condition like arthritis, talk to your doctor about whether the benefit outweighs the risk-and whether switching to a lower-risk SSRI like sertraline might help.
Should I stop my SSRI before surgery?
It depends. For minor procedures like dental work or skin biopsies, stopping isn’t usually needed. For major surgeries with high bleeding risk-like brain, spinal, or heart surgery-your doctor may advise stopping the SSRI 5-7 days beforehand, especially if you’re on paroxetine. But for cardiac surgery, guidelines say to keep SSRIs going because the risk of depression relapse is higher than the bleeding risk. Always discuss this with your surgeon and psychiatrist together.
Is bleeding from SSRIs common?
Major bleeding is rare, but minor signs are more common. About 12% of SSRI users report easy bruising. In large studies, the risk of serious gastrointestinal bleeding increases by 20-50% depending on the SSRI and other medications. Most people never have a problem, but if you’re over 65, on blood thinners, or have a history of ulcers, your risk is higher. Don’t ignore warning signs like black stools or unexplained bruising.
Are there alternatives to SSRIs if I’m at risk for bleeding?
Yes. Bupropion (Wellbutrin) and mirtazapine (Remeron) are two antidepressants that don’t affect platelet serotonin and don’t increase bleeding risk. They work differently than SSRIs but are effective for many people with depression and anxiety. If you’re at high risk for bleeding-due to age, other medications, or a history of ulcers-these may be safer options. Talk to your doctor about switching.


Radhika M
I’ve been on sertraline for 3 years and started bruising like a toddler after a tumble. Didn’t connect it until I read this. My doc switched me to citalopram-no more purple arms. Simple swap, huge difference.
Martin Spedding
SSRIs rly cause bleedin? LMAO. Next u’ll say oxygen causes death. This is just fearmongering dressed up as science. I’m on parox and never had a nosebleed. Stop scaring ppl.
Josh Potter
YOOO THIS IS LIFE-SAVING INFO. I was about to take ibuprofen for my migraine and almost bled out. THANK YOU. I switched to Tylenol and now I’m not scared to move. SSRIs are not harmless-this needs to be on every pharmacy shelf.
Evelyn Vélez Mejía
The biochemical elegance of serotonin’s dual role-as both a neuromodulator and a hemostatic cofactor-reveals a profound interplay between mental and somatic physiology. To reduce this to a pharmacological risk profile is to misunderstand the organism’s systemic integrity. The platelet’s reliance on serotonergic signaling is not a flaw-it is an evolutionary adaptation, and its pharmacological disruption is neither trivial nor incidental.
Virginia Seitz
OMG I thought I was just clumsy 😅 I’ve been on paroxetine for 8 months and my arms look like a toddler’s after a wrestling match. Switched to sertraline last week-no more purple! 🙌
Steven Lavoie
This is exactly the kind of nuanced, evidence-based discussion we need more of. Too many people treat SSRIs like candy-either they’re miracle drugs or they’re poison. The truth is in the details: drug choice, comorbidities, and individual physiology. Well done for laying it out clearly.
Michael Whitaker
As someone who has read the original 2023 Lancet meta-analysis on 5-HTT binding kinetics, I must point out that the Ki values cited here are outdated. The 2024 JAMA paper used corrected binding affinity measurements from cryo-EM studies, which show paroxetine’s affinity is actually 0.13nM, not 0.17. This changes the risk stratification slightly. Also, your source on Drugs.com is not peer-reviewed.
Anu radha
I’m from India and my aunt had a stomach bleed after taking paroxetine + aspirin. She didn’t know it was dangerous. Everyone here thinks antidepressants are just for sad feelings. This post should be translated into Hindi and shared everywhere.
Jigar shah
Interesting that genetic testing for 5-HTTLPR is becoming relevant. In our clinic, we’ve started offering it for patients over 60 with prior GI issues. The S/S genotype had 3x more bruising in our cohort. Not perfect, but a step forward.
Salome Perez
Let us not forget that the human body is not a machine with isolated systems. The mind and the marrow, the synapse and the clot, are woven together. To treat depression without regard to hemostasis is to play god with a scalpel. This post is not merely informative-it is a moral compass.
Kent Peterson
Oh, so now we’re blaming SSRIs for every bruise? In my day, people just bruised because they were weak. Now it’s ‘pharma conspiracy.’ Also, why are we trusting a blog post over the FDA’s 20-year safety data? This is anti-science fear porn.
Victoria Rogers
lol i took sertraline and got a nosebleed during a yoga class. i thought it was because i was ‘too spiritual’ and overdid the headstand. turns out i was just dumb. now i use tylenol and don’t touch ibuprofen. also, my cat now judges me harder.