Drug-Induced Kidney Failure: How to Recognize and Prevent It

Kidney Function Calculator
This tool calculates your estimated glomerular filtration rate (eGFR) using the CKD-EPI formula. Your eGFR helps determine your kidney function and guides medication safety decisions. Based on your result, we'll show appropriate precautions related to drug-induced kidney injury.
What Is Drug-Induced Kidney Failure?
Drug-induced kidney failure, more accurately called drug-induced acute kidney injury (DI-AKI), happens when certain medications suddenly damage your kidneys. It’s not a slow, gradual decline-it’s a sharp drop in kidney function that can occur in just hours or days. This isn’t rare. About 1 in 5 cases of acute kidney injury in hospitals comes from medications. In intensive care units, that number jumps to nearly 6 in 10.
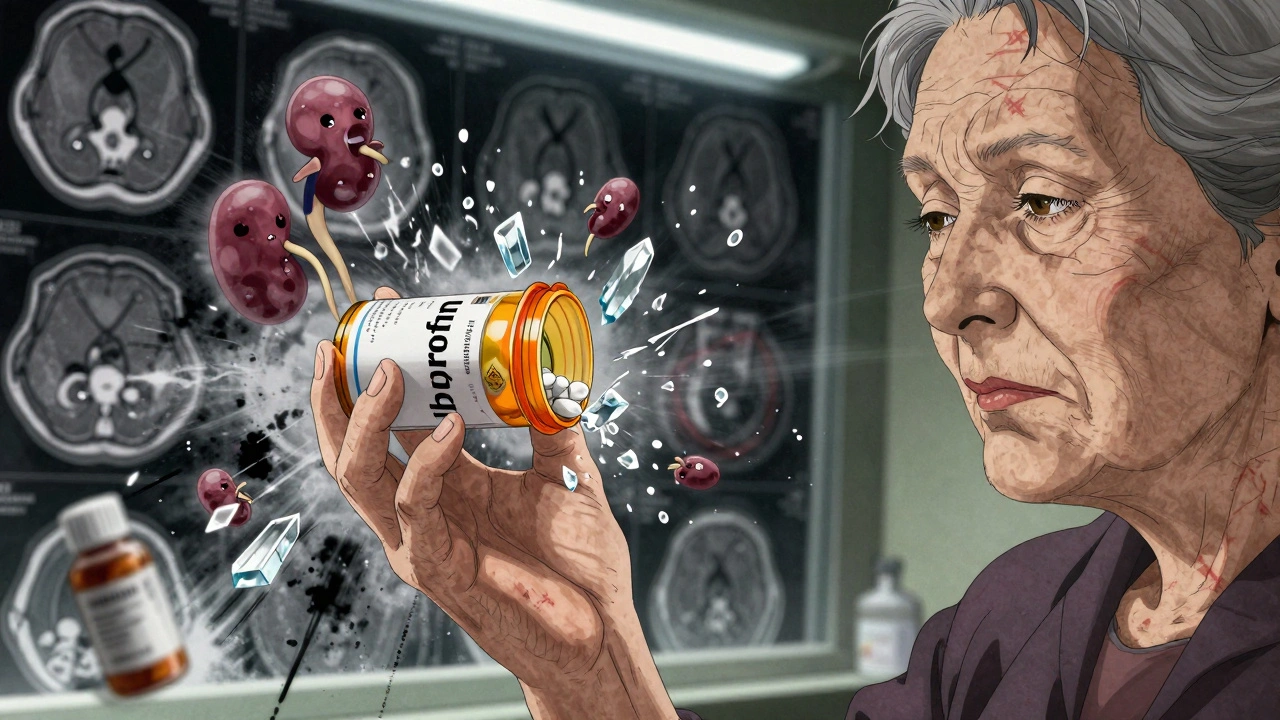
It’s not just about overdoses. Even common drugs like ibuprofen, antibiotics, or contrast dyes used in imaging scans can trigger it-especially if you already have kidney issues, are older, or are taking multiple medications. The damage can be reversible if caught early. But if missed, it can lead to permanent kidney damage, dialysis, or even death.
How Do You Know It’s Happening?
The scary part? DI-AKI often has no symptoms at first. You might feel fine, or just a little tired. That’s why doctors rely on blood tests. The key sign is a rise in serum creatinine. According to the latest guidelines from KDIGO (2024), kidney injury is confirmed if:
- Your creatinine increases by 0.3 mg/dL or more within 48 hours, or
- It jumps by 50% or more from your baseline, or
- You produce less than 0.5 mL of urine per kilogram of body weight for 6 hours straight.
Some drug reactions come with clearer signs. For example, if you’re on a proton pump inhibitor (like omeprazole) or an antibiotic and develop a fever, rash, or joint pain after 7-14 days, you could be having acute interstitial nephritis. That’s one of the most common drug-induced kidney injuries.
Other types show up fast. If you take acyclovir or sulfadiazine and your urine becomes cloudy or you’re in pain when you pee, it might be crystal-induced injury. These crystals form when the drug isn’t flushed out properly-especially if you’re dehydrated.
Which Drugs Are Most Likely to Cause It?
Not all drugs are equal when it comes to kidney risk. Some are far more dangerous than others. Here are the top offenders based on real-world data from the FDA and clinical studies:
- NSAIDs (ibuprofen, naproxen, diclofenac): Cause 3-5% of all hospital AKI cases. Risk spikes to 15-20% in older adults or those with existing kidney disease.
- Antibiotics: Vancomycin and piperacillin-tazobactam are top culprits. Vancomycin alone causes 2.7 cases per 1,000 patient-years.
- Proton pump inhibitors (PPIs): Used for heartburn, but linked to interstitial nephritis in up to 15% of drug-induced AKI cases.
- Contrast dyes: Used in CT scans and angiograms. About 1 in 10 hospital-acquired AKI cases comes from these.
- Antivirals: Acyclovir and tenofovir can form crystals in the kidneys, especially if you’re not drinking enough water.
And here’s something many don’t realize: it’s not just one drug. Taking five or more medications at once-called polypharmacy-makes you 3.7 times more likely to develop DI-AKI. That’s why medication reviews are critical.
Who’s Most at Risk?
You’re at higher risk if you have:
- Chronic kidney disease (eGFR under 60 mL/min/1.73m²)
- Diabetes or high blood pressure
- Heart failure or liver disease
- Are over 65 years old
- Are dehydrated or on diuretics
- Take NSAIDs regularly, even over-the-counter ones
One patient story from the American Kidney Fund tells it clearly: JohnD_72 took ibuprofen for 10 days after dental surgery. He already had stage 3 chronic kidney disease. His creatinine shot up from 1.8 to 4.2 in three days. His doctor didn’t connect the dots for five days. He ended up hospitalized for a week.
On the flip side, MaryK_65 had her cardiologist switch her from naproxen to acetaminophen after her eGFR dropped to 52. Her kidney function stabilized in two weeks. The difference? Someone caught it early.
How to Prevent It
The good news? Up to 70% of drug-induced kidney injuries are preventable. Here’s how:
1. Know Your Baseline
Before starting any new medication-especially antibiotics, NSAIDs, or contrast dyes-ask for a simple blood test: serum creatinine. From that, your doctor can calculate your eGFR. If it’s below 60, your kidneys are already impaired. That changes everything.
2. Avoid NSAIDs If You Have Kidney Issues
NSAIDs are the #1 preventable cause of kidney injury. If your eGFR is under 60, avoid them completely. Use acetaminophen instead for pain. Studies show switching cuts AKI risk by 47%.
3. Hydrate Before and After Imaging Scans
If you’re getting a CT scan with contrast, drink water before and after. For high-risk patients (those with diabetes, kidney disease, or heart failure), hospitals now use IV fluids-usually normal saline-at 1.0-1.5 mL per kg per hour for 6-12 hours before and after the scan. This lowers risk by nearly 30%.
4. Ask About Dose Adjustments
Many drugs need lower doses if your kidneys aren’t working well. Ask your doctor: “Does this medicine need to be adjusted for my kidney function?” Don’t assume they know. A 2022 study of over 286,000 patients found that computerized alerts in electronic health records reduced wrong dosing by 63%.
5. Watch for Warning Signs After Starting a New Drug
If you start a new medication and feel unusually tired, swollen, or stop peeing normally, speak up. Fever, rash, or joint pain? That could be interstitial nephritis. Don’t wait. Call your doctor immediately.
6. Get a Medication Review
Take all your pills-prescription, OTC, supplements-to your pharmacist or doctor every 6 months. They can spot dangerous combinations. For example, taking an NSAID with a diuretic and an ACE inhibitor (the “triple whammy”) is a recipe for kidney failure.
What Happens After Diagnosis?
If DI-AKI is caught early, stopping the drug is often enough. Kidneys can bounce back in days or weeks. But if the injury is ignored, scarring can set in. That’s when it becomes chronic kidney disease-and that’s permanent.
For crystal-induced injury, doctors may give IV fluids and alkalinize the urine (raise pH above 7.1) to dissolve crystals. For interstitial nephritis, steroids might be needed. But the first step is always: stop the drug.
One of the biggest mistakes? Continuing the drug anyway. The NCEPOD 2019 report found that 38% of AKI cases happened because doctors kept giving nephrotoxic drugs even after kidney damage showed up.

New Tools Are Helping
Technology is stepping in. In 2024, the FDA approved the first AI-powered system called Dosis Health designed to flag high-risk prescriptions before they’re written. In trials, it cut DI-AKI cases by 41%. Hospitals using it are seeing fewer errors and faster interventions.
Also, newer guidelines now require doctors to check kidney function before prescribing 12 high-risk drug classes. That’s a big shift from the past, where many just assumed kidneys were fine.
What You Can Do Today
You don’t need to be a doctor to protect your kidneys. Here’s your simple action plan:
- Know your eGFR. If you don’t know it, ask for your last creatinine test.
- Stop taking NSAIDs if you have any kidney issues-even if they’re “just” over-the-counter.
- Drink water before and after any imaging scan.
- Keep a list of all your medications and review it with your pharmacist every 6 months.
- If you feel worse after starting a new drug, don’t ignore it. Call your doctor.
Why This Matters
Drug-induced kidney injury isn’t just a medical issue-it’s a financial one. In the U.S., each episode costs an average of $18,450. That’s more than double the cost of a hospital stay without kidney injury. And 76% of these cases are preventable.
Every time a doctor misses a warning sign or a patient keeps taking ibuprofen without knowing their kidney status, someone suffers needlessly. But with better awareness, better tools, and better communication, we can stop this before it starts.



Stacy Tolbert
I had no idea ibuprofen could wreck your kidneys like that. My mom’s been taking it daily for her arthritis and her eGFR dropped last month. I’m dragging her to the pharmacist this week to review everything. Scary how easy it is to accidentally kill your own organs with OTC stuff.
Also, why do doctors just assume you know your own numbers? I had to beg for my creatinine results last year. It’s like they think we’re all medical students.
Ronald Ezamaru
For anyone reading this and thinking 'I’m fine, I don’t take NSAIDs' - check your supplements. Turmeric extracts, green tea extracts, and even some weight-loss pills have hidden nephrotoxins. A 2023 study in JAMA Nephrology found 22% of DI-AKI cases in older adults came from herbal products labeled 'natural' and 'safe.'
Also, hydration isn’t just about drinking water. Electrolyte balance matters too. If you’re on diuretics or sweating a lot, plain H2O isn’t enough. Consider oral rehydration salts if you’re high-risk. Simple, cheap, life-saving.
Ryan Brady
Ugh. Another liberal medical scare piece. People are dying from opioids but you’re worried about ibuprofen? Grow up. My grandpa took naproxen for 40 years and lived to 92. If your kidneys are trash, maybe don’t be 70 and still eating Twinkies and watching Netflix all day.
Also, AI systems? Really? We’re letting robots decide what drugs we get now? Next they’ll be telling us when to breathe.
Also, I’m not drinking water before a CT scan. I’m not a lab rat.
USA. First. Always.
:)
Raja Herbal
So let me get this straight - in America, you need a PhD to know you shouldn’t take Advil after 60? And the solution is not to fix the system, but to make patients become pharmacists on top of their 9-to-5 jobs? Cute.
Meanwhile in India, we just tell people: if you’re old, don’t take pills unless you’re dying. Works better than AI alerts. Also, our doctors don’t charge $200 to check creatinine. They check it for free while you wait for the chai.
Keep your tech. We’ll keep our common sense.
(Also, yes, I’ve seen 3 people on dialysis from PPIs. Same story. Always.)
Iris Carmen
OMG I just realized I’ve been taking meloxicam for my back and I have stage 2 CKD 😭 I’m literally deleting my ibuprofen app right now. Also why did no one ever tell me to ask for eGFR? I thought creatinine was just for liver stuff??
Also, I just drank a liter of water before my MRI. Hope I don’t pee my pants during the scan lol.
Also, my pharmacist is gonna kill me when I show her my pill bottle. It’s like a pharmacy exploded in there.
Rich Paul
Let’s cut through the noise. DI-AKI is just a subset of iatrogenic injury, and the real issue is pharmacokinetic mismanagement in polypharmacy patients over 65. The KDIGO 2024 criteria are solid, but the real bottleneck is EHR integration. Most hospitals still use legacy systems that don’t auto-flag drug-drug interactions with renal clearance thresholds.
Also, PPI-induced AIN? Classic. It’s a T-cell mediated hypersensitivity. You’ll see lymphocytic infiltration on biopsy. Steroids work because they suppress CD4+ activation. But most docs just say 'stop the drug' and call it a day. No follow-up Cr checks. That’s lazy.
And Dosis Health? Finally. It uses a Bayesian network trained on 12M EHR records. It’s not magic - it’s data. If you’re not using it, you’re practicing 1990s medicine.
Also, acetaminophen isn’t always safe either - hepatotoxicity risk in cirrhotics. Context matters. Don’t just swap one pill for another. Assess renal AND hepatic function. That’s what I do. #MedEd
Delaine Kiara
Okay so I just read this whole thing and I’m crying. Not because I’m sad - because I’m furious. My aunt died from this. She was on 11 meds. Her doctor didn’t even know she was taking turmeric capsules. She had a CT scan, got contrast, kept taking her NSAID, and then… poof. No warning. No second chance.
And now? They’re giving us AI to fix it? Like we didn’t have enough tech already? Why didn’t anyone tell us this before? Why is this not on the back of every OTC bottle? Why is this not taught in high school health class?
I’m starting a petition. #StopTheSilentKiller #MyAuntWasNotATestSubject #IWantMyMedicationListToNotBeAScavengerHunt
Also, I’m throwing out my Advil. And my mom’s. And my neighbor’s. I’m not stopping until every pharmacy in America has a giant neon sign that says: 'IF YOU’RE OVER 60 OR HAVE KIDNEY ISSUES - DON’T TAKE THIS.'
Also, I’m going to cry again. This is too much.
Also, who’s with me? I need a support group. Like, right now. I can’t do this alone.