Thiazide Diuretics and Gout: What You Need to Know About Uric Acid Risks
Uric Acid Risk Calculator
Thiazide diuretics like hydrochlorothiazide can increase uric acid levels by 6-21% within days, raising gout risk. This calculator estimates your risk based on your current health factors.
Many people take thiazide diuretics like hydrochlorothiazide (HCTZ) to control high blood pressure. It’s cheap, effective, and has been used for over 60 years. But if you’ve ever had gout-or know someone who has-you’ve probably heard a warning: thiazide diuretics can trigger gout flares. This isn’t just a side effect you might ignore. It’s a real, measurable risk that changes how you manage your health.
How Thiazide Diuretics Raise Uric Acid
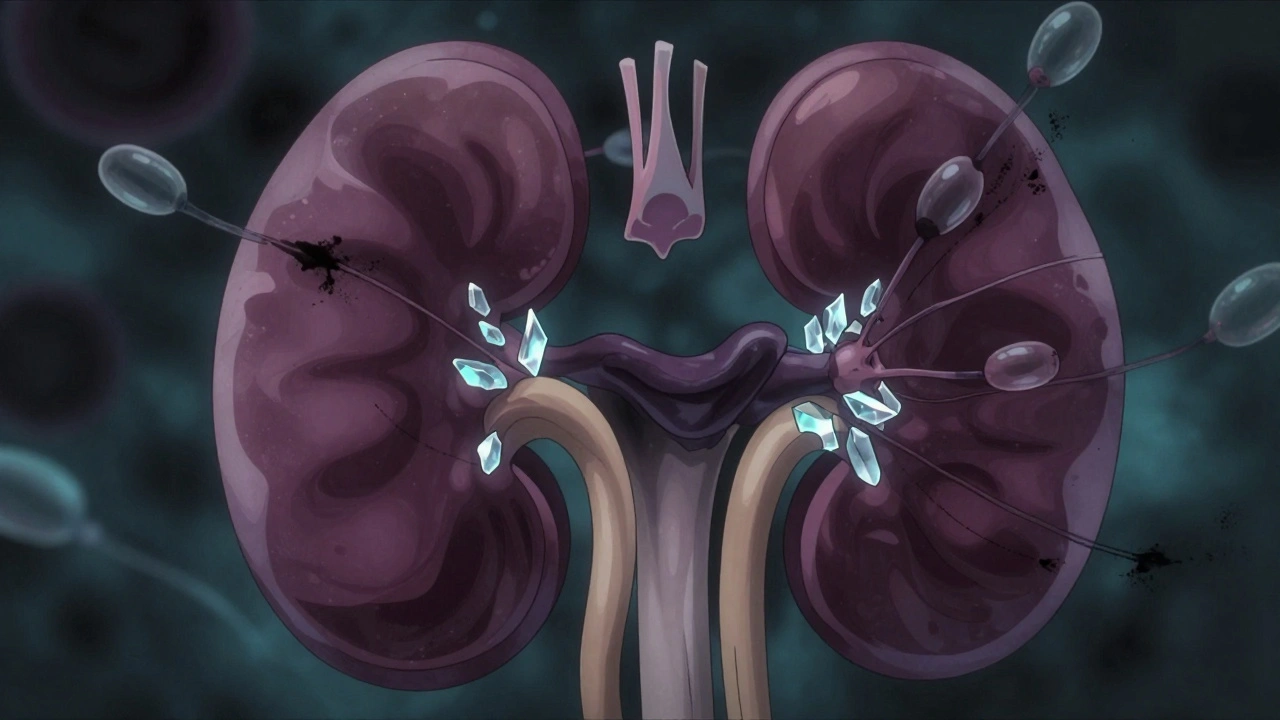
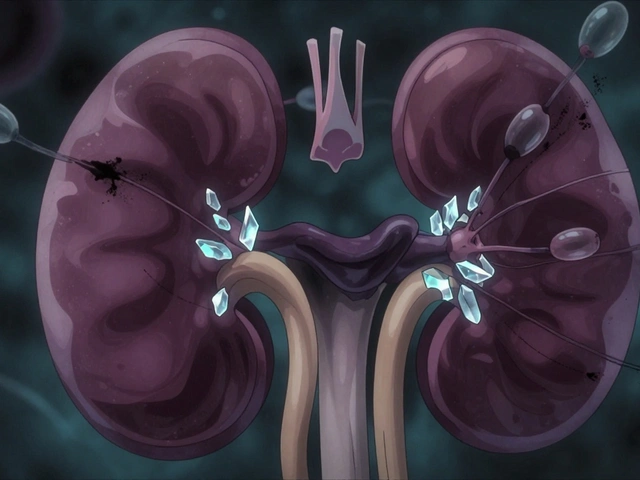
Thiazide diuretics work by blocking sodium reabsorption in the kidneys. That means more water and salt leave your body, lowering blood pressure. But here’s the catch: they also mess with how your kidneys handle uric acid. Uric acid is a waste product from breaking down purines in food. Normally, your kidneys filter it out. But thiazides interfere with specific transporters-OAT1 and OAT4-that move uric acid out of the blood and into urine.
Instead of being flushed away, uric acid gets trapped in your bloodstream. Studies show serum uric acid levels can jump 6% to 21% within just 3 to 7 days of starting a thiazide. This isn’t a slow build-up. It’s fast. And it doesn’t go away unless you stop the drug. If your levels stay high for months, uric acid crystals can form in your joints-especially your big toe-and trigger a gout attack.
Who’s Most at Risk?
Not everyone on thiazides gets gout. But some people are far more likely to. If you already have high uric acid levels-over 7.0 mg/dL for men or 6.0 mg/dL for women-you’re in a high-risk group. So are people who’ve had even one gout flare in the past. The risk isn’t just about the drug. It’s about your body’s baseline.
Research from a 2024 study tracking over 247,000 people found that after 180 days of taking thiazides, the chance of needing gout medication jumped by 41%. That’s not a small number. It’s a turning point. And it’s why doctors now check uric acid levels before prescribing these drugs. The American College of Cardiology and American Heart Association recommend it.
Other factors stack the deck. Obesity, drinking alcohol, eating red meat or shellfish, and having kidney problems all raise your uric acid. If you’re on a thiazide and you’re doing any of those things, your risk multiplies.
Thiazides vs. Other Diuretics
Not all diuretics are the same when it comes to gout. Loop diuretics like furosemide are even more likely to trigger flares than thiazides. But among thiazides, there’s confusion. For years, people thought chlorthalidone was worse than hydrochlorothiazide. But a 2019 study found they carry nearly the same risk when given in similar doses.
Here’s the surprise: potassium-sparing diuretics like spironolactone don’t raise uric acid at all. That’s because they work differently. They block aldosterone, not sodium-chloride transporters. So if you have both high blood pressure and gout, spironolactone might be a better fit.

What Happens When You Get Gout on Thiazides?
There’s no difference between gout caused by thiazides and gout from any other cause. The pain is the same-sudden, intense, often in the big toe. The joint swells, turns red, and feels hot to the touch. Blood tests will show uric acid above 6.8 mg/dL, the point where crystals start forming.
The problem isn’t just the flare. It’s the chain reaction. Once you have one gout attack, you’re more likely to have more. And doctors often respond by prescribing colchicine or allopurinol to prevent future flares. But here’s the catch: those drugs cost more. In one study, nearly 19% of people on thiazides ended up needing gout medication within two years. That’s a lot of extra prescriptions, side effects, and costs.
What Should You Do?
If you’re on a thiazide and have never had gout, don’t panic. But do talk to your doctor. Ask if your uric acid level has been checked. If it hasn’t, get it tested. If your level is above 7.0 mg/dL, you might want to consider alternatives.
If you already have gout, thiazides aren’t the best choice. The European League Against Rheumatism says you shouldn’t use them as your main blood pressure drug if you have gout-unless you’re also taking urate-lowering therapy like allopurinol.
Good alternatives exist. Losartan, a blood pressure pill in the ARB class, actually helps your kidneys flush out uric acid. Calcium channel blockers like amlodipine don’t raise uric acid either. They’re not always cheaper than generic thiazides, but they’re safer for your joints.
Lifestyle Matters-More Than You Think
Medication isn’t the whole story. Diet and habits play a huge role. Alcohol, especially beer and spirits, spikes uric acid. Red meat, organ meats, and shellfish are loaded with purines. Even sugary drinks-especially those with fructose-can trigger flares.
Weight loss helps. Losing just 5-10% of your body weight can cut uric acid levels significantly. Drinking more water-aim for 2 to 3 liters a day-helps your kidneys flush out the crystals before they settle in your joints.
The European guidelines say your target uric acid level should be below 6.0 mg/dL if you have gout. That’s lower than most people think. It’s not enough to just treat the pain. You need to treat the cause.
The Bigger Picture: Benefits vs. Risks
Thiazide diuretics are still one of the most prescribed blood pressure drugs in the world. In the U.S. alone, over 35 million prescriptions were filled in 2022. Why? Because they work. They cut stroke and heart attack risk in people with high blood pressure. For someone with no history of gout, the benefits often outweigh the risks.
But that calculus changes if you’ve had a gout flare. Then, the risk isn’t just a side effect-it’s a trigger for chronic pain, joint damage, and long-term disability. That’s why smart doctors now screen for it. That’s why guidelines have changed. That’s why alternatives exist.
It’s not about avoiding thiazides entirely. It’s about using them wisely. Test first. Monitor often. Choose alternatives when needed. And never ignore a swollen toe.


Ibrahim Yakubu
Let me tell you something nobody else will: thiazides don't cause gout, they expose it. Your body's been holding onto uric acid like a dirty secret for years, and this drug just flips the table. I've seen it in Lagos clinics - men in their 50s, drinking palm wine, eating goat meat, then blaming HCTZ. The drug didn't make them sick. Their lifestyle did. The real crime is doctors prescribing this like it's candy without checking baseline uric acid. That's malpractice, not medicine.
And don't get me started on the 'alternatives' crowd. Losartan? Sure, it lowers uric acid - but it also makes you cough like you're dying of tuberculosis. Amlodipine? Swollen ankles, constipation, dizziness. Every pill has a price. Stop pretending one is magic.
Uric acid isn't evil. It's an antioxidant. Your body makes it for a reason. The problem isn't the drug. It's that we've turned into a nation of metabolic zombies eating sugar, sitting still, and expecting a pill to fix everything.
I've been on HCTZ for 8 years. My uric acid was 8.2 when I started. Now it's 6.1. How? I stopped drinking beer. I lost 22 kilos. I drink 3 liters of water daily. No magic. Just discipline. But nobody wants to hear that. They want a new prescription.
Stop blaming the medicine. Start blaming the mirror.
And yes, I'm a pharmacist. No, I don't work for Big Pharma. I work for the people who still have two feet left to stand on.
Brooke Evers
I just want to say how important it is to approach this with compassion - especially for people who’ve been on thiazides for years without knowing the risk. Many of us were prescribed these meds because our doctors assumed we’d never have gout, or that we’d just ‘deal with it’ if it happened. But gout isn’t just a bad toe - it’s chronic pain that can make you feel like your body is turning against you.
I have a friend who had her first flare after being on HCTZ for five years. She didn’t even know what uric acid was. She felt guilty, like she’d done something wrong. But it wasn’t her fault. It was a system that prioritizes cost over long-term monitoring.
Thank you for including the lifestyle advice - because change is possible. One of my clients lost 15% of her body weight, cut out sugary drinks, and now her flares are rare. She still takes her blood pressure med - just switched to losartan. It wasn’t easy, but she didn’t give up. And that’s the story we need to hear more of: not fear, but empowerment.
Doctors need to screen. Patients need to ask. Communities need to support. This isn’t about vilifying a drug - it’s about making sure no one has to suffer in silence because no one told them the truth.
Thank you for writing this. It’s rare to see someone explain the science and still keep the humanity in it.
Chris Park
Thiazides are a government mind-control tool disguised as hypertension treatment. You think they care about your kidneys? No. They care about your wallet. The pharmaceutical industry funds every ‘study’ that says ‘moderate risk.’ The real data? Hidden. Uric acid spikes? A distraction. The real goal: get you hooked on allopurinol and colchicine - $400/month drugs with side effects that make you question your sanity.
Why do you think spironolactone is ‘safer’? Because it’s off-patent. No profit. So they bury it. Meanwhile, Merck makes billions off HCTZ and its ‘alternatives’ - which are just rebranded versions of the same poison.
And don’t get me started on ‘drink water.’ That’s a placebo tactic. If water fixed gout, why do 70% of people in the Amazon have zero gout and drink river water? Because they don’t eat processed food. Because they don’t take FDA-approved toxins.
The truth? Thiazides are part of a systemic poisoning of the population. You think your doctor is helping you? He’s paid by the same companies that sell you the problem and the ‘solution.’
Stop taking the pills. Go keto. Stop sugar. Go raw. Or die quietly on your couch while Big Pharma counts your blood pressure pills.
Saketh Sai Rachapudi
india has been using ayurveda for 5000 years and we never had gout problem why we need this western medicine bullshit its all about money and pharma companies selling pills to poor people who dont even know what uric acid is
joanne humphreys
I appreciate how thorough this post is - especially the part about uric acid targets being below 6.0 mg/dL. That’s not common knowledge, even among some clinicians.
I’ve been managing hypertension for over a decade, and my doctor never mentioned uric acid until I had my first flare. I wish someone had asked me earlier. I also didn’t realize how much fructose was in my ‘healthy’ smoothies until I read this.
It’s easy to feel overwhelmed by all the info out there, but this breaks it down without fearmongering. I’ve started asking my doctor for a baseline uric acid test before any new meds. I think more people should do that.
Also, I’m curious - has anyone here tracked their uric acid levels over time while switching meds? I’d love to see real-world data, not just studies.
Kumar Shubhranshu
HCTZ not the villain. Lifestyle is. Cut sugar. Drink water. Lose weight. Done.
Mayur Panchamia
Oh, so now we’re blaming the patient again? ‘Just drink water!’ Like I have time to chug 3 liters while working two jobs and raising three kids on minimum wage! And where the hell am I supposed to buy ‘healthy food’ in my neighborhood? The only thing within walking distance is a gas station with soda and chips!
And let’s be real - if you’re poor, you don’t get to choose between ‘losartan’ and ‘HCTZ.’ You get whatever the Medicaid formulary gives you. You don’t get to ‘ask your doctor’ - your doctor is overworked, underpaid, and pressured by insurance companies to prescribe the cheapest option!
Stop pretending this is a personal failure. It’s systemic. It’s structural. It’s poverty disguised as ‘lifestyle.’
And don’t even get me started on ‘Ayurveda’ comments - if your grandmother’s turmeric paste worked, why are you on a ventilator? Because modern medicine saved your life. So shut up and stop romanticizing starvation diets.
Fix the system. Don’t shame the sick.
Karen Mitchell
While the author presents a reasonably well-structured overview of the pharmacological implications of thiazide diuretics on serum uric acid levels, one cannot help but observe a conspicuous absence of primary-source citations for the 2024 cohort study referenced, as well as the 2019 comparative analysis between chlorthalidone and hydrochlorothiazide. Furthermore, the assertion that ‘the American College of Cardiology and American Heart Association recommend’ baseline uric acid testing is not substantiated by any specific guideline document number or publication year, which diminishes the credibility of the entire argument.
Additionally, the conflation of correlation with causation - particularly in the assertion that lifestyle factors ‘multiply’ risk - lacks statistical clarification. Are we speaking of additive effects? Multiplicative? Relative risk? Hazard ratios? Without such precision, this becomes anecdotal rather than evidence-based.
Finally, the suggestion that patients should ‘never ignore a swollen toe’ is not only medically reductive but potentially dangerous, as it may encourage self-diagnosis and delay appropriate rheumatologic evaluation. A swollen joint may indicate septic arthritis, pseudogout, or reactive arthritis - all of which require urgent, distinct interventions.
One appreciates the intent. But rigor must precede accessibility.