Medication-Related Blood Clots: How to Recognize and Prevent Them

Medication-Related Blood Clot Risk Calculator
This calculator helps you understand your risk of developing blood clots related to medications. Based on the Caprini Risk Assessment Model, it identifies key risk factors and provides personalized recommendations.
How this works
Answer the questions below to assess your risk level. The tool will calculate a risk score (0-10) and provide specific recommendations based on your answers.
Every year, around 900,000 Americans develop dangerous blood clots. About one-third of those cases are linked to medications-not bad luck, not genetics alone, but drugs you’re taking to treat something else. That’s the hard truth. Many people don’t realize that pills they swallow for birth control, menopause, or cancer can silently turn their blood into a ticking time bomb. The good news? These clots are often preventable-if you know what to watch for and what to ask your doctor.
What Medications Can Cause Blood Clots?
Not all drugs cause clots, but some are well-documented triggers. The biggest culprits fall into three categories: hormones, cancer treatments, and certain anti-inflammatory drugs.Combined hormonal contraceptives-those with estrogen and progestin-are the most common offender. If you’re on the pill, patch, or ring, your risk of deep vein thrombosis (DVT) goes up 3 to 5 times compared to someone not using them. Third-generation pills with desogestrel or gestodene are even riskier than older ones with levonorgestrel. The reason? Estrogen boosts clotting factors like Factor VII and lowers natural anticoagulants like Protein S. Your blood thickens without you feeling it.
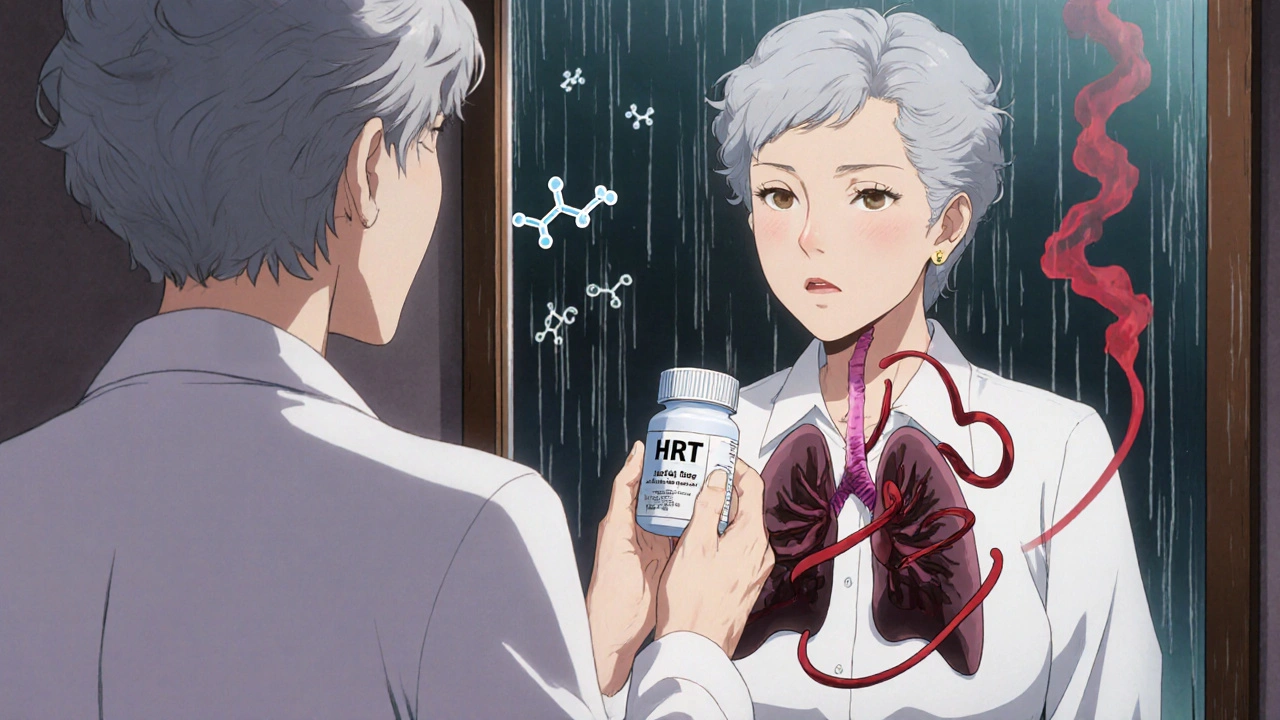
Hormone replacement therapy (HRT) for menopause carries a similar risk-2 to 3 times higher for women on estrogen plus progesterone. The risk spikes after age 60. Many women assume HRT is safe because it’s prescribed by a doctor, but the clot risk doesn’t disappear just because it’s for symptom relief.
Cancer treatments are another major source. Chemotherapy drugs like cisplatin can increase clot risk by 4 to 7 times. Tamoxifen, used for breast cancer, raises it by 2 to 3 times. Even prostate cancer drugs that lower testosterone can nudge your clotting balance toward danger. This isn’t rare-it’s expected. Doctors now use the Khorana Score to predict which cancer patients need preventive blood thinners before treatment even starts.
And don’t forget the less obvious ones. Some anti-inflammatory drugs, especially long-term NSAIDs, can interfere with platelet function and vessel lining, creating a slow-burning clot risk. Even some antibiotics and antidepressants have been linked in rare cases.
How to Spot a Medication-Induced Blood Clot
Symptoms don’t always come with a warning sign. But if you’ve started a new medication in the last 3 to 6 months and suddenly feel off, pay attention.For deep vein thrombosis (DVT), look for:
- Swelling in one leg-usually the calf, not both
- Pain that feels like a cramp or soreness, doesn’t go away with stretching
- Red or bluish skin over the area
- A warm spot on your leg that feels hotter than the other side
For pulmonary embolism (PE), which happens when a clot travels to the lungs:
- Sudden shortness of breath-no exercise, no asthma
- Chest pain that gets worse when you breathe in deeply
- Rapid heartbeat with no obvious cause
- Dizziness, fainting, or feeling like you’re going to pass out
These symptoms often show up within the first few months of starting a high-risk drug. About 60% of medication-related clots happen in that window. If you’re on birth control and suddenly feel winded climbing stairs, or your calf aches for days without injury-don’t brush it off. Call your doctor. Don’t wait.
Diagnosis isn’t guesswork. Doctors use a D-dimer blood test (which detects clot breakdown products), ultrasound for leg clots, and CT scans for lung clots. But here’s the catch: ultrasounds miss about 5-10% of DVTs. If your symptoms are strong but the scan is clear, insist on further testing. False negatives happen.
How to Prevent Medication-Related Clots
Prevention isn’t just about popping a pill. It’s a mix of behavior, monitoring, and smart choices.1. Know your risk before you start. If you have a family history of clots, a personal history, or a known clotting disorder like Factor V Leiden (present in 5% of Caucasians), estrogen-containing medications are often a hard no. The American Heart Association says these patients should avoid them entirely. Ask your doctor to run a simple blood test if you’re unsure.
2. Use compression stockings if you’re at risk. If you’re hospitalized, recovering from surgery, or on long-term bed rest, graduated compression stockings (15-20 mmHg at the ankle) can cut your clot risk by half. They must fit perfectly-measured at three points on your leg. If they’re too loose, they do nothing. Too tight? You risk skin damage. Replace them every 3-6 months. Elasticity fades fast.
3. Move, even when you can’t walk. If you’re stuck on a flight longer than 4 hours, walk every 60 to 120 minutes. If you can’t get up, do seated calf raises: lift your heels 10 times every 30 minutes. Hydrate with 8-10 ounces of water every hour. Alcohol and caffeine dehydrate you-skip them. These simple steps reduce travel-related clots by 30%.
4. Consider blood thinners if your doctor says so. For high-risk patients-like those undergoing surgery or cancer treatment-low molecular weight heparin (LMWH), such as enoxaparin, is the gold standard. It’s injected once a day and reduces clot risk by 60-70%. For outpatient use, direct oral anticoagulants (DOACs) like rivaroxaban or apixaban are easier-no blood tests, fixed doses. But they carry a slightly higher bleeding risk than LMWH. Never start these on your own. They require careful monitoring.
5. Track your kidney function. DOACs are cleared by your kidneys. If your creatinine clearance drops below 30 mL/min, the drug builds up in your system. Get your kidney function checked every 3-6 months if you’re on one. Most people forget this. Don’t be one of them.
What Your Doctor Should Be Doing
Doctors aren’t always perfect. Studies show only 40% of high-risk patients get the right prevention. Why? Many still underestimate the clot risk compared to bleeding risk.For cancer patients, the American Society of Clinical Oncology (ASCO) says: use the Khorana Score at diagnosis and every month. If your score is 2 or higher, you should get LMWH. If your doctor hasn’t mentioned this, ask. It’s standard of care.
For women considering birth control or HRT, your doctor should run the Caprini Risk Assessment Model. It checks for obesity, age, smoking, family history, and more. If you’re over 35 and smoke? Don’t take estrogen. Period. The FDA now requires black box warnings on all estrogen pills for this reason. If your prescriber doesn’t mention it, they’re not following guidelines.
And if you’ve had a previous clot? You’re at higher risk for another. Your doctor should be thinking long-term. Stopping anticoagulants too soon is a common mistake. For medication-induced clots, guidelines often recommend continuing treatment for at least 3-6 months after stopping the drug.

What’s New in Prevention
Science is catching up. Researchers are testing new drugs like asundexian, a factor XI inhibitor that reduces clots by half without increasing bleeding. Early results are promising. It could be a game-changer for cancer patients who can’t tolerate traditional blood thinners.Genetic testing for clotting disorders is also getting faster. Panels that check for Factor V Leiden, prothrombin mutation, and protein C/S deficiencies now take 5-7 days instead of weeks. But most doctors still don’t order them routinely. If you’ve had a clot with no clear cause, push for it. It changes your lifelong medication choices.
The market for anticoagulants is booming-projected to hit $22.7 billion by 2028. DOACs now make up 65% of sales. That’s because they’re easier to use. But ease doesn’t mean safety without supervision. You still need to know your numbers, your symptoms, and your risks.
Bottom Line: Take Control
Medication-related blood clots aren’t accidents. They’re predictable. They’re preventable. But only if you’re informed.Before starting any new hormone therapy, cancer drug, or long-term NSAID, ask:
- Is there a clot risk with this medication?
- Do I have any personal or family risk factors?
- Should I be on a blood thinner or compression stockings?
- What symptoms should I watch for-and when do I call you?
Don’t assume your doctor knows your full history. Bring a list of all medications, supplements, and past medical events. Write down your symptoms. Ask for the Khorana or Caprini score if it applies. You’re not being difficult-you’re being smart.
Clots don’t announce themselves. They sneak in. But you can stop them-if you know what to look for and who to ask.
Can birth control pills really cause blood clots?
Yes. Combined oral contraceptives with estrogen increase the risk of blood clots by 3 to 5 times compared to non-users. Third-generation pills (with desogestrel or gestodene) carry a 1.5 to 2 times higher risk than second-generation pills (with levonorgestrel). The risk is highest in the first 3 to 6 months after starting. Women over 35 who smoke, have obesity, or a family history of clots should avoid estrogen-containing options entirely.
What are the first signs of a blood clot from medication?
For a leg clot (DVT), look for sudden swelling, pain like a cramp, red or discolored skin, and warmth in one leg. For a lung clot (PE), watch for sudden shortness of breath, chest pain when breathing deeply, rapid heartbeat, or fainting. These usually appear within 3 to 6 months of starting a high-risk medication. If you notice any of these, contact your doctor immediately-don’t wait.
Do I need to take blood thinners if I’m on hormone therapy?
Not everyone does. But if you’re over 60, obese, have a history of clots, or have inherited clotting disorders like Factor V Leiden, your doctor should consider preventive anticoagulants. For most healthy women under 60 on HRT, the risk is low enough that routine blood thinners aren’t recommended. But you should still be screened for risk factors before starting.
Can I still fly if I’m on a medication that increases clot risk?
Yes, but you need to take extra steps. Walk every 60 to 120 minutes during flights longer than 4 hours. If you can’t walk, do seated calf raises (10 reps every 30 minutes). Drink 8-10 ounces of water every hour. Avoid alcohol and caffeine. Wear properly fitted compression stockings (15-20 mmHg). These steps reduce travel-related clot risk by about 30%.
How long should I stay on blood thinners after a medication-induced clot?
Guidelines recommend continuing anticoagulants for at least 3 to 6 months after stopping the medication that caused the clot. If you have ongoing risk factors-like cancer or a genetic clotting disorder-you may need longer treatment, sometimes indefinitely. Stopping too early increases your chance of a second clot. Always follow your doctor’s advice based on your individual risk profile.
Are there natural ways to prevent blood clots from medications?
Movement, hydration, and compression stockings are proven non-drug methods. But there’s no proven natural supplement that prevents medication-induced clots. Garlic, ginger, and fish oil may have mild blood-thinning effects, but they’re not strong enough to replace medical prevention. Never stop prescribed anticoagulants to try natural remedies-this can be deadly. Always talk to your doctor before adding supplements.
Medication-related blood clots are serious-but they’re not inevitable. Knowledge is your best defense. Ask questions. Track symptoms. Push for screening. Your life depends on it.



Ashley Miller
Of course the pharmaceutical companies love this stuff. They make billions off your fear and your prescriptions. They don't care if you get a clot-they care if you keep buying pills. The FDA? Totally in bed with them. Black box warnings? Just a PR stunt to make you feel safe while they keep raking it in. You think they'd rather you live or keep you hooked? 😏
Sherri Naslund
so like… if you’re on birth control and you dont want to die you just… dont take it? but then you get pregnant and that’s worse? what even is life anymore?? also my cousin had a clot after her hrt and the doctor just said ‘oh well’ and gave her more pills. like. what??
Martin Rodrigue
While the article presents a clinically accurate overview of medication-associated thrombotic risk, it fails to contextualize absolute versus relative risk adequately. The 3- to 5-fold increase in DVT risk with combined hormonal contraceptives translates to approximately 3–9 cases per 10,000 woman-years, compared to 1–5 per 10,000 in non-users. This is statistically significant but remains low in absolute terms. Risk stratification, not fear-based avoidance, should guide clinical decisions.
Mary Follero
This is SO important and I’m so glad someone laid it out like this. I had a pulmonary embolism after starting birth control and no one warned me. I thought I was just tired. If I’d known about the symptoms-especially that chest pain when breathing in-I would’ve gone to the ER weeks earlier. Please, if you’re on any hormone stuff, learn the signs. Your life isn’t worth gambling with ignorance. Share this with your friends. Seriously.
Will Phillips
They want you scared so you’ll take more pills. Clots? Yeah. But what about the millions of women who take birth control and never have a problem? The system is rigged. Doctors are paid by Big Pharma. The government wants you docile. You think they want you healthy? No. They want you dependent. You think your doctor cares? They’re paid per script. Wake up. This isn’t medicine-it’s control. And they’re using your fear to sell it.
Danielle Mazur
The Khorana Score is underutilized in oncology practice, and this is a systemic failure. The 2023 ASCO guidelines are unequivocal: patients with a score ≥2 should receive prophylactic LMWH. Yet, in a 2022 survey of 1,200 oncologists, only 31% reported routinely applying the score. This is not negligence-it is institutional inertia. Until reimbursement models incentivize thromboprophylaxis, this gap will persist. Patients must advocate for standardized risk assessment.
Freddy Lopez
It’s interesting how we treat medication risks like they’re all-or-nothing. We either fear them or ignore them. But maybe the real issue is that we’ve outsourced our health to systems that don’t prioritize our autonomy. What if we treated medication like a conversation-not a command? What if doctors listened more and prescribed less? Maybe then we’d stop seeing clots as ‘side effects’ and start seeing them as signals.
Brad Samuels
I just want to say thank you for writing this. My mom had a clot after HRT and she didn’t tell anyone for weeks because she didn’t want to ‘bother’ anyone. She’s fine now, but she says she wishes she’d known sooner. This article could save someone’s life. I’m sharing it with my whole family. You’re doing good work.
Arun Mohan
Let me be frank-this is why Western medicine is a joke. You people swallow pills like candy and then act shocked when your blood turns to glue. In India, we use turmeric, neem, and yoga. No pills. No fear. Just balance. You think a lab test can replace ancient wisdom? Please. You’re drowning in data while starving for truth.
Tyrone Luton
It’s funny how people treat blood clots like they’re some newfangled horror story. People have been dying from clotting since the 1800s. The difference now? We have the tools to stop it. But we don’t. Why? Because convenience beats caution. You want to fly, you want to be thin, you want to be ‘normal’-so you take the pill. Then you cry when your body rebels. The body doesn’t lie. You just stopped listening.
Jeff Moeller
Just one thing-compression stockings aren’t magic. They have to fit right. My sister bought some off Amazon and they were too loose. She still got a clot. Measure your leg. Three points. Ankle calf thigh. Don’t guess. And if your doc says ‘they’re optional’-push back. They’re not optional if you’re high risk
Herbert Scheffknecht
Think about it-every time you take a pill, you’re making a deal with your biology. You’re saying ‘I’ll override your natural balance for my convenience.’ And then you’re shocked when it fights back. The clot isn’t the enemy. The assumption that you can control your body without consequence is. Maybe the real medication is awareness. Maybe the real treatment is humility.
Jessica Engelhardt
As an American woman who’s had two clots from birth control, I’m tired of this being framed as ‘personal responsibility.’ My doctor didn’t ask about my family history. The pill was just handed to me like a candy. Now I’m on DOACs for life. And guess what? Insurance won’t cover the new asundexian trials. They’re too expensive. So yeah, knowledge is power-but only if you’ve got the money to pay for it. This isn’t prevention-it’s privilege.
rachna jafri
They say ‘ask your doctor’ like doctors are gods. I asked mine and he said ‘you’re fine’ while I was clutching my leg screaming. Then he wrote me a new prescription for a different pill. I’m not paranoid-I’m just not stupid. They don’t want you to know that 80% of these clots happen because doctors skip the screening. They’re too busy. Too rushed. Too paid by the bottle. Wake up. This isn’t medicine. It’s assembly-line poisoning.