How to Read Pharmacy Allergy Alerts and What They Mean
When you pick up a prescription at the pharmacy, you might not notice the quiet beep or pop-up on the pharmacist’s screen. But that alert? It could be the only thing standing between you and a dangerous reaction. Pharmacy allergy alerts are built into nearly every electronic health record system today - Epic, Cerner, Allscripts - and they’re designed to stop the wrong drug from being given to the wrong person. But here’s the problem: most of them are wrong.
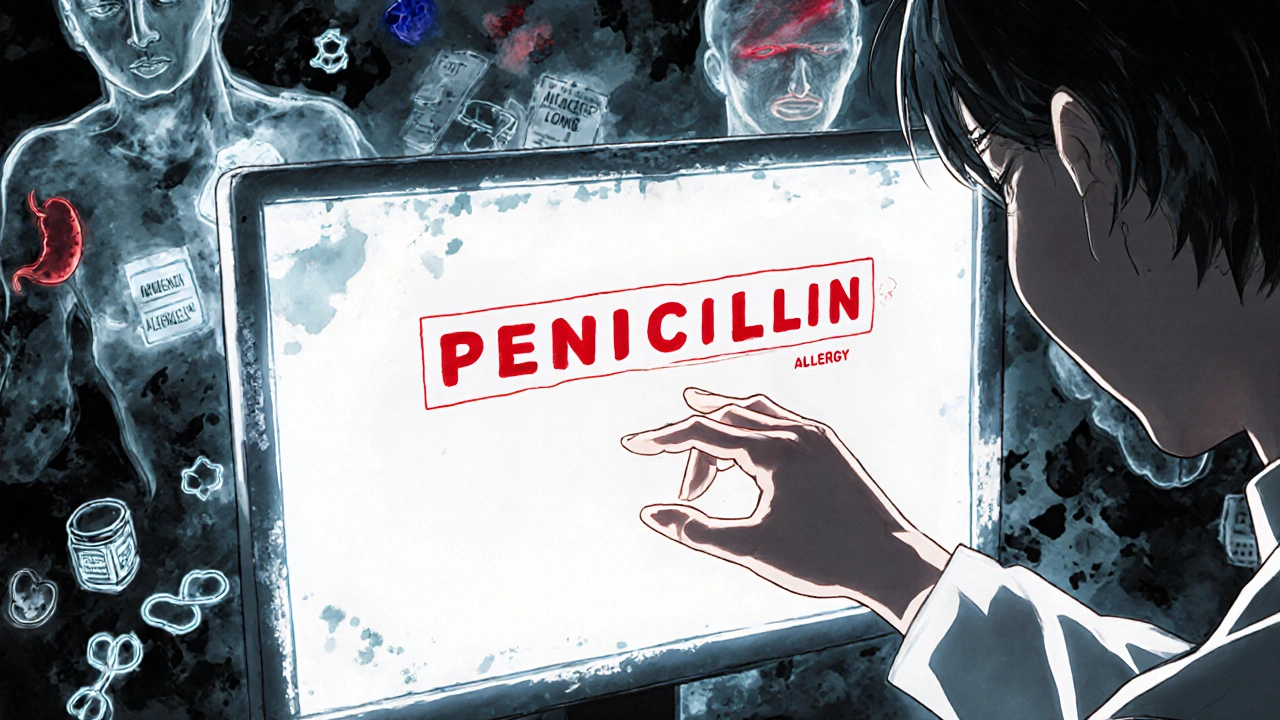
What You’re Actually Seeing When an Alert Pops Up
Pharmacy allergy alerts aren’t magic. They’re automated comparisons between what the doctor ordered and what’s written in your medical record. If your chart says "penicillin allergy," and the pharmacist tries to fill amoxicillin, the system flags it. Simple, right? Not quite. These systems use databases like First DataBank to map drug classes. So if you’re allergic to penicillin, the system might also warn you about ampicillin, cephalosporins, or even some NSAIDs - even if you’ve taken them safely for years. That’s because the software doesn’t know the difference between a real allergy and a side effect. It just sees a match. There are two kinds of alerts you’ll see:- Definite allergy alert: The drug you’re being given is in the same class as something you’ve been documented as allergic to.
- Possible allergy alert: The system thinks there’s a chance of cross-reactivity - like linking penicillin to a third-generation cephalosporin.
Why So Many Alerts Are Useless - And Dangerous
In 2023, a study of over 1.2 million alerts across U.S. hospitals found that 78% were triggered by reactions that weren’t true allergies at all. Think of it: a patient writes down "I got sick after taking ibuprofen" - meaning they had a stomachache. The system logs it as "ibuprofen allergy." Now every time someone tries to give them naproxen, ketoprofen, or celecoxib, the alarm goes off. But NSAID allergies? Less than 1% of cases are immune-mediated. The rest are just side effects. The same goes for penicillin. About 10% of Americans say they’re allergic. But when tested properly, 90% of them aren’t. Yet systems treat every "penicillin allergy" as if it’s a ticking bomb. That’s why clinicians override these alerts so often - 95% of the time, according to one 2020 study. And when you override alerts constantly, you start ignoring them. Even the real ones. Worse, many systems don’t even ask for details. They just say "allergy." No date. No symptoms. No severity. So if you had a rash after amoxicillin at age 8, the system treats it the same as someone who went into anaphylactic shock after penicillin last year. That’s not smart. That’s dangerous.
How to Read the Alert - Step by Step
When you see an alert, don’t just click "OK." Pause. Ask these questions:- What was the reaction? Was it a rash? Hives? Swelling? Trouble breathing? Or just nausea, diarrhea, or dizziness? Only immune reactions - like hives, swelling, or anaphylaxis - count as true allergies.
- When did it happen? True allergic reactions happen within minutes to hours after taking the drug. If you had a stomachache two days later? Probably not an allergy.
- Was it documented by a doctor? If it’s just something you told a receptionist ten years ago, it might not be accurate. Ask if it was confirmed by an allergist.
- What drug class is being flagged? Is it a direct match? Or is it a "related" drug? For example: amoxicillin (direct match) vs. cefdinir (cephalosporin - low risk).
- How severe is the alert? Some systems use color codes: yellow = mild, red = severe. Don’t ignore a red alert. But also don’t assume a yellow alert means you’re at risk.
What You Can Do to Fix Your Own Allergy Record
You’re not powerless. Your allergy record is yours to update. Start by reviewing your chart. Go to your patient portal or call your doctor’s office and ask: "What allergies do you have on file for me?" Then ask: "Was this confirmed by testing?" If you’ve been told you’re allergic to penicillin but never had a serious reaction - or if you’ve taken it since without issue - ask about a penicillin skin test. It’s quick, safe, and covered by most insurance. If the test is negative, your allergy can be removed from your record. That alone can cut down hundreds of unnecessary alerts over your lifetime. Same goes for NSAIDs. If you got a headache after taking ibuprofen, that’s not an allergy. It’s a side effect. Ask your doctor to change it from "allergy" to "intolerance" or "adverse reaction." That way, the system won’t block you from other NSAIDs if you need them.


stephanie Hill
Okay but have you ever noticed how the pharmacy alert just goes *beep* and the pharmacist sighs like you're asking for a unicorn? I once got flagged for ibuprofen because I threw up after a concert in 2012. Turns out it was tequila. Not the drug. The system didn't care. I swear, if I sneeze near a pill, it'll lock my whole medical record down.
Akash Chopda
They track your DNA now too they just dont tell you
Jessica okie
The system doesn't care if you're allergic to penicillin or just allergic to bad decisions. It doesn't know the difference between a rash and a tantrum. Your chart is a dumpster fire labeled 'medical history' and the algorithm is just trying not to drown in it.
Benjamin Mills
I had a pharmacist yell at me because I said 'I think I'm allergic to aspirin' when I was 12 and got a stomach ache. Now I can't take Advil without a 15-minute consultation. I swear they're just trying to make us feel guilty for existing.
Craig Haskell
It's a classic case of algorithmic overfitting in clinical decision support systems - the model has been trained on noisy, unstructured, and often anecdotal patient-reported data, leading to catastrophic false positive rates. The lack of temporal, contextual, and severity metadata in allergy fields creates a pathological signal-to-noise ratio. We're not just dealing with bad UI - we're dealing with epistemological collapse in EHR design.
And yet, when you push back, the system just says 'allergy' in bold red. No context. No nuance. Just fear.
Ben Saejun
My grandma had a rash after amoxicillin at age 6. Now at 82, every time she needs antibiotics, the system screams like a fire alarm. She’s had 17 different meds blocked because of a 1957 incident. Meanwhile, the real danger - polypharmacy, kidney damage, drug interactions - goes unmarked. The system is scared of ghosts.
And we wonder why people stop listening.
Visvesvaran Subramanian
Doctors write what they hear. Patients say what they feel. Systems believe both. That is the problem.
Christy Devall
They call it an 'allergy alert' like it's a warning from the gods. But it's just a spreadsheet that got drunk and started guessing. I once got flagged for codeine because I cried during a Pixar movie. The system thought I was allergic to sadness. I’m not even kidding.
Selvi Vetrivel
So let me get this straight - if you sneezed after a drug in 2008, you're now banned from 47 medications for life? And the system won't even let you say 'I think I'm fine'? How is this not a dystopian sitcom? I'd rather get the flu than fight this.
Nick Ness
It is imperative that patients engage in proactive reconciliation of their allergy documentation with their primary care provider. Structured data entry, as mandated by the 21st Century Cures Act, significantly reduces ambiguity. Furthermore, referral to an allergist-immunologist for formal challenge testing is the gold standard for de-labeling false-positive allergies.
Failure to do so perpetuates suboptimal therapeutic outcomes and increases antimicrobial resistance.
Rahul danve
The system is run by robots who hate humans. Also, NSAIDs are a CIA plot. 🤖💊
Abbigael Wilson
Oh darling, this isn't just a technical failure - it's a cultural one. We've outsourced our medical intuition to a machine that doesn't know what a 'mild rash' feels like. It doesn't understand grief, or trauma, or the fact that people lie to doctors because they're tired of being judged. This isn't bad code - it's bad humanity.
Katie Mallett
If you're unsure about your allergy record, just call your doctor's office. Say, 'Hi, I'd like to review my allergy list - can you confirm what's in there and whether it was tested?' Most offices will send you a portal link. Takes five minutes. Could save you from being denied life-saving meds later.
You're not being annoying. You're being smart.
Joyce Messias
My sister got her penicillin allergy removed after a skin test. Now she gets antibiotics faster than anyone in the ER. They even gave her a sticker. I cried. You can fix this. Just ask. Please.
Wendy Noellette
Per the Office of the National Coordinator for Health IT (ONC) guidelines, structured allergy documentation must include: reaction type, date of reaction, and verification status. Failure to comply with these standards constitutes a breach of the Meaningful Use criteria under the Medicare and Medicaid EHR Incentive Programs.
Patients are encouraged to request documentation review in accordance with 45 CFR § 164.524.