Managing Steroid-Induced High Blood Sugar: A Practical Guide for Diabetes Patients
Steroid-Induced Hyperglycemia Calculator
Steroid Insulin Adjustment Calculator
This tool helps calculate insulin adjustments for patients on steroid therapy based on clinical guidelines. Always consult your healthcare provider before making medication changes.
When you're prescribed steroids for inflammation or autoimmune issues, your blood sugar can spike unexpectedly. For people with diabetes, this isn't just a minor inconvenience-it can lead to serious complications if not managed properly. Steroid-Induced Hyperglycemia (SIHG) is a condition where blood sugar levels rise due to steroid medications, affecting 20-50% of patients on glucocorticoid therapy. The good news? With the right adjustments to your diabetes medications, you can keep your blood sugar in a safe range.
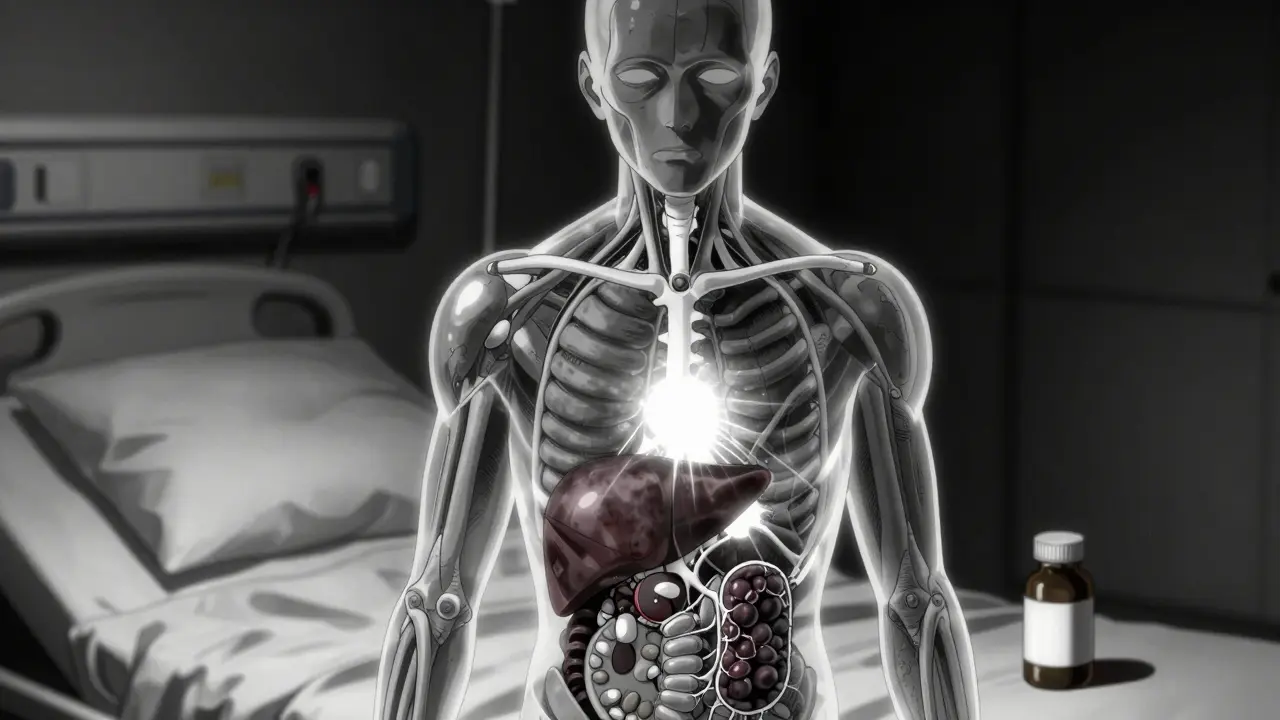
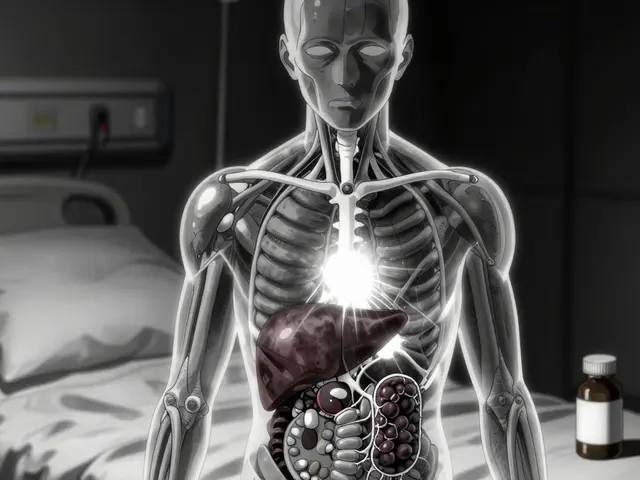
How Steroids Raise Blood Sugar
Steroids like prednisone and dexamethasone trigger hyperglycemia in three key ways. First, they make your body resistant to insulin, so glucose can't enter cells properly. Second, they force your liver to produce extra glucose through gluconeogenesis. Third, they damage pancreatic beta cells, reducing insulin production. This isn't theoretical-it happens in real time. A 2021 study in Diabetes Care found blood sugar spikes begin 4-8 hours after steroid dosing, peak at 24 hours, and last 3-4 days after stopping. For hospitalized patients, 40% develop SIHG, according to Umpierrez et al. (2021).
Adjusting Insulin for Steroid Therapy
When taking steroids, adjusting insulin is critical to manage blood sugar spikes. The right dose depends on the type and timing of your steroid medication. For rapid-acting insulin, start with 0.1 IU per kilogram of body weight at the time of steroid administration. If your blood sugar is between 11.1-16.7 mmol/L (200-300 mg/dL) before meals, add a correction dose of 0.04 IU/kg. For readings above 16.7 mmol/L, use 0.08 IU/kg. These numbers come from the 2021 practical guide published in PMC8157052.
The type of insulin matters too. Prednisone has a half-life of 18-36 hours, so NPH insulin-which lasts 12-36 hours-is ideal. For Dexamethasone, which lasts 36-72 hours, long-acting analogues like glargine or detemir work better. The Waterloo Wellington Diabetes Clinical Practice Guideline (2023) confirms this matching approach. If you previously needed 20 units of extra insulin for dexamethasone, start with just 10 units and adjust slowly-rushing increases hypoglycemia risk.
Managing Oral Diabetes Medications
Sulfonylureas like glipizide or glyburide are dangerous during steroid therapy. A 2021 Johns Hopkins Hospital study showed 27% of patients on sulfonylureas during steroid treatment required emergency visits for hypoglycemia, compared to 8% on insulin-only regimens. This happens because sulfonylureas keep forcing insulin release even as steroids taper, leading to dangerous low blood sugar. Safer alternatives include Metformin, which improves insulin sensitivity without causing lows, or GLP-1 Agonists like semaglutide, which slow digestion and reduce glucose production. DPP-4 inhibitors like sitagliptin also work well for outpatient management of mild hyperglycemia.

Monitoring Your Blood Sugar Safely
Continuous Glucose Monitoring (CGM) is recommended for at least 48 hours during high-dose steroid therapy. This device tracks your blood sugar in real-time, helping you stay within the target range of 3.9-10.0 mmol/L (70-180 mg/dL). The JBDS 2021 guideline emphasizes that CGM reduces the risk of dangerous highs and lows compared to traditional fingerstick checks. For patients not using CGM, check blood sugar at least four times daily-before meals and at bedtime. During dose changes or hyperglycemia, monitor every 2-4 hours. A 2023 survey by the American Association of Clinical Endocrinology found that 68% of patients struggled to adjust insulin doses without real-time data, making CGM a game-changer for safety.
Tapering Steroids: Avoiding Dangerous Mistakes
The most common error in SIHG management? Failing to reduce insulin as steroids decrease. Dr. David Kendall, Chief Scientific Officer of Diabetes UK, warns: "Failure to reduce diabetes medications as steroids taper is the most common clinical error, leading to preventable hypoglycemia in 30-40% of cases." For every 5mg reduction in prednisone, lower your basal insulin by 10-15%. With dexamethasone, reduce insulin doses starting 3-4 days before the steroid dose drops, since its effects linger longer. Always check blood sugar more frequently during tapering-every 2 hours for the first 48 hours. A Reddit user named "Type1Since99" shared: "When tapering to 20mg prednisone, my endocrinologist didn't reduce my insulin fast enough and I had 3 hypos in 2 days." This is exactly why timing matters.
Real-World Scenarios and Common Errors
Consider two real cases. Sarah, a type 2 diabetes patient on 30mg prednisone daily, started with 0.1 IU/kg rapid-acting insulin at steroid dose time. Her morning blood sugar was 18 mmol/L (324 mg/dL), so she added 0.08 IU/kg correction. By day 3, her fasting glucose stayed above 11.1 mmol/L, so her basal insulin was increased by 15%. When prednisone was tapered to 20mg, she reduced basal insulin by 12% daily until her levels stabilized. Contrast this with Mark, who kept his full insulin dose while tapering dexamethasone. He experienced severe hypoglycemia (blood sugar 2.1 mmol/L) twice, requiring emergency treatment. A 2022 quality improvement study at Massachusetts General Hospital found 37% of SIHG cases involved this exact mistake-failing to reduce insulin during steroid tapering.
Frequently Asked Questions
What is steroid-induced hyperglycemia?
Steroid-induced hyperglycemia (SIHG) occurs when glucocorticoid medications like prednisone or dexamethasone cause blood sugar levels to rise. This happens because steroids increase insulin resistance and boost liver glucose production. According to a 2021 review in the Journal of Clinical Endocrinology & Metabolism, 20-50% of patients on moderate to high-dose steroids develop this condition.
How soon after taking steroids does blood sugar rise?
Blood sugar typically starts rising 4-8 hours after taking steroids, peaks at 24 hours, and remains elevated for 3-4 days after stopping. This timing varies by steroid type-prednisone acts faster than dexamethasone due to its shorter half-life. Always check your blood sugar before and after taking steroids to catch spikes early.
Should I stop taking my diabetes meds when on steroids?
Never stop diabetes medications without consulting your doctor. For insulin, you'll likely need to increase doses during steroid therapy but reduce them as steroids taper. For oral meds like sulfonylureas, you may need to switch to safer alternatives. A Johns Hopkins study found 27% of patients on sulfonylureas during steroid treatment had emergency hypoglycemia, while those on insulin-only regimens had only 8% risk. Always work with your healthcare team to adjust safely.
Is continuous glucose monitoring necessary?
Yes, for high-dose steroid therapy. The JBDS 2021 guideline recommends continuous glucose monitoring (CGM) for at least 48 hours. Real-time data helps you see how steroids affect your blood sugar and adjust insulin precisely. Patients using CGM during steroid treatment spend 70% more time in the safe blood sugar range (3.9-10.0 mmol/L) compared to those using only fingerstick checks. If you can't access CGM, check blood sugar every 2-4 hours during steroid use and tapering.
What's the biggest mistake people make with SIHG?
The most common error is failing to reduce insulin doses as steroids taper. This causes preventable hypoglycemia in 30-40% of cases, according to Diabetes UK. For example, if you take 40mg prednisone for 10 days and taper down to 5mg over 5 days, you should reduce your insulin dose gradually during the tapering phase-not wait until the steroid is completely stopped. Always coordinate dose reductions with your healthcare provider to match the steroid's half-life and your blood sugar trends.


Tola Adedipe
Steroid-induced hyperglycemia is no joke. I've managed many patients on this, and the key is adjusting insulin early. For prednisone, start with 0.1 IU/kg at dosing time. If blood sugar is high, add correction doses. But don't forget to taper insulin when steroids are reduced-this is where most mistakes happen. Trust me, I've seen cases where people didn't adjust and ended up in hypoglycemia. Always check your numbers.
Ritu Singh
As someone who's worked with diabetic patients in India, I've seen how steroids can really mess with blood sugar control. The key is adjusting insulin early. Sulfonylureas like glipizide are dangerous during steroid therapy-I've had patients on them end up in emergency for hypoglycemia. Switching to metformin or GLP-1 agonists is safer. Always consult your doctor before making changes. This info could save lives.
Mark Harris
Been on prednisone for my autoimmune thing, and my sugar went through the roof. Adjusted my insulin as per the guide-0.1 IU/kg at dosing time-and it's been way better. Also, the part about tapering insulin when reducing steroids is crucial. I almost had a low last week because I didn't adjust. Don't skip the CGM either-real-time data is a game changer. Thanks for this!
Ariel Edmisten
Adjust insulin early, monitor closely, taper carefully.
Niel Amstrong Stein
Hey folks, steroids and blood sugar? Total chaos 😅. But this guide breaks it down perfectly. The part about dexamethasone lasting longer-36-72 hours-means you need to adjust insulin earlier than you think. I've been there, done that, and the CGM saved me from a few lows. 🙌 Also, don't forget to check your numbers during tapering. It's a marathon, not a sprint. Stay safe, everyone!
Paula Sa
It's fascinating how steroids disrupt insulin sensitivity and glucose production. This guide really highlights the importance of tailored insulin adjustments. I've seen patients struggle with tapering, but gradual reductions prevent hypoglycemia. Always work with your healthcare team-this isn't something to handle alone. Knowledge is power, and this information is invaluable.
Mary Carroll Allen
Steroids can totally wreck your blood sugar if you dont adjust insulin. I had a friend who went into a hypo because they didnt reduce insulin when tapering prednisone. The numbers in this guide are spot on-0.1 IU/kg for rapid-acting. But dont forget to monitor constantly. CGM is a lifesaver. I almost died because I ignored this. Please take this seriously!
Joey Gianvincenzi
Proper management of steroid-induced hyperglycemia is imperative for patient safety. The data presented here is unequivocally accurate regarding insulin adjustments and monitoring protocols. Failure to adhere to these guidelines results in preventable complications. This information must be disseminated widely to healthcare professionals globally. The stakes are simply too high to ignore.
Amit Jain
I've been on prednisone for years and never had issues. Maybe the guide is overcomplicating things. Some people's bodies handle steroids fine.
Sarah B
adjust insulin or suffer
Ashley Hutchins
people who dont adjust insulin when on steroids are just being reckless. this is basic diabetes management. they should know better
Lakisha Sarbah
Hey, this is really helpful. I've been managing my diabetes and had to deal with steroids. The part about metformin being safer than sulfonylureas makes sense. I switched and had no issues. Just remember to check your blood sugar often. Thanks for sharing!
Eric Knobelspiesse
Interesting how steroids trigger hyperglycemia through multiple pathways. But let's think deeper: is it the steroids themselves, or the body's response? Maybe we should question the underlying mechanisms. Also, the numbers here are good, but real-world application varies. Always consult your doctor-this is just one perspective.
Heather Burrows
Not sure if this is the best approach. I've seen cases where adjusting insulin too early caused issues. Maybe it's better to monitor first before changing doses. This guide seems a bit too prescriptive for my taste.
Savannah Edwards
As someone who's been managing diabetes for years and has worked with diverse communities, I've seen firsthand how steroids can really throw a wrench into blood sugar control. It's not just about the immediate spike-it's the ripple effect that lasts days after stopping the steroids. The guide here is spot on, especially the part about how steroids make your body insulin resistant and force the liver to produce more glucose. I remember a patient in my clinic who was on prednisone for a severe autoimmune flare-up. They didn't adjust their insulin properly, and their blood sugar soared to dangerous levels. It took days to stabilize, and they had to be hospitalized. The key takeaway is that timing matters. For example, prednisone's half-life is 18-36 hours, so NPH insulin works best for that. But dexamethasone sticks around for 36-72 hours, so long-acting analogues like glargine are better. Also, the part about sulfonylureas being dangerous during steroid therapy is critical. I've seen multiple cases where patients on glipizide or glyburide had severe hypoglycemia because the steroids were tapering but the sulfonylureas kept pushing insulin. Switching to metformin or GLP-1 agonists is a safer bet. Continuous glucose monitoring is a game-changer too. It's not just about checking four times a day; real-time data lets you catch spikes before they become emergencies. During steroid therapy, I recommend checking every two hours for the first 48 hours. The JBDS 2021 guideline really emphasizes this. I've also noticed that many people forget to reduce insulin as steroids are tapered. It's a common mistake, and it leads to preventable lows. For every 5mg reduction in prednisone, lowering basal insulin by 10-15% is a good rule of thumb. But you have to monitor closely. Patients have experienced severe hypoglycemia during steroid tapering when insulin wasn't adjusted properly. This is exactly why coordination with your healthcare provider is so important. Don't just follow the numbers blindly; listen to your body and adjust accordingly. And for those of us in different cultural contexts, it's crucial to adapt these guidelines to local resources. Not everyone has access to CGMs, so frequent fingerstick checks are essential. The takeaway is clear: stay informed, communicate with your doctor, and don't skip the monitoring. This guide is a lifesaver for anyone on steroids with diabetes.