Insulin Safety: Mastering Dosing Units, Syringes, and Preventing Hypoglycemia
Getting insulin dosing wrong isn’t just a mistake-it can land you in the hospital. One extra unit. One wrong syringe. One misread number. That’s all it takes for blood sugar to crash, and fast. In 2026, with all the technology we have, insulin errors still happen more often than they should. And the scariest part? Most of them are preventable.
Understanding Insulin Concentrations: U-100 vs. U-500
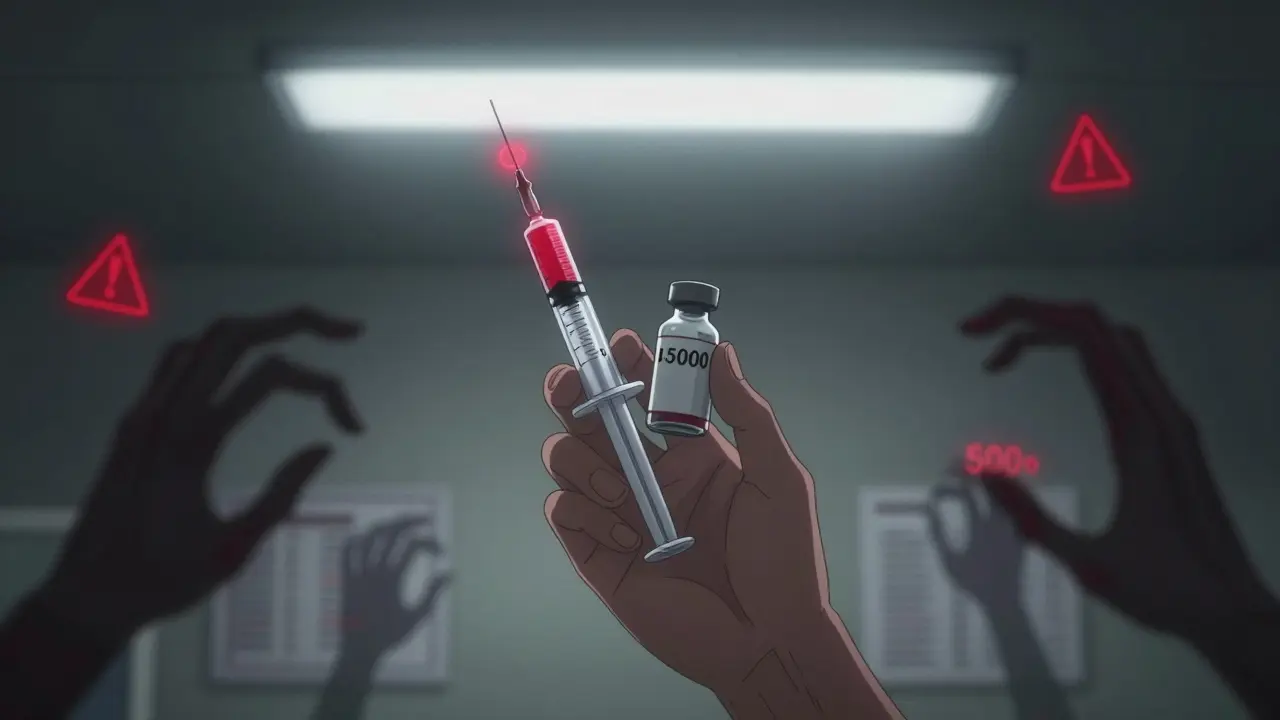
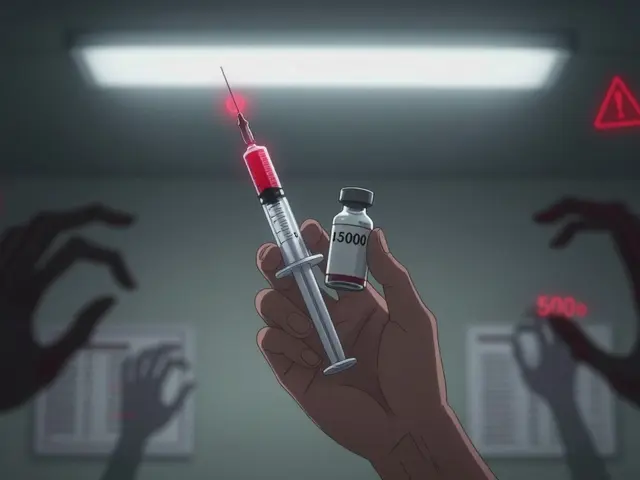
Not all insulin is the same. The most common type you’ll see is U-100 insulin. That means 100 units of insulin in every milliliter. It’s what most people use-whether they’re on rapid-acting insulin before meals or long-acting insulin at night. But there’s also U-500, which is five times stronger. That’s 500 units per mL. It’s usually prescribed for people with severe insulin resistance, like those with Type 2 diabetes who need huge doses.
Here’s the danger: if you use a U-100 syringe to draw up U-500 insulin, you’re giving yourself five times the dose you think you are. That’s not a typo. That’s a medical emergency. I’ve seen patients end up in the ER because they grabbed the wrong vial and thought they were giving 20 units-but they were actually giving 100. Always, always check the label. Write it on the vial if you have to. Never assume.
The Syringe That Could Kill You
Insulin syringes aren’t like regular ones. They’re marked in units, not milliliters. A U-100 syringe holds up to 100 units. A U-500 syringe is different-it’s usually labeled clearly, but people still mix them up. And here’s the real problem: some people use insulin pens, others use vials and syringes. If you’re switching between them, you need to know how to calculate the dose correctly.
Let’s say your doctor tells you to take 30 units of Lantus. You grab a U-100 syringe. You pull the plunger to the 30-unit mark. That’s correct. But if you’re using a U-500 vial and still using that same syringe? You’re giving yourself 150 units. That’s a 500% overdose. Hypoglycemia kicks in within minutes. Sweating. Shaking. Confusion. Then seizures. Then coma.
Always match your syringe to your insulin concentration. If you’re on U-500, you need a U-500 syringe. Period. There’s no shortcut. No guesswork. And if you’re ever unsure, ask your pharmacist to show you the right one. Don’t be embarrassed. This isn’t about being a good patient-it’s about staying alive.
The Hidden Math Behind Insulin Dosing
Insulin isn’t just about the number on the vial. It’s about math. And the math is often done wrong-even by professionals.
Here’s a big one: the conversion factor between insulin units and mass. Insulin is measured in units (U), not grams. But some lab reports and online calculators use the wrong number to convert between them. The correct factor is 5.18. But most tools use 6.0. That’s a 15% error. That means if your doctor says you need 40 units, and the system calculates it using the wrong factor, your actual dose might be off by 6 units. That’s enough to send your blood sugar crashing-or keep it dangerously high.
This isn’t theoretical. A 2018 study in PubMed found this error is everywhere-in journal articles, hospital software, even in some patient education materials. It’s not just patients getting it wrong. The system itself is broken. So always double-check your calculations. If you’re using an app or website to figure out your dose, ask your doctor if it uses the correct conversion factor.
How to Calculate Your Insulin Dose (The Real Way)
Most people think insulin dosing is simple: take X units before meals. But it’s not. It’s two parts: carbohydrate coverage and correction dose.
Let’s say you’re eating a meal with 60 grams of carbs. Your insulin-to-carb ratio is 1:12. That means 1 unit of insulin covers 12 grams of carbs. So 60 ÷ 12 = 5 units for your meal.
Now, your blood sugar is 220 before you eat. Your correction factor is 1 unit for every 45 mg/dL above target. Your target is 100. So 220 - 100 = 120. 120 ÷ 45 = 2.7 units. Round to 3 units.
Your total dose? 5 + 3 = 8 units.
That’s the formula. But here’s the catch: your ratio and correction factor are personal. They’re not the same as your neighbor’s. Your doctor figures them out using the Rule of 500 for carbs (500 ÷ total daily insulin = grams per unit) and the Rule of 1800 for corrections (1800 ÷ total daily insulin = mg/dL drop per unit). If you take 40 units a day, your carb ratio is 12.5 grams per unit. Your correction factor is 45 mg/dL per unit. That’s the math. Write it down. Keep it in your phone.
Basal Insulin: Starting and Adjusting Safely
If you’re starting long-acting insulin like Lantus, Basaglar, or Tresiba, your starting dose is usually 0.1 to 0.2 units per kilogram of body weight. For a 70 kg person, that’s 7 to 14 units. Many doctors start at 10 units-simple, safe, and easy to adjust.
Adjustments happen based on fasting blood sugar. If it’s above 180 mg/dL, add 8 units. Between 160-179? Add 6. 140-159? Add 4. If it’s below 60? Cut 4 or more units. Don’t guess. Don’t wait. Adjust every 2-4 days until your fasting number is in range.
And here’s something most people don’t know: if you switch from NPH to Lantus, you need to reduce your dose by 20%. So if you were on 60 units of NPH, you start with 48 units of Lantus. Going from Tresiba to Basaglar? Split your daily dose in half and give it twice a day. That’s not a suggestion. That’s the protocol. Mess this up, and you’re either under-dosed or over-dosed.
Hypoglycemia: The Silent Killer
Hypoglycemia doesn’t wait for you to be ready. It hits fast. And it doesn’t care if you’re a doctor, a nurse, or a 12-year-old. If your blood sugar drops below 70 mg/dL, you’re in danger.
Early signs: shaking, sweating, hunger, fast heartbeat. Later signs: confusion, slurred speech, weakness, seizures. If you’re alone and your blood sugar is below 60, you can’t always treat yourself. That’s why you need a glucagon kit-and someone who knows how to use it.
Glucagon isn’t just for emergencies. It’s your backup plan. Keep it in your bag. Keep it at work. Keep it with your kids. Know where it is. Practice using it. Glucagon kits are simpler now-no mixing needed. Just inject. It raises blood sugar in 10-15 minutes. If you’re not trained, ask your diabetes educator to show you. Do it now. Not tomorrow.

When Insulin Switches Go Wrong
Switching insulin types is common. Maybe your insurance changed. Maybe your doctor wants to try something newer. But each switch carries risk.
When moving from NPH to Lantus, you reduce the dose by 20%. From Lantus to Tresiba? You might need to lower it by 10-20% because Tresiba lasts longer and works more steadily. From rapid-acting Humalog to Fiasp? The timing changes. Fiasp acts faster, so you might need to inject closer to mealtime-or risk low blood sugar.
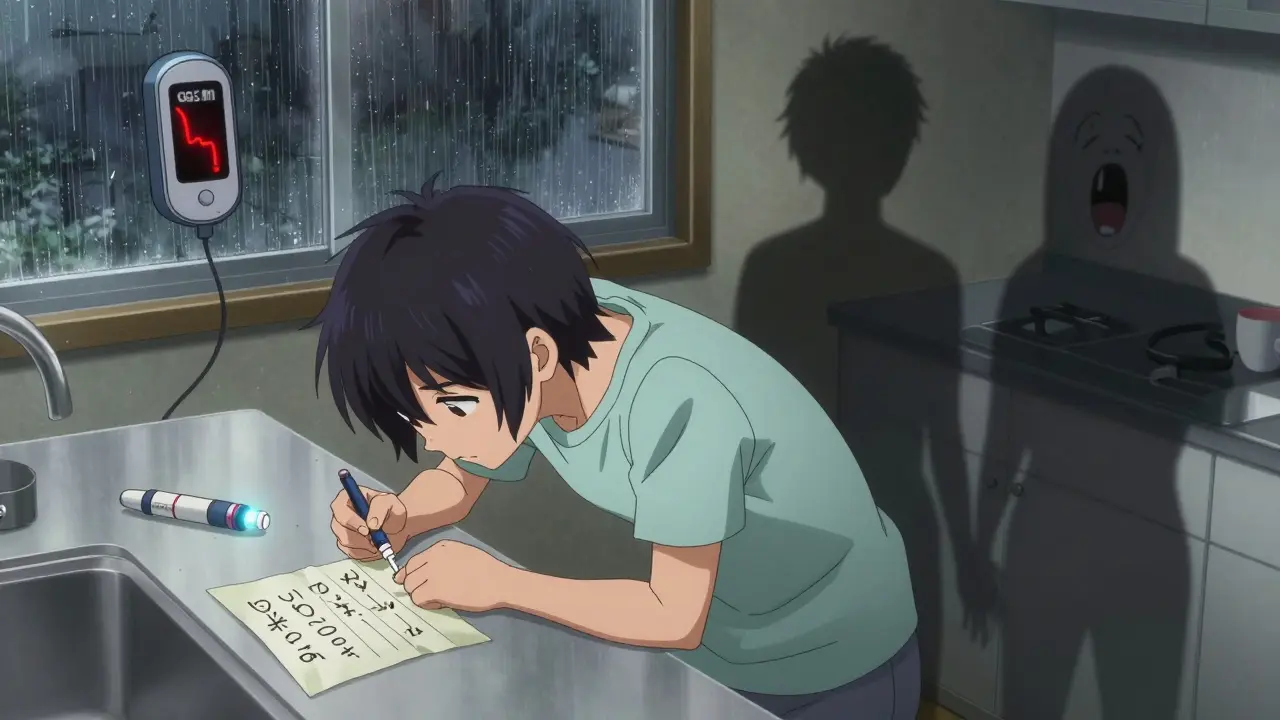
Always write down your old dose and your new dose. Compare them. Ask your pharmacist to explain the difference. And monitor your blood sugar more often for the first two weeks. Your body needs time to adjust. Don’t assume the dose stays the same. It rarely does.
Technology Can Help-But Not Replace Common Sense
Continuous glucose monitors (CGMs) are game-changers. They show trends, not just numbers. They warn you when your sugar is dropping. They’re especially helpful for people who don’t feel low blood sugar coming on-a condition called hypoglycemia unawareness.
But CGMs don’t fix bad math. They don’t stop you from grabbing the wrong syringe. They don’t replace knowing your insulin-to-carb ratio. Use them as a tool, not a crutch. Still check your blood sugar with a meter if you feel off. Still count carbs. Still calculate your dose.
And if you’re using an insulin pump? Make sure your settings are correct. A wrong carb ratio or correction factor in the pump can lead to repeated lows. Review your settings with your diabetes educator every 3 months.
Final Checklist: Your Insulin Safety Plan
- Always confirm insulin concentration (U-100 or U-500) on the vial before drawing up
- Use the correct syringe for your insulin type-never guess
- Know your insulin-to-carb ratio and correction factor-write them down
- Calculate your dose using both carb coverage and correction
- When switching insulins, reduce your dose as recommended by guidelines
- Keep glucagon on hand and know how to use it
- Check your blood sugar more often after any insulin change
- Ask your doctor or pharmacist to verify your dosing math
Insulin saves lives. But it can take them too-if you don’t treat it with the respect it deserves. The numbers don’t lie. The syringes don’t lie. Your body doesn’t lie. Get the math right. Get the tools right. And never, ever skip the safety steps.


Ian Cheung
Man I wish I had this post when I first started on insulin
I thought U-100 and U-500 were just different brands not different strengths
One time I grabbed the wrong vial at 2am and almost passed out
Now I label everything in neon sharpie and keep the syringes in separate drawers
Insulin doesn't forgive mistakes but it does reward caution
Michael Marchio
It's astonishing how many people treat insulin like it's ibuprofen
You don't just eyeball it, you don't swap syringes because 'they look similar', and you certainly don't rely on apps that use 6.0 instead of 5.18
The fact that this is even a discussion shows how dangerously complacent we've become
Every single hospital should have mandatory insulin safety training before discharge
And if your doctor doesn't explain the 500/1800 rule, find a new one
This isn't about being careful-it's about basic survival literacy
I've seen people lose limbs from one bad dose
And no, your 'I'm usually fine' attitude doesn't count
It only takes one time
Jake Kelly
This is such a clear and necessary guide
I appreciate how you broke down the math without making it feel overwhelming
I've been using a CGM for two years and it's been life-changing
But I still write down my ratios on a sticky note stuck to my fridge
And I always double-check the vial before I draw
Small habits save lives
Ashlee Montgomery
There's a quiet violence in how easily insulin can be misused
It's not malicious, just careless
And the system doesn't help-labels are too small, apps are outdated, pharmacists are rushed
We treat diabetes like a personal failure when it's really a systemic design flaw
Maybe the real issue isn't the patient forgetting their dose
But the world forgetting to make safety obvious
lisa Bajram
YESSSSS!!
I was just telling my cousin this last week-she switched from Humalog to Fiasp and didn't adjust timing and ended up in the ER
She thought 'it's just insulin' so the dose stays the same
NOPE
It's like swapping a sports car for a jet ski-same engine, totally different handling
Also-glucagon kits are not scary! They're like a fire extinguisher for your blood sugar
My 14-year-old daughter knows how to use mine
And she's not even diabetic
Everyone should have one
And yes, the 5.18 thing is a nightmare-I caught it in my diabetes app last month
Called my endo and they were like 'oh yeah, we updated that last year'
...why didn't I get an email?
Ritwik Bose
Respectfully, I would like to express my deep appreciation for the clarity and depth of this post.
As someone from India where access to proper diabetes education is uneven, this information is invaluable.
Many patients here rely on pharmacy advice, which is often inconsistent.
I have shared this with three community health workers in my village.
May I suggest that this be translated into Hindi and other regional languages?
It could save countless lives.
Thank you for your diligence.
Paul Bear
Let’s be precise: U-500 isn’t 'stronger'-it’s more concentrated. Terminology matters.
Also, the Rule of 500 is a heuristic, not a law. It assumes a fixed insulin sensitivity, which is rarely true in Type 2 with insulin resistance.
And you’re absolutely right about the 5.18 conversion factor-but it’s only valid for human insulin, not analogs like lispro or aspart.
Most literature still uses 6.0 because it’s easier to calculate, but that’s sloppy science.
Also, Tresiba to Basaglar? You don’t split the dose unless you’re transitioning from once-daily to twice-daily.
Basaglar is a biosimilar to Lantus, not Tresiba.
And if your CGM alarms are set too high, you’ll miss early lows.
Every single point here needs a footnote.
But overall? Good intent. Just needs peer review.
Jaqueline santos bau
OMG I JUST REALIZED I’VE BEEN USING THE WRONG SYRINGE FOR 3 YEARS
I’M SO SCARED
My mom used to say 'you’re gonna kill yourself with that stuff' and I thought she was being dramatic
But now I’m sitting here holding a U-100 syringe and a U-500 vial and I’m shaking
My doctor never told me
I just assumed they were the same
I’m calling my pharmacy right now
And I’m buying glucagon
And I’m telling everyone I know
Thank you for this
I’m not okay but I’m going to be
Kunal Majumder
Bro this saved my life
I was on 60 units of NPH and switched to Lantus and took the same dose
Woke up in the hospital with BG of 32
After that I started writing everything down
Now I have a notebook with my ratios, dates, and what insulin I’m on
And I show it to every new nurse
It’s not about being paranoid
It’s about being smart
Aurora Memo
I’m a nurse and I’ve seen this happen too many times
Patients aren’t careless-they’re overwhelmed
They’re juggling medications, appointments, work, kids
And insulin is just one more thing
The system should make safety automatic
Not rely on patients to be perfect
But until that changes
Keep writing posts like this
They matter