HIV and AIDS: Modern Treatment, Medications, and Quality of Life

Twenty years ago, an HIV diagnosis meant a death sentence. Today, it’s a chronic condition - one that can be managed with the same routine as high blood pressure or diabetes. The difference? HIV treatment has changed more in the last decade than it did in the first 20 years of the epidemic.
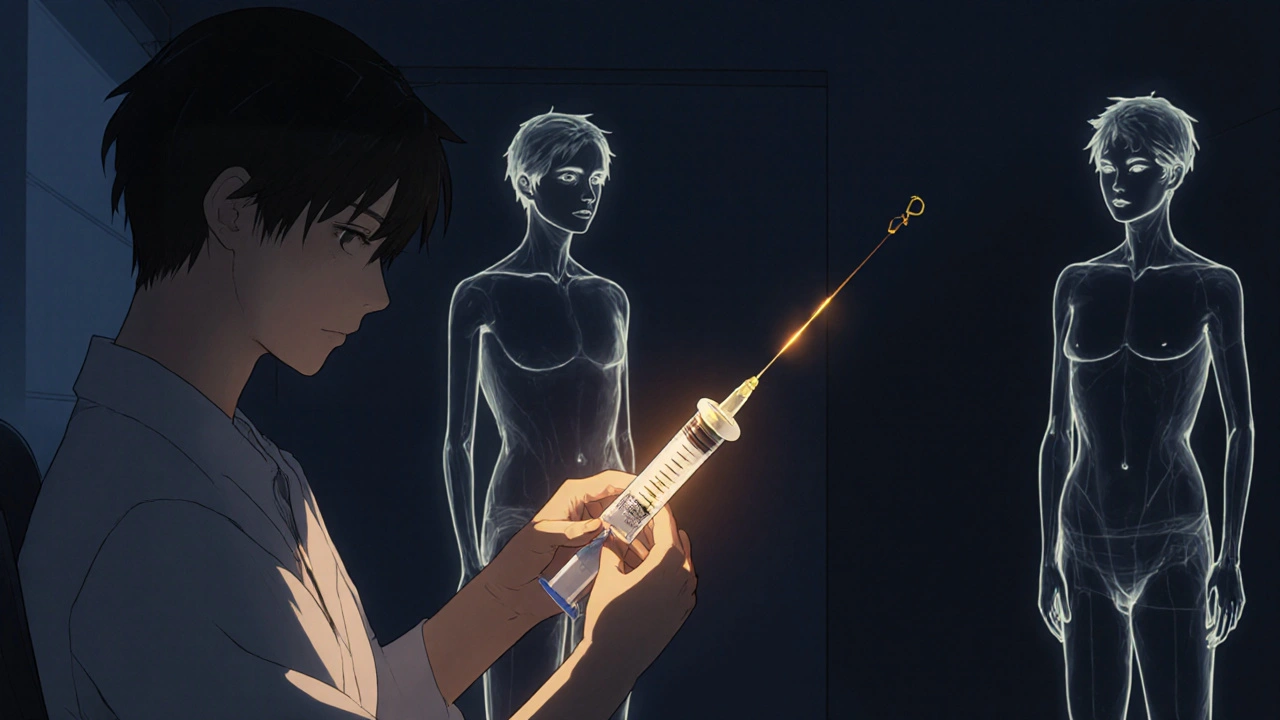
From Daily Pills to Twice-Yearly Injections
The biggest shift in HIV care isn’t a new drug - it’s the rhythm of treatment. For decades, people living with HIV took one or more pills every single day. Missing a dose could mean the virus coming back. That stress, that constant reminder - it wore people down, mentally and emotionally. Now, there’s something new: lenacapavir. Approved in 2022 for treatment and in 2025 for prevention (as Yeztugo), it’s the first HIV medication that works for six months after just one shot. In early 2025, researchers combined it with two other drugs - teropavimab and zinlirvimab - to create a regimen called LTZ. In trials, it suppressed the virus in 98.7% of people after 48 weeks. That’s better than daily pills. And the side effects? Only 12% of people had mild pain or swelling at the injection site. Most said it was worth it. One person on Reddit wrote: “After 12 years of daily pills, the twice-yearly injection has eliminated my treatment-related anxiety completely.”How Modern HIV Drugs Work
HIV attacks your immune system by hijacking CD4 cells. To stop it, drugs block different parts of the virus’s life cycle. Today’s treatments use combinations from seven drug classes:- NRTIs - fake building blocks that stop the virus from copying itself (like tenofovir, emtricitabine)
- INSTIs - block the virus from inserting its DNA into your cells (bictegravir, doravirine)
- Protease inhibitors - stop the virus from maturing into infectious particles
- CCR5 antagonists - lock the door the virus uses to enter cells
- Fusion inhibitors - prevent the virus from fusing with your cells
- Capsid inhibitors - disrupt the virus’s protective shell (lenacapavir)
Leading Regimens in 2025
You don’t need to remember all the drug names, but knowing the top options helps when talking to your doctor:- Biktarvy - A single pill with three drugs (bictegravir, emtricitabine, tenofovir alafenamide). It’s small, light, and taken once daily. Used by over 70% of new patients in the U.S. in 2024.
- DELSTRIGO - Another daily pill, good for people with kidney issues because it uses a different form of tenofovir.
- Sunlenca (lenacapavir) - The first long-acting treatment. Injected under the skin every six months. Requires a clinic visit, but no pills.
- Yeztugo - The same drug, now approved for prevention. For people at high risk of HIV, it’s a shot twice a year instead of a daily pill.
- LTZ (investigational) - Lenacapavir + two antibodies. Expected to be approved in mid-2026. Could become the new gold standard.
Quality of Life: More Than Just Viral Suppression
Suppression means the virus is undetectable. That’s great - it means you can’t transmit HIV to others. But treatment isn’t just about numbers. It’s about your life. A 2025 survey of 150,000 people with HIV found that 92% on long-acting therapies rated their satisfaction as 8 out of 10 or higher. Only 76% of people on daily pills said the same. Why? Because long-acting treatments remove the daily mental burden. No more panic when you travel. No more hiding pills at work. No more guilt when you forget. People report better sleep, less anxiety, and more freedom. One woman in New Zealand told her clinic: “I used to check my calendar every day for my pill time. Now I just remember: ‘June and December.’ That’s it.”Cost, Access, and the Global Divide
Here’s the problem: these breakthroughs are expensive. In the U.S., Biktarvy costs about $69,000 a year. Yeztugo is $45,000. But here’s the twist: the actual cost to make these drugs is around $25 per person per year. That’s not a typo. The price difference comes from patents, marketing, and pricing systems - not manufacturing. UNAIDS says 1.3 million new HIV infections happened in 2024. That’s way above the goal of 370,000. Why? Because most people in low-income countries can’t access even the basic pills, let alone the new injections. Only 2% of people in sub-Saharan Africa are on long-acting therapy. In the U.S., it’s 38%. The World Health Organization knows this. That’s why, in July 2025, they said: “Let community health workers give these shots.” In rural clinics, nurses and volunteers can be trained to give the injection. No hospital needed. No specialist. Just a clean needle and a cold pack.
What You Need to Know Before Switching
If you’re on daily pills and thinking about switching to an injection:- Ask if your virus is fully suppressed. You need to be stable for at least 3 months.
- Be ready for a 4-week overlap. You’ll still take your pills for a month while the injection builds up in your system.
- Check if your clinic offers it. As of mid-2025, only 43% of U.S. clinics stock Sunlenca. Storage requires freezing (-20°C), which not all offices can handle.
- Expect mild injection pain. Most people say it feels like a bee sting that lasts 1-3 days. Ice and ibuprofen help.
- Plan your schedule. You’ll need two visits a year. Set calendar reminders. Programs with automated texts saw 96% of people show up on time.
The Future: What’s Next?
By 2030, experts predict 75% of people with HIV in rich countries will use long-acting treatments. In poorer countries? Maybe 40% - if prices drop. Gilead Sciences, the company behind lenacapavir, made $13.2 billion from HIV drugs in 2024. That’s a 14% jump from the year before. Meanwhile, generic manufacturers are preparing to make versions for $25 a year. If they succeed, the global HIV epidemic could end faster than anyone thought. The science is here. The tools exist. The question now is: who gets them?Can you still transmit HIV if you’re on long-acting treatment?
No. If your viral load is undetectable - meaning the virus is suppressed below the level that tests can measure - you cannot transmit HIV, no matter if you’re on daily pills or a twice-yearly injection. This is called U=U: Undetectable = Untransmittable. It’s backed by decades of research and confirmed in every major study, including those for lenacapavir.
Is long-acting HIV treatment safe for everyone?
Most people tolerate it well. But it’s not for everyone. People with severe allergies to any component, those with uncontrolled liver disease, or those who can’t attend regular clinic visits may not be candidates. Your doctor will check your kidney and liver function before starting. If you’ve had injection-site reactions to other shots, talk about it - your provider can adjust the technique.
Can you switch back to daily pills if you don’t like the injection?
Yes. Switching back is safe and common. If you experience side effects, miss appointments, or just prefer pills again, your provider can transition you to an oral regimen. There’s no penalty for changing your mind. The goal is what works best for your life.
How do you get access to lenacapavir if you’re not in the U.S.?
In high-income countries like Canada, Australia, and parts of Western Europe, lenacapavir is available through national health systems. In lower-income countries, access is still limited. But WHO’s 2025 guidelines are pushing for community-based delivery. Look for local HIV clinics or NGOs working with UNAIDS - many are starting pilot programs with trained health workers. Generic versions may become available in 2026-2027.
Does long-acting treatment prevent other STIs?
No. Lenacapavir only prevents or treats HIV. It does not protect against syphilis, gonorrhea, chlamydia, or hepatitis. Condoms and regular STI testing are still essential. Some people use PrEP (like Yeztugo) along with other prevention tools - that’s the smartest approach.
What if you miss your injection appointment?
If you’re more than a few weeks late, your viral load could rise. Contact your provider immediately. They may ask you to resume oral medication temporarily while scheduling your next shot. Missing one dose doesn’t mean failure - but it does mean you need to act fast. Programs with reminder texts or phone calls reduce missed appointments by over 15%.
Are there any long-term side effects of lenacapavir?
So far, no major long-term side effects have been found in trials lasting up to five years. The most common issue is mild injection-site reactions. Unlike older drugs, lenacapavir doesn’t affect kidney function or bone density - which is a big win for long-term health. Ongoing studies are tracking heart health, liver function, and immune response over time.
Can children or pregnant people use long-acting HIV treatments?
Currently, lenacapavir is approved only for adults. Clinical trials for adolescents and pregnant people are underway and expected to report results in 2026. For now, standard daily regimens remain the standard for these groups. Always talk to your provider - many safe options exist for pregnancy and pediatric care.



rob lafata
Let me tell you something, folks - this whole 'long-acting injection' thing is just Big Pharma’s way of making you dependent on clinics instead of your own damn discipline. They don’t care if you live or die, they care if you keep coming back for your $45k shot every six months. And don’t get me started on how they’re pushing this as some kind of 'freedom' - it’s a leash with a fancy name. You think you’re free? Nah. You’re just a walking ATM with a needle mark.
Matthew McCraney
wait… so u mean to tell me they’re injecting us with some kinda nanotech that stays in our blood for 6 months?? lol no way. this is a government mind control thing. i read on a forum that the FDA is working with the illuminati to track people via their HIV meds. they’re using the capsid inhibitor to implant microchips. u think the 'mild pain' is just from the needle? think again. that’s the chip activating. they’re building a database of every HIV+ person on earth. and they’re calling it 'freedom' 😭
serge jane
It’s fascinating how we’ve gone from treating HIV as a moral failing to treating it as a medical condition to now treating it as a lifestyle upgrade. We used to stigmatize people for having it, then we medicated them, now we’re giving them a six-month injection that lets them forget they’re even sick. That’s not just science - that’s a philosophical shift in how we define personhood. If your illness no longer defines your daily rhythm, then what does? The injection doesn’t just suppress the virus - it suppresses the identity of being a patient. And maybe that’s the real breakthrough. Not the drug. The silence.
Nick Naylor
The U.S. healthcare system is the only one in the developed world that allows pharmaceutical monopolies to charge 2,800% markup on life-saving medications - and yet, somehow, we’re supposed to be grateful for 'innovation'? The fact that lenacapavir costs $45,000 annually - while the marginal cost of production is $25 - is not a market failure. It is a crime. And the WHO’s new directive to empower community health workers? Finally - a policy that doesn’t require a corporate lobbyist to draft it. But don’t expect the FDA to approve generics until 2035. They’re still busy approving new flavors of Viagra.
Brianna Groleau
I just want to say - I have a cousin who’s been living with HIV since 2008. She used to cry every morning because she had to hide her pills in her lunchbox at work. Now? She goes to her clinic in June and December. She travels to Japan last year. She didn’t panic when her flight got delayed. She didn’t have to explain to her boss why she needed a 10-minute break every day. She just… lived. And I watched her become a person again, not a patient. I cried when she told me about it. Not because she’s sick - but because she finally got to breathe. This isn’t just medicine. It’s a second chance at being ordinary. And that’s the most beautiful thing I’ve seen in years.
Rusty Thomas
OMG I just saw this on TikTok and I had to comment. I’m 24 and I just started dating someone who’s HIV+ and they’re on the injection thing?? I was like WAIT - does that mean we can like… kiss?? And like… have sex?? Without condoms?? I mean I know U=U is a thing but I’m still scared. Also I just Googled ‘lenacapavir side effects’ and someone said it can cause ‘emotional detachment’ - is that real?? Also I’m crying right now because I just realized how much I don’t know about this and I feel like such a terrible person for being scared. 😭😭😭
Sarah Swiatek
Let’s be real - the whole 'freedom' narrative is a little too polished. Yes, the injections are amazing. Yes, they reduce anxiety. But let’s not pretend this is some kind of universal win. The people who get this treatment? They’re the ones with insurance, transportation, time off work, and a doctor who doesn’t think HIV is 'someone else’s problem.' Meanwhile, in rural Alabama or the Mississippi Delta, someone’s still choosing between rent and their tenofovir. The real innovation isn’t the capsid inhibitor - it’s the fact that we’re still talking about this like it’s a luxury upgrade instead of a basic human right. And the fact that Gilead made $13 billion last year while people in Uganda still die because they can’t get a pill? That’s not a market. That’s a massacre dressed in clinical trial results.
Dave Wooldridge
They say the injection suppresses the virus - but what if it’s just hiding it? What if the virus is still there, just… dormant? Waiting? Like a sleeper agent? And what if the next strain evolves to bypass the capsid inhibitor? What if this is all a trap? They’re testing it on us so they can weaponize it later. I heard from a guy who works at a CDC lab - they’re already building a strain that only responds to the injection. So if you’re not on it? You’re a target. That’s why they’re pushing it so hard. It’s not medicine. It’s control. And the 'mild pain'? That’s the virus being reprogrammed. I’m not taking it. I’m going back to the pills. At least I know what I’m fighting.
Rebecca Cosenza
I’m not taking the shot. Too many unknowns. Pills are safe. I’ve been on them for 15 years. I don’t need a new trend.