Lot-to-Lot Variability in Biologics and Biosimilars: What You Need to Know

Why two bottles of the same biologic drug aren’t exactly the same
If you’ve ever been told your medication is "the same" as someone else’s, but your body reacts differently, you’re not imagining things. With biologics and biosimilars, lot-to-lot variability isn’t a flaw-it’s built in. Unlike a pill made in a lab from exact chemical formulas, biologics are grown inside living cells. Those cells? They’re not robots. They’re delicate, changing, and never perfectly consistent. So every batch, or "lot," of a drug like Humira or Enbrel ends up with millions of tiny, natural differences in its structure. And that’s okay-as long as those differences don’t change how the drug works.
The U.S. Food and Drug Administration (FDA) puts it plainly: biologics contain "millions of slightly different versions of the same protein or antibody." These aren’t mistakes. They’re normal. Think of it like baking bread from the same recipe every day. The flour, yeast, and water are identical, but the oven temperature, humidity, even the baker’s hand movements-tiny things-make each loaf unique. One might rise higher. Another might brown a bit faster. But they’re still bread. Same with biologics. The protein is the same. The variations? Just part of the process.
How biosimilars are different from generics
Here’s where things get confusing. When you hear "generic," you probably think of a cheap copy of a brand-name pill-like ibuprofen. That’s a small-molecule drug. It’s made from chemicals. Every tablet is identical. That’s why generics can be approved quickly: they just prove they’re chemically the same.
Biosimilars? Not even close.
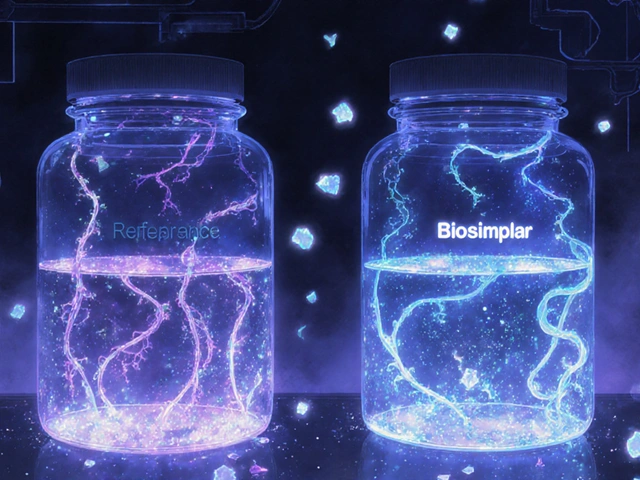
They’re not copies. They’re highly similar versions of complex biologic drugs. Because biologics are made from living cells, you can’t recreate them exactly. Even the original manufacturer can’t make two batches that are 100% identical. So the FDA doesn’t require biosimilars to be identical. They just need to prove they’re so close in structure, function, and effect that there’s no meaningful difference in safety or performance. That’s called "biosimilarity."
That’s why biosimilars go through a completely different approval path-called 351(k)-than generics, which use the simpler ANDA route. Biosimilars need dozens of lab tests, animal studies, and sometimes human trials to prove they behave like the original. It’s expensive. It’s complex. But it’s necessary.
What kinds of changes happen inside a biologic lot?
The biggest variations occur in what scientists call "post-translational modifications." That’s a fancy way of saying: after the protein is made, nature adds or tweaks little parts. The most common? Sugar molecules, or glycosylation. These sugars stick to the protein like decorations on a cake. They affect how the drug moves through your body, how long it lasts, and how strongly it binds to its target.
Other changes include:
- Missing or extra amino acids (the building blocks of proteins)
- Broken or folded protein chains
- Small chemical groups added or removed
Each lot of a biologic can contain hundreds of thousands to millions of these slightly different versions. The key isn’t eliminating them-it’s controlling them. Manufacturers use strict processes to keep those variations within a narrow, safe range. And the FDA checks every single one of those controls before approving a biosimilar.
Why this matters for patients and labs
For patients, the good news is: this variability doesn’t mean your treatment is less safe. The FDA requires that any changes between lots of the original biologic-and the biosimilar-must fall within the same range. If the reference product has a 5% variation in glycosylation from lot to lot, the biosimilar must stay within that same 5%. That’s called "comparability."
But here’s the catch: if you’re switching between a reference product and a biosimilar-or even between two different lots of the same biosimilar-your body might respond slightly differently. That’s why the FDA created a special category: interchangeable biosimilars. These are the ones that have passed extra tests to prove you can switch back and forth without increased risk or loss of effectiveness. As of May 2024, 12 out of 53 approved biosimilars in the U.S. have this designation.
For labs, this variability is a daily headache. When a new reagent lot arrives for blood tests, technicians don’t just swap it in. They run dozens of patient samples through both the old and new lots to make sure results haven’t shifted. One study found that 78% of lab directors consider lot-to-lot variation a "significant challenge." Why? Because a 0.5% change in a test like HbA1c (used to track diabetes) can mean the difference between a treatment being adjusted-or not.
How manufacturers and regulators keep things safe
It’s not luck. It’s science.
Manufacturers use advanced tools like mass spectrometry and high-throughput analytics to map out every possible variation in each lot. They track trends over time. They test for consistency in how the protein folds, how sugars attach, and how it behaves in the body. They don’t just test one or two samples. They test dozens, sometimes hundreds, per lot.
The FDA doesn’t just approve a biosimilar once. They monitor ongoing production. If a manufacturer changes their cell line, their bioreactor temperature, or their purification process, they must prove the new version still matches the original’s variability profile. That’s called a "manufacturing change control strategy." And it’s reviewed every single time.
For interchangeable biosimilars, the bar is even higher. Companies must run "switching studies"-where patients alternate between the reference product and the biosimilar multiple times over months. They track immune responses, side effects, and effectiveness. Only if there’s no detectable difference can the FDA approve interchangeability.

What’s changing in 2025 and beyond
The biosimilars market is growing fast. In 2023, it was worth $10.6 billion. By 2028, it’s expected to hit $35.8 billion. More companies are entering the space-Amgen, Pfizer, Sandoz-and more complex biologics are coming: antibody-drug conjugates, cell therapies, gene therapies. These are even harder to make consistently than monoclonal antibodies.
Regulators are adapting. The FDA’s latest guidance, updated in January 2023, pushes for even more detailed analytical data. By 2026, experts predict 70% of new biosimilar applications will include data to support interchangeability-up from 45% in 2023. That means more patients will be able to switch to lower-cost options without needing a doctor’s note.
And as analytical tools get better, we’ll see even finer control over variability. Scientists are now able to detect differences smaller than one molecule in a million. That’s not just precision-it’s peace of mind.
Bottom line: variability isn’t a problem. It’s a feature
Lot-to-lot variability isn’t something to fear. It’s a natural consequence of making medicines from living systems. The real question isn’t "Is it different?" It’s "Is it safe? Is it effective?" And the answer, for both reference biologics and approved biosimilars, is yes.
Thanks to strict science, rigorous oversight, and advanced technology, we can now trust that even if two bottles aren’t identical, they’ll work the same way. That’s the power of modern biopharma. And it’s why biosimilars are now part of 32% of all biologic prescriptions in the U.S.-and counting.


Laurie Sala
Okay, but can we just talk about how wild it is that my insurance won't cover the 'original' Humira unless I prove I 'failed' the biosimilar first?? Like, I'm not a lab rat!! And the labels?? The lot numbers?? The tiny print?? I have to cross-reference three different websites just to make sure I'm not getting the 'wrong' version of my life-saving drug!!!
Suresh Ramaiyan
This is such an important perspective. It's easy to think of medicine as something perfect and exact, but life doesn't work that way. Even our bodies are constantly changing-why should the drugs that help us be any different? The real miracle isn't that biologics vary-it's that we've learned to manage that variation with such precision. It's not magic, it's science, and it deserves respect.
Katy Bell
So… I’m just gonna say this out loud: I once had a bad reaction to a new lot of my biologic. No one believed me because ‘it’s the same drug.’ But my body knew. And now I keep a little notebook-lot number, date, how I felt. It’s weird, but it’s my survival tactic. I wish more doctors took this seriously.
Ragini Sharma
so like… biosimilars are basically the ‘homemade’ version of biologics? like, same recipe but your cousin bakes it and it’s just… slightly different? also why is everything so complicated?? i just wanna take my pill and not think about glycosylation 😭
Linda Rosie
Regulatory rigor is non-negotiable. The FDA’s approach is scientifically sound and patient-centered.
Vivian C Martinez
I love how this breaks down something so complex into something we can actually understand. It’s not about perfection-it’s about consistency within a safe range. That’s the kind of science I can get behind. Keep sharing this kind of clarity!
Ross Ruprecht
Ugh, another article about drug chemistry. Can we just get cheaper generics already? Why does everything have to be so damn complicated?
Bryson Carroll
Let’s be real-this whole ‘lot variability’ thing is just Big Pharma’s way of justifying their monopoly. They pretend it’s science but it’s just a smokescreen so they can charge $70,000 a year for a vial of protein soup. The FDA is asleep at the wheel
Lisa Lee
Why are we letting foreign companies make our life-saving drugs? This is a national security issue. If we can’t make biologics ourselves, we’re at the mercy of whoever controls the cell lines. This isn’t innovation-it’s dependency.
Jennifer Shannon
You know, I think about this like a jazz improvisation-same melody, same instruments, but every performance is a little different because the musicians are alive, feeling the moment. That’s what biologics are: a living performance of science. The variations? They’re the soul of the drug. The FDA doesn’t just allow them-they celebrate them, as long as the harmony holds. And that’s beautiful, really. We don’t need identical twins-we need harmonious variations.
Kezia Katherine Lewis
Post-translational modifications-specifically glycosylation patterns-are the primary drivers of pharmacokinetic and pharmacodynamic heterogeneity in monoclonal antibody therapeutics. The FDA’s comparability protocols, as outlined in the 2014 Guidance for Industry, require demonstration of structural and functional equivalence within statistically validated tolerance limits, which are typically derived from historical reference product data spanning multiple lots. This is not mere regulatory checkbox compliance-it is a rigorous, evidence-based framework for ensuring clinical continuity.
Henrik Stacke
It’s fascinating how the British and American approaches differ here. In the UK, we’ve embraced biosimilars faster-partly because the NHS needs cost control, partly because our clinicians trust the data. But I’ve seen patients here panic over ‘different’ lot numbers too. Maybe the real challenge isn’t the science-it’s the storytelling. We need to teach people that ‘different’ doesn’t mean ‘worse.’
Manjistha Roy
As someone who trains new lab techs, I’ve seen firsthand how one lot change can throw off weeks of calibration. We run parallel testing, document everything, and still get calls from worried clinicians. This isn’t just science-it’s a daily act of patience and precision. We owe it to patients to keep doing it right.
Jennifer Skolney
This made me feel so much better about my meds 😊 I used to stress out every time my pharmacy switched the brand, but now I get it-it’s like switching from one brand of peanut butter to another. Same core, different texture. And if it works? That’s what matters. Thanks for explaining it so clearly!
JD Mette
I appreciate the depth of this post. It’s rare to see the science explained without hype or fear. I’ve been on biologics for eight years. I’ve never had a bad reaction-but I’ve always wondered why my bloodwork shifts slightly between refills. Now I know it’s normal. Thank you.