Cervical Myelopathy: Spinal Stenosis Symptoms and When Surgery Is Needed
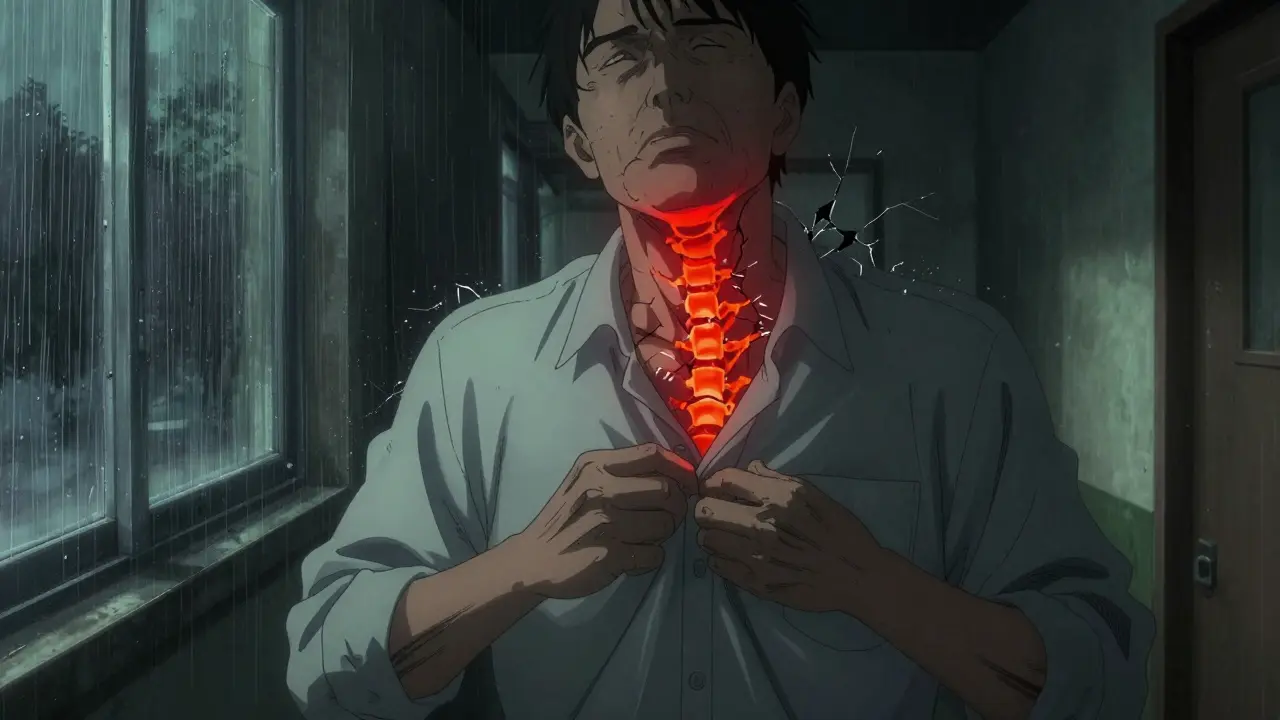
When your hands start fumbling with buttons, your walk feels unsteady, or you suddenly drop things you used to handle without thinking, it’s easy to blame aging. But if these symptoms are new, worsening, and paired with numbness in your arms or trouble controlling your bladder, it could be something more serious: cervical myelopathy. This isn’t just a stiff neck. It’s your spinal cord being squeezed in your neck - and if left untreated, it can lead to permanent nerve damage.
What Exactly Is Cervical Myelopathy?
Cervical myelopathy isn’t the same as cervical stenosis, though the two are often confused. Spinal stenosis means the space inside your neck bones has narrowed. Cervical myelopathy means that narrowing is actually squishing your spinal cord - and damaging it. Think of it like this: stenosis is the pipe getting smaller. Myelopathy is the water inside the pipe starting to leak because the walls are crushed. The most common cause is cervical spondylotic myelopathy (CSM), which happens as part of normal aging. Over time, discs between your neck bones dry out and collapse, bone spurs grow, ligaments thicken, and joints swell. All of this slowly eats away at the space meant for your spinal cord. By age 70, nearly 1 in 11 people have signs of it. It’s the top reason adults over 55 develop spinal cord problems that aren’t from injury.How Do You Know It’s Not Just Arthritis?
Many people assume neck pain and stiffness mean arthritis. But myelopathy doesn’t always hurt. In fact, up to half of patients don’t even have neck pain. The real red flags are neurological - changes in how your body moves and feels. Early signs include:- Clumsy hands - fumbling with keys, dropping utensils, struggling to tie shoelaces
- Walking like you’re drunk - unsteady gait, bumping into things, feeling like your feet are heavy
- Numbness or tingling in fingers, arms, or legs
- Weakness in arms or legs - difficulty lifting objects or climbing stairs
- Increased reflexes - your doctor might notice your knee or ankle jerks too hard during an exam
How Is It Diagnosed?
A doctor can’t just look at an X-ray and say, “You’ve got myelopathy.” That’s because many people over 40 have narrow spinal canals without any symptoms. The key is finding both the narrowing and signs of spinal cord injury. The gold standard is an MRI. It shows exactly where the cord is being squished and whether there’s damage inside the cord itself - seen as bright spots on T2-weighted images. A normal spinal canal is about 17-18mm wide. At 13mm or less, it’s stenotic. At 10mm or under, it’s severe - and myelopathy is likely. Doctors also use the Japanese Orthopaedic Association (JOA) score. It’s a simple test that checks motor function, sensation, and bladder control on a scale of 0 to 17. A score below 14 means myelopathy is present. X-rays help spot bone spurs and disc collapse, but they don’t show the cord. EMG and nerve tests can catch early damage even before symptoms get bad.When Is Surgery the Only Real Option?
Conservative treatment - physical therapy, pain meds, activity changes - might help a little if your symptoms are mild. But here’s the hard truth: only about 28% of people with mild myelopathy improve over two years. Almost two-thirds get worse. If your JOA score is below 12, or if your symptoms are getting worse - even slowly - surgery is the only proven way to stop the damage. The American Academy of Orthopaedic Surgeons gives this a strong, top-level recommendation. Delaying surgery doesn’t just mean more pain. It means less chance of recovery. Studies show that patients who have surgery within six months of noticing symptoms recover 37% better than those who wait over a year. Every month you wait, your chance of full recovery drops by about 3%.
What Surgery Options Exist?
There’s no one-size-fits-all fix. The right approach depends on where the cord is compressed, how many levels are involved, and your spine’s natural curve. Anterior approaches (from the front of the neck):- ACDF (Anterior Cervical Discectomy and Fusion): Removes the damaged disc and fuses the bones with a plate. Best for 1-2 level problems. Success rate: 85-90% for symptom relief. Downside: 5-7% risk of needing another surgery nearby in 10 years.
- Cervical Disc Arthroplasty (Artificial Disc): Removes the disc but replaces it with a moving implant. Preserves motion. FDA approved for 2-3 levels in 2023. Early results show 81% success at two years - better than fusion for keeping movement.
- Laminectomy with fusion: Removes the back part of the bone to relieve pressure, then fuses the spine. Used for multi-level disease. High success (85%) but can cause more post-op neck pain.
- Laminoplasty: Hinges the bone open like a door instead of removing it. Less pain, faster recovery. Works best for 3+ levels. Slightly lower neurological recovery (78%) than fusion, but fewer complications.
What Are the Risks?
Surgery isn’t risk-free. About 4-6% of patients face major complications:- Dysphagia (trouble swallowing) - affects 22% in the first few months, usually fades
- C5 nerve palsy - shoulder or arm weakness, happens in 3-5% of cases
- Neurological worsening - rare, but 1-2% of patients end up worse after surgery
- Chronic neck pain - 18-35% of patients still have discomfort months later
What Happens After Surgery?
Recovery isn’t quick. Most people stay in the hospital 1-3 days. Full healing takes 3-6 months. You’ll need physical therapy for 8-12 weeks. Focus is on regaining balance, retraining your hands, and strengthening your neck muscles. About 82% of patients report better hand function a year after surgery. But only 65% regain normal walking ability. Some will still need a cane or walker. The earlier you operate, the better your odds of full recovery.
What Should You Do If You Suspect It?
If you’ve noticed any of these symptoms - especially if they’re getting worse - don’t wait. See a spine specialist. Don’t rely on your primary care doctor to diagnose this. It’s easy to miss. The average patient sees three doctors before getting the right diagnosis - and waits nearly 15 months. Get an MRI within 2-4 weeks of noticing neurological symptoms. Don’t delay. If your doctor says, “Just wait and see,” get a second opinion. The data is clear: early surgery saves function. Late surgery saves you from worse outcomes - but not from permanent damage.What’s Changing in Treatment?
The field is moving fast. New tools are helping doctors pick the right surgery for the right person:- Robotic-assisted surgery is being tested - it could cut revision rates by a third by improving precision
- Genetic tests are being studied to predict who degenerates faster
- Drugs like riluzole are being tested alongside surgery to protect nerves during recovery
It’s not about avoiding surgery. It’s about doing it at the right time - before your hands stop working, before your walk becomes unsafe, before you lose control of your body. Cervical myelopathy doesn’t fix itself. And waiting too long means losing the chance to get it back.
Can cervical myelopathy get better without surgery?
In rare cases, mild symptoms may stabilize with rest and physical therapy, but true improvement without surgery is uncommon - only about 28% of patients see any benefit over two years. Most people (63%) get worse over time. If your symptoms are worsening, even slowly, surgery is the only way to prevent permanent damage.
How do I know if I need surgery?
If your JOA score is below 12, or if you’re experiencing worsening hand clumsiness, gait problems, or bladder control issues, surgery is strongly recommended. Imaging must show spinal cord compression with signs of damage (like T2 hyperintensity on MRI). If your symptoms are getting worse, don’t wait - early intervention gives you the best chance of recovery.
What’s the difference between ACDF and laminoplasty?
ACDF is done from the front of the neck and is best for 1-2 levels. It fuses the bones, which stops motion at that spot but gives strong relief. Laminoplasty is done from the back, opens up the spinal canal like a door, and is better for 3 or more levels. It preserves neck movement and causes less pain, but neurological recovery is slightly lower than with fusion.
How long does recovery take after cervical myelopathy surgery?
Most patients go home in 1-3 days. You’ll need physical therapy for 8-12 weeks. Full recovery - including regaining hand function and stable walking - typically takes 3 to 6 months. Some people continue improving for up to a year. The sooner you start rehab, the better your outcome.
Can I avoid surgery with exercise or chiropractic care?
Exercise and physical therapy can help maintain strength and mobility, but they won’t reverse spinal cord compression. Chiropractic adjustments in the neck are not recommended and can be dangerous if you have myelopathy. The spinal cord is already compressed - adding force to it risks further injury. Surgery is the only proven way to relieve pressure on the cord.
What happens if I ignore the symptoms?
Ignoring symptoms leads to progressive nerve damage. Between 20% and 60% of untreated patients will experience significant worsening over 2-5 years. This can mean permanent weakness, loss of coordination, paralysis, or loss of bladder/bowel control. Once the spinal cord is severely damaged, even surgery can’t restore lost function.



Shanahan Crowell
Okay, I’ve been fumbling with my keys for months now-thought it was just getting old. But this? This is the first time someone put it in terms I actually understood. My neck’s been stiff for years, but the numbness in my fingers? The way I trip over nothing? That’s not aging. That’s my spinal cord screaming. I’m booking an MRI tomorrow.
Thank you for writing this like a human, not a textbook.
Kerry Howarth
Early intervention is non-negotiable. Delaying surgery increases permanent damage risk by 3% per month. Data is clear. Act now.
Tiffany Channell
Let’s be real. This post reads like a pharmaceutical ad disguised as medical advice. Who funded this? How many of these ‘success rates’ are cherry-picked? And why is there zero mention of the 15% of patients who end up worse after surgery? You’re scaring people into scalpel territory without context.
Joy F
It’s not just a spinal cord compression-it’s a metaphysical unraveling. Your body becomes a foreign landscape: your hands, once instruments of creation, now betray you like traitorous limbs. The weight of your own skeleton becomes a prison. And the silence of the medical establishment? That’s the real horror. We’re told to ‘wait and see’ while our nervous system slowly dissolves into static. This isn’t medicine-it’s a slow-motion execution disguised as patience. And the worst part? We’re told to be grateful if we get a 65% recovery rate. Sixty-five percent. As if that’s a win. When did we stop fighting for wholeness?
They call it ‘degenerative.’ I call it betrayal by time. And surgery? It’s not a cure. It’s a ceasefire.
Haley Parizo
You think this is about surgery? It’s about capitalism. Insurance won’t cover an MRI unless you’re in agony. Doctors get paid more to do fusion than to explain what’s happening. The system doesn’t want you to know you’re being slowly disabled-because if you did, you’d demand answers. And answers cost money. This isn’t a medical issue. It’s a moral failure dressed in white coats. I’ve seen people wait five years because their copay was $750. Five years. For a condition that gets worse every day. You’re not just losing function-you’re losing faith in the system that’s supposed to protect you.
Angela Fisher
Wait. So you’re telling me the government and big pharma are pushing this? I read online that cervical myelopathy is actually caused by 5G signals messing with your spinal fluid. And the MRI machines? They’re calibrated to make you think you have it so you’ll get surgery and they can implant those ‘smart’ spinal plates that track your emotions. I know a guy whose cousin’s neighbor got the surgery and now her dreams are being streamed to a server in Nevada. Why does the JOA score even exist? Who made it? What if it’s rigged? And what about the 18% of people who still have pain after surgery? Are they the ones who got the fake implants? I’m not getting scanned until I get a second opinion from a guy who talks to trees. He says my spine is ‘out of alignment with the earth’s frequency.’
Neela Sharma
My mother had this. No surgery. Just yoga, turmeric, and silence. She walks again now. Not perfect. But she walks. In India, we don’t rush to the knife. We wait. We breathe. We trust the body to heal-if you give it space. Not every nerve needs a scalpel. Sometimes it needs stillness.
But I hear you. The West rushes. I get it. Still. I wonder if we’re losing something by always fixing instead of listening.
Shruti Badhwar
While the author presents compelling clinical data regarding the progressive nature of cervical myelopathy, it is imperative to acknowledge that individual patient variables-including comorbidities, socioeconomic access to care, and preoperative neurological baseline-significantly influence surgical outcomes. The generalized recommendation for early intervention, though statistically valid, may not be universally applicable without multidisciplinary evaluation. A one-size-fits-all surgical paradigm risks overlooking holistic patient-centered care pathways.
Michael Burgess
Bro. I had this. ACDF at 58. Three days in the hospital. PT for three months. I still drop my coffee sometimes. But I can tie my shoes again. And I didn’t end up in a wheelchair. If you’re reading this and your hands are acting up-go get the MRI. Don’t wait. Don’t Google it for six months. Just go. I almost didn’t. Now I’m glad I did.
Also, if you’re nervous about surgery? Totally normal. But the thing they don’t tell you? The scariest part is waiting. Not the knife.
❤️
Liam Tanner
Interesting breakdown. I’ve seen patients delay for years because they thought it was ‘just carpal tunnel.’ The moment they realize it’s their spinal cord, not their wrist? That’s when the panic hits. And honestly? That’s when the real work begins.
Hank Pannell
There’s a deeper ontological question here: if the body is a vessel of consciousness, and the spinal cord is the conduit between mind and physical form, then compressing it isn’t just a biomechanical failure-it’s an epistemological rupture. We experience the world through proprioception, through motor intentionality. When that’s disrupted, we don’t just lose function-we lose our sense of embodiment. The surgical intervention isn’t merely structural; it’s a reclamation of selfhood. And yet, the medical-industrial complex reduces this to a CPT code and a fusion rate. We’ve quantified the soul into a JOA score. Is that progress?
veronica guillen giles
Oh, so now we’re supposed to panic because we can’t button our shirts? Next you’ll tell me we should all get spine implants before we turn 40. I’ve had ‘clumsy hands’ since I was 22. It’s called being a messy human. Maybe stop selling fear as medicine and start selling patience? Or, I don’t know, therapy for anxiety about aging?
erica yabut
Let’s be honest-this is the kind of article that gets shared by people who think ‘neurological symptoms’ is a fashion trend. You don’t get cervical myelopathy because you’re ‘aging.’ You get it because you didn’t do enough yoga, didn’t drink enough alkaline water, and didn’t sleep on a Himalayan salt pillow. The real villain here? Toxic modernity. And the solution? Not surgery. A retreat to a cabin in the Rockies with a crystal grid and a certified somatic healer. But no, let’s just slice open the neck and call it science.
Vincent Sunio
The data presented is methodologically flawed. The cited 37% improvement differential between early and late surgery is derived from non-randomized cohorts with significant selection bias. Furthermore, the JOA scoring system lacks inter-rater reliability in populations with comorbid neuropathy. The recommendation for universal early surgical intervention is not supported by Level I evidence and constitutes an overreach of clinical authority. One must question the influence of industry-sponsored research on these guidelines.
Philip Leth
My pops had this. Laminoplasty. Walked out of the hospital like he’d just won a marathon. Now he’s 82 and still gardening. You don’t wait. You don’t Google it. You don’t ask Reddit. You go see the spine guy. And you don’t come back until you’ve got the MRI in hand. Simple as that.