Living with Herpes and Disability: Practical Guidance for Chronic Illness
Herpes and Disability Impact Calculator
Assess Your Situation
Answer the following questions to get personalized insights on managing herpes alongside your disability.
Your Personalized Assessment
Antiviral Medication Comparison
Compare key features of commonly prescribed antivirals for herpes management.
| Medication | Dosage | Cost (Monthly) | Effectiveness | Side Effects |
|---|---|---|---|---|
| Acyclovir | 400 mg 5x/day or 200 mg 3x/day | $15–$25 | ~70% reduction | Nausea, headache, mild renal impact |
| Valacyclovir | 1 g 2x/day or 500 mg once daily | $30–$45 | ~80% reduction | GI upset, dizziness, rare kidney issues |
| Famciclovir | 250 mg 3x/day or 250 mg 2x/day | $40–$55 | ~75% reduction | Headache, fatigue, occasional rash |
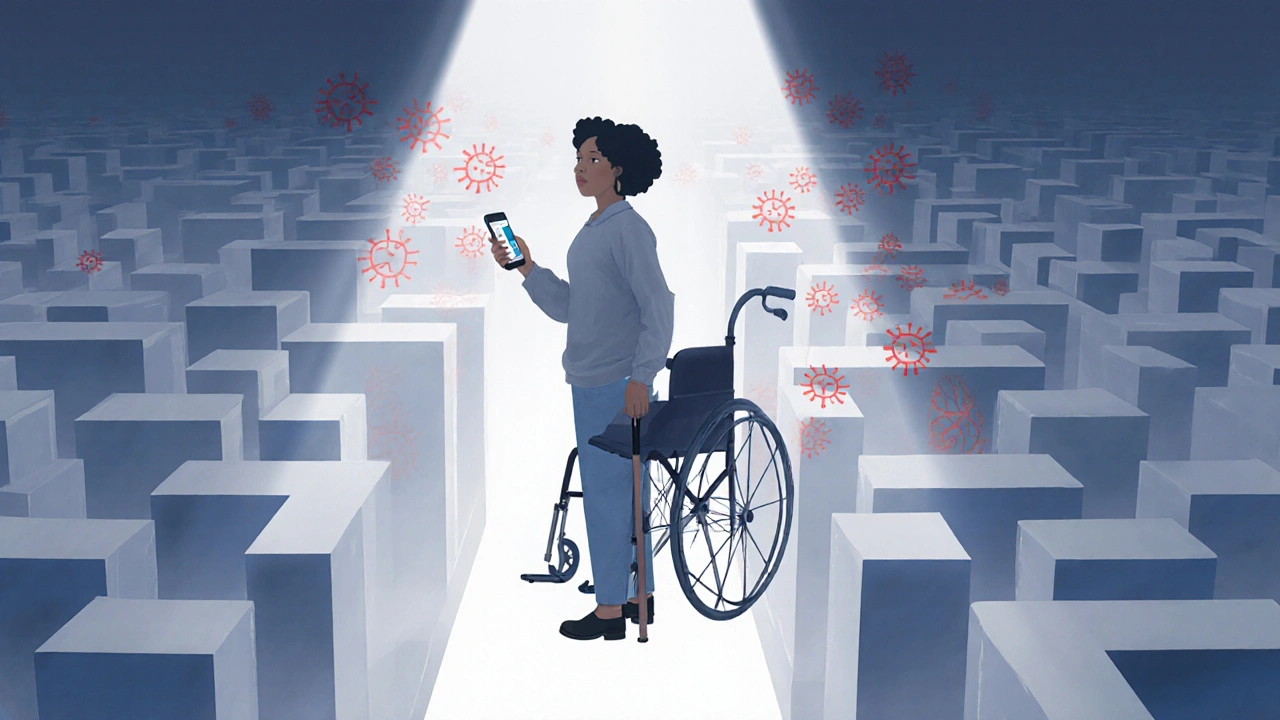
When herpes meets a disability, daily life can feel like a maze of medical, emotional, and legal obstacles. Even if you’re already navigating a chronic condition, a herpes diagnosis adds another layer of complexity-triggering flare‑ups, influencing independence, and shaping the support you need. This guide walks you through the most pressing challenges and offers concrete steps to regain control, protect your rights, and connect with the right resources.
Herpes is a viral infection caused by the herpes simplex virus (HSV), which comes in two main types: HSV‑1, typically oral, and HSV‑2, usually genital. The virus remains dormant in nerve cells and can reactivate under stress, weakened immunity, or hormonal changes, leading to painful outbreaks that can last from a few days to several weeks.
Disability refers to any physical, sensory, mental, or chronic health condition that substantially limits one or more major life activities. When a chronic illness like herpes co‑exists with another disability-such as mobility impairment, chronic fatigue, or a cognitive condition-the interplay can magnify symptoms, restrict access to care, and complicate everyday tasks.
Understanding the Interaction Between Herpes and Other Disabilities
Every body reacts differently, but several common pathways explain why herpes can feel tougher when you already live with a disability:
- Immune system strain: Many disabilities, especially autoimmune disorders, already tax the immune response. A weakened defense can make herpes reactivations more frequent and severe.
- Pain amplification: Conditions like fibromyalgia or neuropathy heighten pain perception, turning a mild outbreak into a debilitating episode.
- Medication interactions: Antivirals, pain relievers, and other prescription drugs may clash, leading to side‑effects that further limit mobility or cognition.
- Psychosocial stress: Managing a disability often involves navigating stigma. Adding a sexually transmitted infection can increase anxiety, depression, and social isolation.
Identifying which of these factors affect you is the first step toward a tailored coping plan.
Medical Management: Antiviral Treatment Comparison
Modern antivirals keep outbreaks short and reduce transmission risk. Choosing the right regimen depends on dosing convenience, cost, side‑effect profile, and how it fits with your existing medication schedule. Below is a quick side‑by‑side look at the three most prescribed options.
| Medication | Typical Dosage (Adults) | Average Monthly Cost (USD) | Effectiveness (outbreak reduction) | Common Side‑effects |
|---|---|---|---|---|
| Acyclovir | 400mg five times daily (initial) or 200mg three times daily (suppressive) | $15-$25 | ~70% reduction | Nausea, headache, mild renal impact |
| Valacyclovir | 1g twice daily (initial) or 500mg once daily (suppressive) | $30-$45 | ~80% reduction | GI upset, dizziness, rare kidney issues |
| Famciclovir | 250mg three times daily (initial) or 250mg twice daily (suppressive) | $40-$55 | ~75% reduction | Headache, fatigue, occasional rash |
For someone juggling multiple prescriptions, the once‑daily dosing of Valacyclovir often wins out for simplicity, but Acyclovir remains the most budget‑friendly. Discuss with your prescriber how each option fits into your overall medication plan.
Practical Day‑to‑Day Strategies
Beyond medication, daily habits can tilt the balance toward fewer flare‑ups and smoother functioning.
- Track triggers: Use a simple spreadsheet or a phone app to log stress levels, sleep quality, diet, and any outbreak signs. Patterns emerge quickly, especially when you have a baseline disability that already affects energy.
- Prioritize skin care: Gentle, fragrance‑free cleansers and barrier creams reduce irritation. When mobility is limited, consider adaptive tools-long‑handled sponges or seated shower chairs-to maintain hygiene without strain.
- Boost immunity: Regular, moderate exercise (e.g., seated yoga, water aerobics) improves circulation and immune resilience. Pair this with a diet rich in zinc, vitaminC, and probiotics.
- Stress‑reduction techniques: Mindfulness meditation, breathing exercises, or guided imagery can lower cortisol, a known trigger for herpes reactivation. Many organizations offer free online sessions tailored for people with physical limitations.
- Medication timing: Set alarms on a smartwatch or phone to ensure antivirals are taken at consistent intervals, even on days when fatigue makes routine difficult.

Legal Rights and Disability Accommodations
Living with dual health challenges often means navigating the legal landscape. In most countries-including NewZealand, the United States, the UK, and Australia-disability legislation protects you from discrimination and mandates reasonable accommodations in workplaces, schools, and public services.
Key steps to secure support:
- Document your condition: Obtain a formal medical statement that outlines how herpes and any co‑existing disability affect you. Include frequency of outbreaks, pain levels, and any medication side‑effects that impact work performance.
- Know your rights: In NewZealand, the Human Rights Act and the Health and Disability Services (Safety) Act require employers to provide reasonable adjustments. In the US, the Americans with Disabilities Act (ADA) does the same.
- Request accommodations: Examples include flexible work hours to manage medication schedules, remote work options during severe outbreaks, or ergonomic equipment to reduce strain.
- Engage an advocate: Disability support organisations often provide legal counsel or can connect you with occupational therapists who specialize in workplace adjustments.
Remember, you don’t have to disclose the specific diagnosis if you’re uncomfortable; a general description of a “chronic condition that requires periodic breaks” is often sufficient.
Psychosocial Support and Community Resources
The emotional toll of living with herpes and a disability can feel overwhelming, but you’re not alone. Connecting with peers who share similar experiences reduces isolation and offers practical advice.
- Online forums: Platforms like Reddit’s r/Herpes and r/Disability provide anonymity and 24/7 interaction. Look for moderated groups that enforce respectful discourse.
- Local support groups: Many hospitals and community health centers run weekly meetings for chronic illness patients. These gatherings often include a mental‑health professional who can guide coping strategies.
- Therapy options: Cognitive‑behavioral therapy (CBT) has proven effective for managing anxiety related to stigmatized conditions. Tele‑therapy services are especially convenient for those with mobility limitations.
- Education resources: Websites such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) publish up‑to‑date fact sheets on herpes transmission, treatment, and prevention.
When Outbreaks Disrupt Your Routine: A Crisis Plan
If an outbreak coincides with a crucial work deadline, a medical appointment, or a caregiving responsibility, having a ready‑made plan can keep panic at bay.
- Notify a trusted contact: Whether it’s a supervisor, family member, or roommate, let someone know you might need assistance.
- Have a “symptom kit” ready: Include antiviral tablets, a gentle pain‑relief cream, disposable gloves, and a clean towel. Store it in an easy‑to‑reach place.
- Adjust expectations: If possible, shift non‑essential tasks to a lower‑energy day. Use calendar blocks to protect recovery time.
- Seek professional help early: A quick call to your GP or tele‑health service can secure a prescription refill or recommend a stronger dose before the outbreak worsens.
- Practice self‑compassion: Remind yourself that flare‑ups are a medical event, not a personal failure. Positive self‑talk can reduce secondary stress, which in turn shortens outbreak duration.

Future Outlook: Emerging Therapies and Research
Scientists are actively pursuing a cure for herpes. While a definitive vaccine remains years away, several promising developments are worth watching:
- Therapeutic vaccines: Early‑phase trials of HSV‑2 therapeutic vaccines aim to boost the body’s specific immune response, potentially lowering recurrence rates.
- Gene‑editing approaches: CRISPR‑based techniques are being tested in animal models to excise latent HSV DNA from nerve cells.
- Long‑acting antiviral implants: Similar to contraceptive implants, these devices could release steady doses of medication for up to a year, reducing daily pill burden.
Staying informed about clinical trials-via registries like ClinicalTrials.gov-can provide early access to cutting‑edge therapies, especially for those whose current treatments offer limited relief.
Key Takeaways
- Understanding how herpes interacts with existing disabilities helps you tailor treatment and daily habits.
- Antiviral choice should balance effectiveness, cost, and compatibility with other meds; Valacyclovir often wins for convenience.
- Legal protections exist; document your condition and request reasonable accommodations early.
- Psychosocial support-online or in‑person-reduces isolation and offers practical coping ideas.
- Prepare a crisis plan for outbreak days to safeguard work, caregiving, and personal wellbeing.
Frequently Asked Questions
Can herpes be considered a disability?
If outbreaks are frequent, painful, or cause significant psychosocial distress that limits major life activities, herpes can qualify as a disability under many national laws. Documentation from a healthcare professional is essential for formal recognition.
How often should I take antiviral medication?
There are two main strategies: episodic treatment (starting meds at the first sign of an outbreak) and suppressive therapy (daily low‑dose pills). Suppressive therapy, taken every day, is recommended for people with more than four outbreaks a year or for those who need to reduce transmission risk.
What workplace accommodations are reasonable for herpes?
Common accommodations include flexible scheduling for medication timing, permission to work from home during severe flare‑ups, access to private restroom facilities, and ergonomic adjustments that reduce pain during long periods of sitting or standing.
Are there any over‑the‑counter products that help with outbreaks?
Topical anesthetics such as lidocaine creams can relieve pain, and certain zinc‑based ointments may modestly shorten healing time. However, they should complement-not replace-prescribed antivirals.
Where can I find support groups for people with both herpes and a disability?
National disability organisations often run health‑focused support circles. For example, the NewZealand Disability Action Network and the Arthritis Foundation host virtual meetings where members discuss chronic infections, including herpes. Online platforms like HealthUnlocked also have disease‑specific forums.


Stephanie Colony
Patriotic elites understand that chronic conditions demand disciplined management, not the excuse‑filled complacency you see online.
Abigail Lynch
It's obvious the pharmaceutical giants are hiding the true cure, while we, the suffering, are forced to juggle endless pills and inaccessible assistive tech as part of their grand experiment.
David McClone
Oh sure, because nothing says “freedom” like scheduling antiviral doses around a wheelchair‑accessible bathroom that somehow never exists.
Jessica Romero
Navigating the intersection of herpes virology and disability ergonomics demands a multidisciplinary framework that integrates immunological surveillance, pharmacological adherence, and adaptive occupational strategies.
First, the clinician must perform a comprehensive virological assessment, quantifying lesion frequency and correlating it with immunocompetence markers such as CD4+ counts where relevant.
Second, the disability profile-whether it pertains to mobility limitations, chronic fatigue, or cognitive load-must be mapped onto a functional capacity index that informs dosing schedules.
Third, medication selection should consider pharmacokinetic variables; for instance, valacyclovir boasts superior bioavailability that can reduce dosing frequency, a critical factor for individuals with limited dexterity.
Moreover, the cost–benefit analysis must incorporate insurance formularies, out‑of‑pocket expenses, and potential generic alternatives to avoid financial toxicity.
In parallel, assistive technologies like automated pill dispensers with voice prompts can mitigate adherence barriers caused by fine motor deficits.
Environmental modifications, such as installing low‑height shower benches and non‑slip flooring, diminish the physical strain during outbreak flare‑ups.
Psychosocial support structures, including peer support groups and tele‑health counseling, address the stigma that often compounds both conditions.
Employers should be educated on the legal obligations under the ADA, ensuring reasonable accommodations such as flexible work hours or remote work options during severe outbreaks.
Nutritional optimization, emphasizing zinc, lysine, and vitamin C intake, can subtly bolster the host immune response, though it should not replace antiviral pharmacotherapy.
Regular monitoring through digital health dashboards can provide real‑time analytics on outbreak patterns, facilitating proactive interventions.
Patients are encouraged to maintain a symptom diary, documenting lesion onset, pain scores, and any precipitating stressors to refine personalized treatment plans.
It is vital to periodically reassess renal function, especially when using high‑dose acyclovir, to preempt nephrotoxic complications.
Collaboration between neurologists, physiatrists, and infectious disease specialists yields a synergistic care model that addresses both the neurological sequelae and the virological burden.
Educational resources, such as the CDC’s herpes fact sheets and disability advocacy webinars, empower patients to make informed decisions.
Finally, fostering a culture of resilience and self‑advocacy can transform the lived experience from one of passive endurance to proactive management.
Michele Radford
Honestly, the above drivel reads like a self‑help brochure written by someone who never dealt with a real‑world disability, and it glosses over the brutal reality of systemic neglect.
Mangal DUTT Sharma
🙌 I totally get how overwhelming it can be – the constant juggling of meds 💊, appointments 📅, and accessibility hurdles 🛠️ can feel relentless, but building a solid support network and leveraging tech tools can make a huge difference 🌟.
Gracee Taylor
It really helps to view each challenge as a piece of a larger puzzle, where medical, emotional, and logistical components all need attention, and integrating them can lead to a smoother daily rhythm.
Leslie Woods
What about linking the medication schedule with the daily routine so it doesn’t become a separate task entirely
Manish Singh
I think it’s a great idea – you could set reminders on your phone or use a simple spreadsheet to keep track its not as compicated as it sounds
Dipak Pawar
From a sociocultural perspective, the stigmatization of both herpes and disability often stems from historical narratives that pathologize deviation from normative health and productivity standards, thereby marginalizing individuals who negotiate these intersecting identities; addressing this requires not only medical interventions but also community‑level dialogues that de‑construct myths and promote inclusive language, which can ultimately empower affected persons to claim agency over their health trajectories.
Jonathan Alvarenga
All this talk about cultural narratives is just fluff; the real issue is that many patients still can’t afford the latest antivirals, and your lofty discourse does nothing to fix the pricing nightmare.
Jim McDermott
Hey guys, does anyone have tips on how to talk to a doctor about needing a more accessible exam table? I feel like I always get the short end of the stick.
Naomi Ho
Start a weekly medication log use a simple notebook or phone note and mark outbreak days note any triggers and discuss patterns with your provider during checkups
Christine Watson
Great suggestion! Keeping that log not only empowers you with data but also shows your healthcare team that you’re proactive and engaged in your own care.
Macy Weaver
I’m curious how different disability accommodations, like remote work policies, actually impact outbreak frequency and overall quality of life in the long term.
James McCracken
One might argue that the true barrier isn’t the lack of accommodations but the internalized narrative that equates productivity with worth, which subtly fuels stress‑induced outbreaks regardless of external policies.
Evelyn XCII
Oh great, another ‘deep’ insight that nobody asked for, because obviously we’re all just sitting around waiting for enlightenment.
Suzanne Podany
Let’s channel that energy into concrete steps – set realistic goals, seek peer support, and remember that progress is built one small win at a time.