Hepatitis B: Chronic Infection, Antivirals, and Vaccination Explained
Chronic hepatitis B isn’t just a lingering infection-it’s a silent threat to your liver that can go unnoticed for decades. If you’re living with it, or know someone who is, understanding the real options for treatment and prevention isn’t optional. It’s life-saving. The virus doesn’t always cause symptoms, but it can slowly scar your liver, leading to cirrhosis or liver cancer. The good news? We now have tools to stop it in its tracks. And the better news? You don’t need to wait until your liver is damaged to act.
What Chronic Hepatitis B Really Means
Chronic hepatitis B happens when your body can’t clear the hepatitis B virus (HBV) within six months. That’s the official cutoff. If the hepatitis B surface antigen (HBsAg) is still in your blood after that time, you’re considered chronically infected. About 296 million people worldwide are living with this right now, according to the WHO. Many don’t know they have it. That’s the danger. Without regular checks, the virus keeps quietly replicating, damaging liver cells over time.
It’s not about how you feel. Someone can feel perfectly fine and still have advanced liver scarring. That’s why testing matters more than symptoms. A simple blood test for HBsAg is the first step. If it’s positive, the next step is checking your HBV DNA levels, ALT (a liver enzyme), and liver stiffness-all of which tell your doctor how active the virus is and how much damage has already happened.
When Treatment Starts-It’s Not One Size Fits All
For years, doctors waited for signs of liver damage before starting antivirals. That’s changed. The 2025 guidelines, updated with data from over 120 new studies, now say: if your HBV DNA is above 2,000 IU/mL, treatment should be considered-even if your ALT is normal and you have no scarring. This is a major shift. It means we’re treating earlier, not waiting for harm to occur.
There are exceptions. If you already have cirrhosis, treatment is non-negotiable. Even if your viral load is low, you still need antivirals. For people with decompensated cirrhosis (where the liver is failing), antivirals are just the start-you also need to be evaluated for a liver transplant.
Guidelines vary slightly. The WHO 2024 guidelines are the most aggressive: treat everyone with HBV DNA over 2,000 IU/mL, no matter what else is going on. The AASLD and EASL guidelines are a little more selective, but they all agree: if you have fibrosis or are over 30, don’t wait. Start treatment.
The Top Antivirals: What Works and What’s Safer
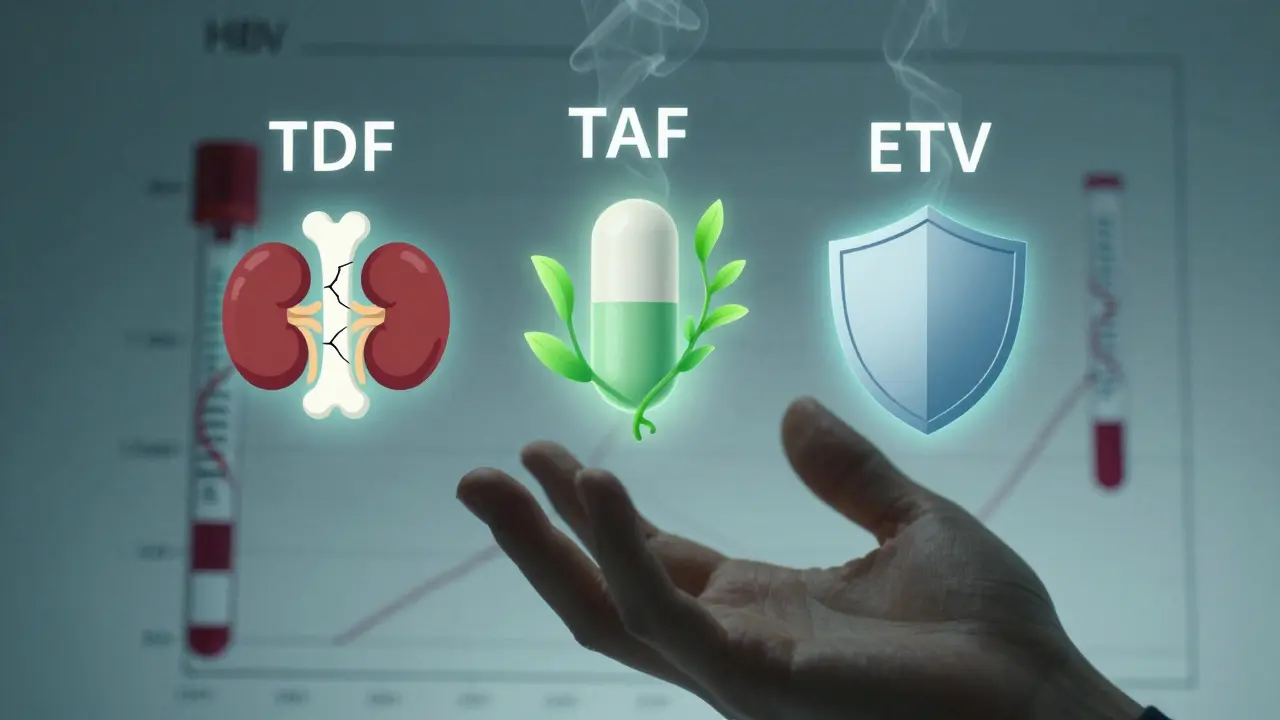
Three drugs are now the standard first-line treatments: tenofovir disoproxil fumarate (TDF), entecavir (ETV), and tenofovir alafenamide (TAF). All of them are highly effective at suppressing the virus. But they’re not the same.
TDF has been around longer and works well. But it can affect your kidneys and bones over time. Studies show it can cause protein in the urine, reduced bone density, and even rare kidney damage. That’s why TAF was developed. TAF (sold as VEMLIDY) delivers the same antiviral punch with much less strain on your body. Clinical trials found that switching from TDF to TAF improved kidney markers within 24 weeks and boosted bone mineral density. If you have kidney issues, osteoporosis, or are older, TAF is often the better choice.
Entecavir is another solid option, especially if you’re not on other medications. It’s taken once a day, has a high barrier to resistance, and rarely causes side effects. But it’s not recommended if you’ve had prior treatment with other antivirals.
Pegylated interferon (PEG-IFN) is rarely used now. It’s given as a weekly injection for up to a year and comes with flu-like side effects, depression, and fatigue. It’s mostly reserved for young patients with a strong immune system who want a finite treatment course-meaning they hope to stop meds after a year.
Special Cases: Pregnancy, HIV, and Co-Infections
If you’re pregnant and have hepatitis B, you’re not alone. The WHO now recommends giving tenofovir to pregnant women with HBV DNA above 5.3 log10 IU/mL starting at week 28. This cuts the risk of passing the virus to the baby by over 90%. After birth, the baby gets the first dose of the hepatitis B vaccine and hepatitis B immune globulin (HBIG) within 12 hours. This combo is 95% effective at preventing infection.
If you have HIV and hepatitis B, you need both viruses treated at the same time. The 2025 guidelines say: start HIV meds that also work against HBV-like tenofovir or emtricitabine-as soon as you’re diagnosed. Don’t wait. If you’re getting treated for hepatitis C with direct-acting antivirals (DAAs), you also need to take HBV antivirals during and after treatment. Otherwise, your HBV can flare dangerously.
And don’t forget hepatitis D. If you’re HBsAg-positive, you should be tested for HDV. It’s rare in most places but can make HBV much worse. Testing is simple and should be routine.
The Vaccine: Your Best Shield Against HBV
The hepatitis B vaccine is one of the most effective vaccines ever made. It’s safe, it’s cheap, and it’s 95% effective at preventing infection. The standard schedule is three shots: first shot, then one month later, then six months after the first. Even if you’re past childhood, it’s never too late to get vaccinated.
Post-exposure? If you get pricked by a needle or have unprotected sex with someone who has HBV, get the vaccine and HBIG (a dose of antibodies) within 24 hours. The combination cuts infection risk dramatically. For unvaccinated people exposed to blood or bodily fluids, start the vaccine series immediately-even if you don’t know the source’s status.
Many people still don’t realize the vaccine is part of routine care. All newborns get it. All healthcare workers get it. But adults? Too often, it’s forgotten. If you’ve never been vaccinated, ask your doctor. It’s one shot that could save your liver for life.

What Happens After You Start Treatment
Treatment isn’t a cure-but it’s not a life sentence either. Most people take antivirals for years, sometimes for life. The goal isn’t to eliminate the virus completely (that’s still rare), but to keep it so suppressed your liver can heal. Regular monitoring every six months is key. You’ll need blood tests for HBV DNA, ALT, and HBsAg levels. Some clinics now also test for quantitative HBsAg-it helps predict if you might ever stop treatment safely.
Adherence matters. Missing doses can lead to resistance. TAF and ETV have high barriers to resistance, but skipping pills still risks the virus coming back stronger. If you’re struggling to take your meds daily, talk to your provider. There are pill boxes, phone reminders, and support programs designed to help.
Side effects? TAF is gentle on kidneys and bones. TDF needs monitoring. ETV has almost none. If you’re on TDF and notice swelling, fatigue, or changes in urination, get your kidney function checked. The same goes for bone pain-don’t ignore it.
What’s Next? The Future of HBV Treatment
Scientists are working on a cure. Not just control-actual elimination of the virus. Right now, there are at least 15 new drugs in clinical trials targeting the virus’s hidden DNA (cccDNA), which current antivirals can’t touch. Some aim to turn off the virus permanently. Others boost your immune system to fight it. Experts predict that by 2030, 30-40% of patients could achieve a functional cure-meaning the virus stays gone even after stopping meds.
But we can’t wait for science. Right now, we have what we need: testing, antivirals, and vaccines. The biggest barrier isn’t lack of tools-it’s lack of awareness. Millions still don’t know they’re infected. Many don’t get tested. Others stop treatment because they feel fine. That’s the trap.
What You Need to Do Now
- If you’ve never been tested for hepatitis B, ask for an HBsAg test today.
- If you’re positive, get your HBV DNA, ALT, and liver fibrosis checked.
- If your HBV DNA is above 2,000 IU/mL, talk to a liver specialist about starting treatment.
- If you’re pregnant and HBsAg-positive, ask about tenofovir at week 28.
- If you’ve never been vaccinated, get the three-shot series now.
- If you’re on antivirals, never skip a dose. Never stop without your doctor’s say-so.
Chronic hepatitis B doesn’t have to mean cirrhosis. It doesn’t have to mean cancer. With the right care, it can mean a long, healthy life. The tools are here. The knowledge is clear. What’s left is to act.


Gloria Ricky
i got tested last year after my cousin got diagnosed. turns out i was positive but had low viral load. doc said wait and watch, but i started reading up and now i’m on TAF. no side effects, feel way better. if you’re asymptomatic, don’t assume you’re fine. your liver doesn’t complain till it’s too late.
also, vaccine for adults? yes. just got mine for my mom. she’s 62. never had it. best $20 i ever spent.
Stacie Willhite
this post made me cry. not because i’m scared, but because i wish someone had told me this 10 years ago. i ignored my HBsAg positive result because i felt fine. now i have mild fibrosis.
if you’re reading this and you’ve been told ‘it’s not urgent’ - push back. your silence isn’t peace. it’s waiting for damage.
Jason Pascoe
as an Aussie GP, i’ve seen too many patients delay because they thought ‘if i don’t feel sick, i don’t need treatment.’ the shift in guidelines is long overdue. TAF is a game-changer for older patients and those with comorbidities.
also, pregnant women: please, get the tenofovir at 28. it’s not optional. it’s basic care.
Luke Trouten
there’s a quiet tragedy in medicine: we treat symptoms, not systems. hepatitis B exposes how fragmented our preventive care is.
the vaccine works. the drugs work. the testing is cheap. yet millions slip through because we don’t institutionalize awareness. we wait for crises. we don’t build systems of vigilance.
we’re not failing because we lack knowledge. we’re failing because we lack collective will.
Brad Ralph
so let me get this straight… we have a vaccine that’s 95% effective, antivirals that are safer than ibuprofen, and yet people still die because they ‘felt fine’? 🤡
also, who’s the genius who decided we should test for HBV DNA but not make it part of annual physicals? 🤔
Autumn Frankart
this is all a big pharma scam. the vaccine? it’s laced with graphene oxide. the antivirals? they’re designed to keep you dependent.
they don’t want you cured. they want you on meds forever. i stopped all meds and went on a lemon water + turmeric cleanse. my liver enzymes are normal now.
also, the WHO? controlled by Bill Gates. don’t trust them.
Skilken Awe
you people are so naive. you think TAF is safe? it’s just a rebranded TDF with a fancy name. the real issue? they’re not telling you about the cccDNA reservoir. no drug touches it. you’re all just delaying the inevitable.
and don’t get me started on the vaccine. it’s a Trojan horse for digital ID tracking. 100% corporate control.
you think you’re saving your liver? you’re just signing up for the surveillance state.
andres az
why are we even discussing this? the whole hepatitis B narrative is a distraction. real health crises are climate change, 5G, and mandatory vaccines.
if you’re worried about your liver, maybe stop eating processed carbs. no one talks about that.
also, HBV? probably just a lab leak. ask the CDC.
Steve DESTIVELLE
life is a river and the liver is its source. when the river flows clear the body thrives. when it turns murky the soul suffers.
we live in an age of fragments. we test DNA we measure enzymes we name diseases but we forget the essence.
the virus is not the enemy. the fear is. the fear that we are not enough. the fear that we must control.
healing comes not from pills but from stillness. from silence. from listening to the body without labels.
the vaccine? yes. the antivirals? perhaps. but the real cure is awakening.
you cannot heal what you refuse to feel.
Stephon Devereux
if you’re reading this and you’re on antivirals - you’re doing better than 90% of people with HBV. seriously. most don’t even know they’re infected.
you’re not alone. i’ve worked with hundreds. the ones who thrive? they show up. they track. they talk. they don’t wait for symptoms.
you’re not broken. you’re not doomed. you’re just one step ahead of the curve. keep going. you’ve got this.
Neha Motiwala
I CAN’T BELIEVE THIS IS HAPPENING. I JUST FOUND OUT MY BOYFRIEND IS POSITIVE AND HE NEVER TOLD ME. I’M SO ANGRY. I’M SO SCARED. WHAT IF HE GAVE IT TO ME? I NEED TO GET TESTED RIGHT NOW. I’M GOING TO THE CLINIC IN 20 MINUTES. WHY DIDN’T HE SAY SOMETHING? I’M SO ANGRY. I’M SO SCARED. I NEED HELP. PLEASE HELP ME.