How to Prevent and Treat Yeast Infections Caused by Antibiotics

Yeast Infection Risk Calculator
This tool helps you assess your risk of developing a yeast infection after taking antibiotics. Enter your risk factors to get personalized prevention recommendations based on the latest medical guidelines.
When you take antibiotics, you’re fighting bad bacteria. But sometimes, you end up with a whole new problem: a yeast infection. It’s not rare - up to 30% of people with vaginas get one after antibiotics. The itching, burning, and thick white discharge can feel like a punishment for taking medicine meant to help you. The truth? It’s not your fault. It’s a side effect of how antibiotics work - and it’s completely preventable.
Why Antibiotics Cause Yeast Infections
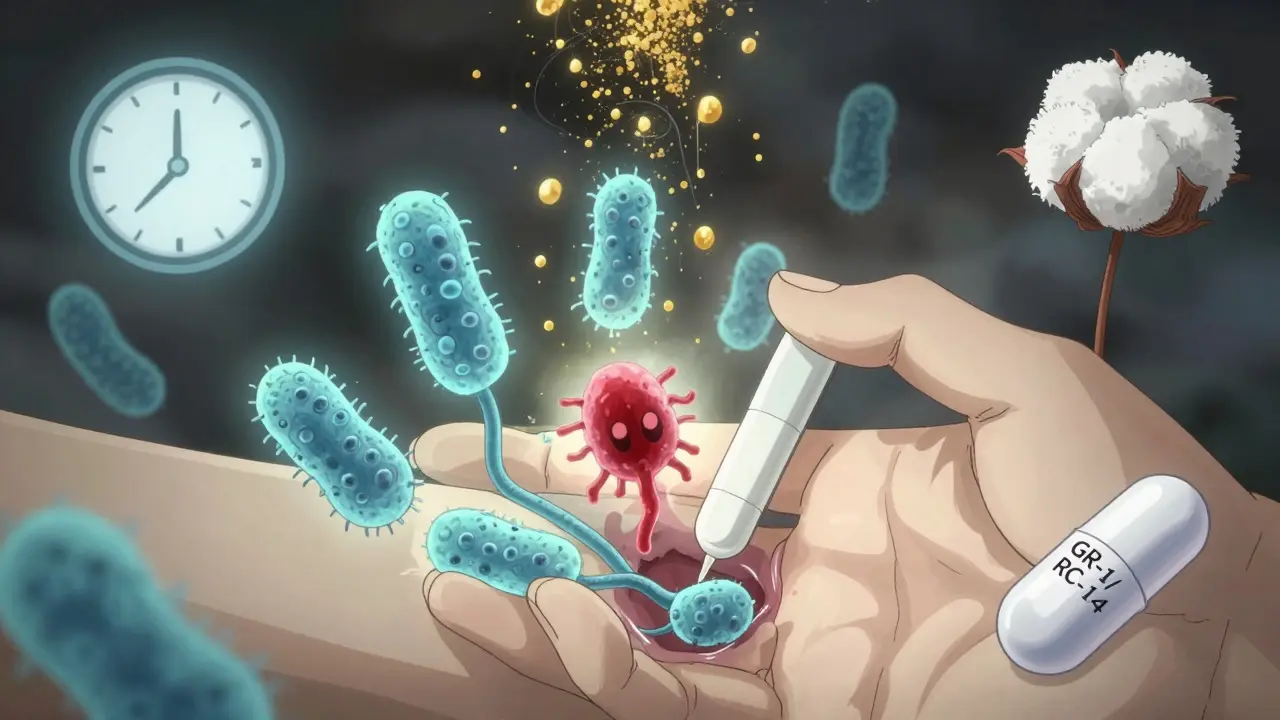
Your body isn’t just made up of you - it’s also home to trillions of tiny organisms, mostly bacteria. In the vagina, a healthy balance means lots of Lactobacillus bacteria. These good bugs keep things acidic (pH 3.8-4.5), which stops yeast like Candida albicans from taking over. When you take broad-spectrum antibiotics like amoxicillin, doxycycline, or ciprofloxacin, they don’t just kill the bad bacteria. They wipe out the good ones too. Without those protective bacteria, yeast grows unchecked. It’s not the antibiotic itself causing the infection - it’s what it removes.Who’s Most at Risk?
Not everyone gets a yeast infection after antibiotics. Some people never do. Others get them every time. Why? It’s about your body’s setup. If you have:- Uncontrolled diabetes (blood sugar over 180 mg/dL),
- High estrogen levels (from pregnancy, birth control pills, or hormone therapy),
- A weakened immune system (like HIV with CD4 count under 200),
- Or you’re taking SGLT2 inhibitors like Jardiance (which dump sugar into your urine),
your risk goes way up. So do habits like douching (which strips away protective bacteria), wearing tight synthetic underwear (traps heat and moisture), or using scented soaps and sprays (they throw off your pH by 1.5-2.0 units). Cotton underwear? It keeps your vaginal temperature 2-4°C lower than synthetics - and that’s enough to cut yeast growth in half.
How to Prevent It Before It Starts
The best time to stop a yeast infection is before it begins. Here’s what actually works, backed by clinical data:- Start an antifungal on day one of your antibiotics. Use an over-the-counter cream or suppository like clotrimazole (Gyne-Lotrimin) or miconazole (Monistat). A 7-day course is 15% more effective than a single dose. Start it the same day you take your first antibiotic pill - don’t wait for symptoms.
- Take the right probiotics. Not all probiotics are equal. Look for strains that actually survive in the vagina: Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14. Products like Fem-Dophilus contain these. Take 10 billion CFU daily, and space them 2 hours apart from your antibiotic. Studies show this cuts infection risk by half.
- Watch your sugar. Yeast feeds on sugar. Cut out white bread, candy, soda, and even fruit juices. Simple carbs break down into glucose, which your body excretes in urine - and that sugar can leak into the vaginal area. One study showed cutting sugar reduced yeast recurrence by 20%. It’s not a magic cure, but it helps.
- Ditch the douches and scented products. Douching removes 70-90% of your good bacteria. Scented tampons, sprays, and washes? They’re not cleaning you - they’re disrupting your natural ecosystem. Water and plain soap are enough.
- Wear cotton underwear. Synthetic fabrics trap heat and sweat. Cotton lets air move. It’s simple, cheap, and backed by microbiology studies showing it lowers vaginal temperature enough to slow yeast growth by 50%.
People who combine at least two of these methods - say, probiotics plus antifungals - have an 78% success rate in avoiding infection. Those who use only one? Only 45%.
What to Do If You Already Have Symptoms
If you’re already itching, burning, or noticing thick white discharge that looks like cottage cheese, don’t panic. But also don’t assume it’s yeast. About 64% of self-diagnosed yeast infections turn out to be something else - like bacterial vaginosis or a sexually transmitted infection. If you’ve never had one before, see a provider. They can do a quick test.If you’ve had yeast infections before and recognize the symptoms:
- Use an OTC antifungal cream or suppository. Butoconazole (Gynazole-1) or clotrimazole work well. Most clear up in 5-7 days.
- If it’s your fourth infection in a year, or it’s not going away after a week, you need a prescription. Fluconazole (Diflucan), one pill, is 95% effective for stubborn cases - but only if you’re not pregnant.
Here’s the catch: Fluconazole is risky during pregnancy. The FDA warns it can increase the chance of birth defects by 4.5 times in the second and third trimesters. If you’re pregnant and have a yeast infection, your doctor will likely recommend boric acid suppositories (600mg nightly for 14 days). They work on non-albicans strains that don’t respond to regular antifungals.
What Doesn’t Work (and Makes Things Worse)
There’s a lot of misinformation out there. Here’s what to avoid:- More antibiotics. You can’t treat a fungal infection with a bacterial drug. Taking more antibiotics just kills more good bacteria and makes the yeast grow stronger. About 22% of people try this - and end up with worse symptoms.
- Yogurt in the vagina. Eating yogurt with live cultures helps, but putting it inside? It doesn’t work. The strains in yogurt (like L. acidophilus) don’t stick around in the vagina. Plus, it can introduce unwanted sugars and bacteria.
- “Candida diets” alone. Cutting sugar helps, but it’s not enough. One review in JAMA Dermatology found strict diets only reduced recurrence by 15-20%. Combine it with probiotics and antifungals - don’t rely on diet alone.
- Waiting to treat. The longer you wait, the worse it gets. Symptoms can escalate from mild itching to painful sores and swelling. Start treatment early, even if you’re unsure.

What’s Changing in Medicine
For years, doctors didn’t talk about this. They treated the infection after it happened - rarely prevented it. But things are shifting. The CDC now includes vaginal health in its antimicrobial stewardship guidelines. New 2024 updates are expected to recommend prevention for high-risk patients. In Europe, some guidelines already suggest fluconazole prophylaxis during antibiotics. In the U.S., we’re still catching up.Why? Because vaginal health research gets only 2.5% of the NIH’s $42.9 billion budget - despite affecting 1.4 billion people globally. That’s why you won’t find official prevention guidelines yet. But that’s changing. Clinical trials are underway for vaginal microbiome transplants and pH-regulating tampons. These could be game-changers - but they’re still years away.
For now, the tools you need are already here: antifungals, probiotics, cotton underwear, and avoiding sugar. You don’t need a miracle. You need to act before the infection starts.
Real People, Real Results
On Reddit, over 1,200 people shared their experiences. 68% said using Monistat daily during antibiotics stopped their yeast infection. But 42% said the suppositories irritated them. Others switched to creams - and had fewer issues. On Amazon, Culturelle Women’s Healthy Balance has 4.3 stars from over 2,000 reviews. But 31% said it took two weeks to notice a difference. That’s normal. Probiotics need time to rebuild your microbiome.Fluconazole gets a 6.7/10 rating. Some people swear by it. Others got headaches or nausea. A few had liver enzyme changes - rare, but real. The best approach? Start with OTC antifungals and probiotics. Only turn to fluconazole if it doesn’t clear up.
One woman in a Mayo Clinic forum said: “I started clotrimazole and Fem-Dophilus on day one of my antibiotics. No infection. No itch. No stress. I wish I’d known this five years ago.”
Can antibiotics cause yeast infections in men?
Yes, but it’s less common. Men can get penile yeast infections after antibiotics, especially if they have diabetes, are overweight, or have unprotected sex with someone who has a yeast infection. Symptoms include redness, itching, and a white, clumpy discharge under the foreskin. Treatment is the same: antifungal creams like clotrimazole. Probiotics and avoiding sugar help prevent it too.
How long after antibiotics can a yeast infection develop?
It can start as early as 2-3 days after beginning antibiotics, but most appear within 5-10 days. That’s when the good bacteria are most depleted and yeast has had time to multiply. Don’t wait until you’re in pain to act - prevention works best when started immediately with your antibiotic course.
Can I take probiotics while on antibiotics?
Yes - and you should. But timing matters. Take probiotics at least 2 hours before or after your antibiotic. That gives the live cultures time to survive without being killed by the antibiotic. Use strains proven for vaginal health: Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14. Take 10 billion CFU daily.
Is yogurt enough to prevent yeast infections?
Eating yogurt with live cultures may help a little - especially if it has Lactobacillus acidophilus. But it’s not enough on its own. The strains in yogurt don’t colonize the vagina well. Studies show a 35% relative risk reduction with daily yogurt, but that’s far less than the 50% reduction seen with targeted probiotic supplements. Use yogurt as a supplement, not your main defense.
When should I see a doctor for a yeast infection?
See a provider if: it’s your first time, symptoms don’t improve in 7 days, you’re pregnant, you have fever or pelvic pain, or you get four or more infections a year. Self-diagnosis is wrong 64% of the time - what feels like yeast could be bacterial vaginosis, trichomoniasis, or even a skin condition. A quick test can save you from wrong treatment and lasting discomfort.
Can I use antifungals while on antibiotics?
Yes, and you should. Antifungals don’t interfere with antibiotics. In fact, starting them together reduces your infection risk by 60-70%. Use a 7-day cream or suppository. Don’t wait for symptoms. Begin on the same day you start your antibiotic. This proactive approach cuts severe infections by 82% compared to waiting.
Antibiotics save lives. But they also disrupt the quiet, invisible world inside your body. You don’t have to accept yeast infections as a normal side effect. With the right steps - started early - you can protect yourself. It’s not about avoiding antibiotics. It’s about protecting your body while you use them.



Christina Bischof
I’ve had yeast infections after antibiotics three times. Cotton underwear and probiotics changed everything. No more stress. Just peace.
Lisa Davies
This is the best guide I’ve ever read 🙌 I started using Fem-Dophilus with my last course of amoxicillin and zero symptoms. Thank you for sharing this 💕
RONALD Randolph
This article is scientifically accurate, meticulously researched, and long overdue. The CDC’s failure to mandate prophylaxis for high-risk patients is a national disgrace.
Mike Nordby
I appreciate the emphasis on microbiome preservation. The data on L. rhamnosus GR-1 and L. reuteri RC-14 is compelling. However, I’m curious whether the studies controlled for dietary fiber intake, which may independently modulate vaginal pH.
Jocelyn Lachapelle
You’re not broken if this happens to you. You’re just human. And now you know how to fight back. Keep going. You’ve got this. 💪
Nupur Vimal
In India we just use neem water wash and dont care about probiotics. This western overcomplication is unnecessary
Cassie Henriques
The microbiome modulation here aligns with recent findings in mucosal immunology-particularly the role of SCFA production by Lactobacilli in suppressing Candida hyphal transition. The 7-day antifungal protocol is critical for biofilm disruption.
Jake Sinatra
This is exactly the kind of patient-centered, evidence-based guidance that’s missing from most clinical guidelines. Thank you for making this accessible. I’ve shared it with my entire family.
John Samuel
I’ve spent decades in clinical research, and this is one of the clearest, most beautifully articulated summaries I’ve seen on vaginal microbiome dynamics. The inclusion of real-world Reddit data adds invaluable context. Kudos. 🌟
Raj Kumar
i used yogurt and it didnt work but then i tried the probiotics from the article and wow. so simple. why do docs never tell us this?
Benjamin Glover
Fascinating. Though one must wonder: is this merely a symptom of overmedicalization? In the UK, we rarely treat asymptomatic candida. The obsession with ‘prevention’ feels almost obsessive.
Sai Nguyen
Americans always overthink everything. Just take the pill. Stop whining.