Proton Pump Inhibitors and Antifungals: How They Interfere With Absorption

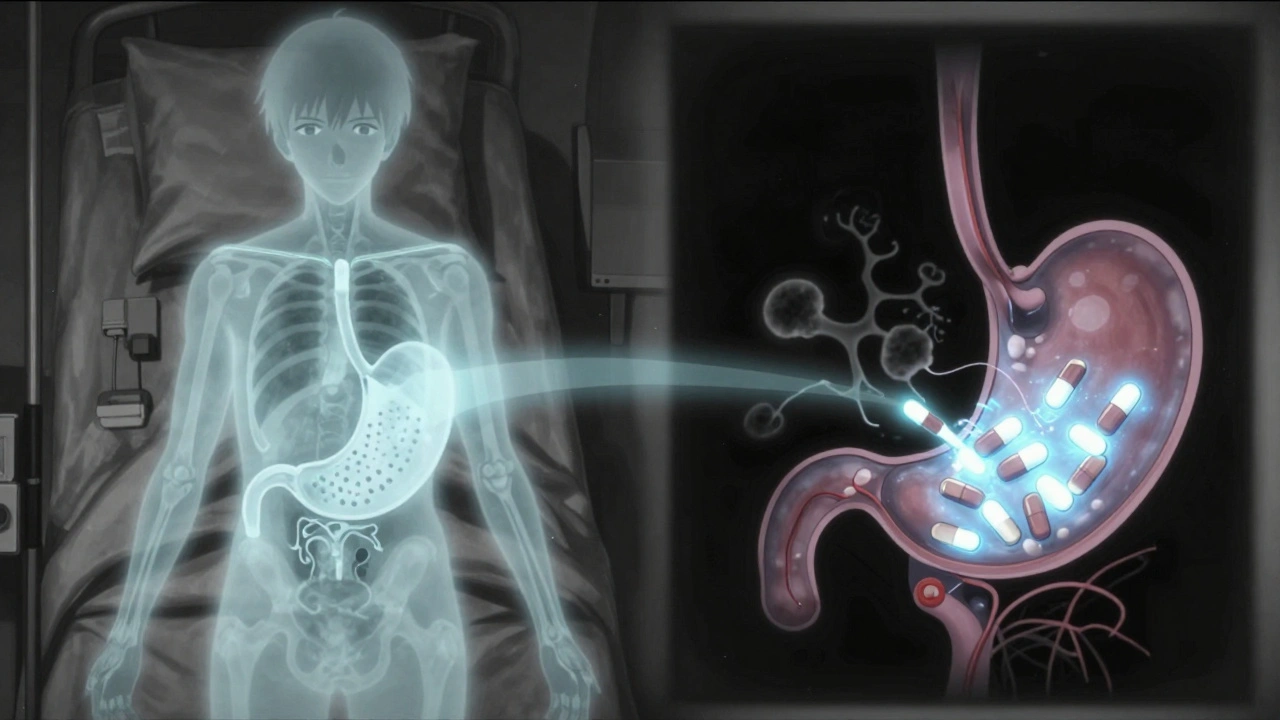
When you take a proton pump inhibitor (PPI) like omeprazole for heartburn and an antifungal like itraconazole for a stubborn fungal infection at the same time, something unexpected can happen: the antifungal stops working as well as it should. This isn’t just a theoretical concern-it’s a real, documented problem that affects thousands of patients every year. The issue isn’t that the drugs clash in your bloodstream. It’s that the PPI changes the environment in your stomach, and that change blocks the antifungal from being absorbed properly.
Why Your Stomach Acid Matters for Antifungals
Most people think of stomach acid as just a nuisance that causes heartburn. But for certain antifungal drugs, it’s essential. Drugs like itraconazole and posaconazole are weak bases. That means they need a low pH-around 3 or lower-to dissolve properly in your stomach before they can be absorbed into your blood. PPIs shut down the acid-producing pumps in your stomach lining. Instead of a pH of 1-2, your stomach might sit at 4-6. That small change makes a huge difference.At higher pH levels, itraconazole doesn’t dissolve. It just sits there, unchanged, and passes through your system without being absorbed. Studies show that when you take itraconazole capsules with a PPI, your blood levels of the drug drop by 50% to 60%. That’s not a minor reduction. It’s enough to turn a treatment that should work into one that fails.
Not All Antifungals Are Affected the Same Way
This isn’t a universal problem. Some antifungals don’t care about stomach pH at all. Fluconazole, for example, dissolves easily in water and gets absorbed no matter how acidic your stomach is. That’s why fluconazole is often the go-to choice when someone needs an antifungal and is already on a PPI.But others are sensitive:
- Itraconazole capsules: 50-60% drop in blood levels with PPIs.
- Itraconazole solution: Only 10-15% drop-much safer to use with PPIs.
- Voriconazole: About 22-35% reduction in absorption.
- Posaconazole delayed-release tablets: 40% drop with PPIs.
- Posaconazole oral suspension: Only 15% drop-better than the tablet form.
Even the formulation matters. The liquid form of itraconazole has the drug already dissolved, so it doesn’t need stomach acid to break it down. That’s why hospitals often switch patients from capsules to the solution if they’re on long-term PPI therapy.
PPIs Are Worse Than Other Acid Reducers
Not all drugs that reduce stomach acid are equal. H2 blockers like famotidine (Pepcid) or ranitidine only lower acid for 4 to 10 hours. PPIs like omeprazole or pantoprazole suppress acid for 12 to 24 hours. That means PPIs create a longer, deeper change in your stomach environment.One study found that omeprazole reduced itraconazole absorption by 57%, while famotidine cut it by only 41%. That’s a big difference. Antacids? They work fast but only last a few hours. If you take them two hours before or after your antifungal, the impact is minimal.
So if you’re stuck on a PPI and need an antifungal, switching to an H2 blocker might be a practical fix-especially if you’re on itraconazole capsules. But you still need to time it right. Take the antifungal at least 10 hours after the H2 blocker to avoid interference.

What Happens When the Antifungal Doesn’t Work
When antifungal levels drop too low, the infection doesn’t get treated. That’s not just frustrating-it’s dangerous. In patients with invasive aspergillosis or coccidioidomycosis, subtherapeutic levels can lead to treatment failure, hospital readmissions, or even death.The European Committee on Antimicrobial Susceptibility Testing (EUCAST) warns that low drug levels can actually make fungi resistant. If the drug is present but too weak to kill the fungus, it gives the fungus time to adapt. What was once a treatable infection becomes harder to manage.
Real-world data confirms this. A 2022 survey of over 1,200 hospital pharmacists found that 68% saw at least one case per month where a patient’s antifungal failed because of a PPI interaction. One pharmacist in Massachusetts General Hospital reported a patient with chronic pulmonary aspergillosis whose itraconazole levels jumped from 0.3 mcg/mL to 1.7 mcg/mL after switching from omeprazole to famotidine. That’s a fivefold increase-enough to turn a failing treatment into a successful one.
What Can You Do? Practical Solutions
If you’re on a PPI and need an antifungal, here’s what actually works:- Switch to fluconazole. If your infection allows it, this is the easiest fix. No interaction. No timing issues.
- Use itraconazole solution instead of capsules. The solution bypasses the pH problem entirely.
- Switch from PPI to H2 blocker. Use famotidine, and take your antifungal at least 10 hours after the H2 blocker.
- Separate doses by 2 hours. For itraconazole solution, take it at least 2 hours before the PPI. For posaconazole tablets, take them with an acidic drink like cola-this can boost absorption by 35%.
- Check blood levels. For serious infections like invasive aspergillosis, therapeutic drug monitoring is critical. Target levels for itraconazole are 0.5-1.0 mcg/mL. If you’re below that, your treatment isn’t working.
Many hospitals now have pharmacists review all antifungal prescriptions in patients on PPIs. That’s because the interaction is so common and so dangerous. A 2023 study showed that when pharmacists intervened, 82% of patients got their dosing right.
New Developments Are Changing the Game
There’s good news on the horizon. In 2023, the FDA approved a new version of itraconazole called Tolsura. Unlike the old capsules, Tolsura is designed to be absorbed regardless of stomach pH. Studies show it only drops 8% in absorption when taken with a PPI-compared to 50% for the old capsules. That’s a game-changer.Even more surprising? Research published in Frontiers in Pharmacology in 2025 found that low-dose omeprazole and itraconazole, when combined in a lab, actually worked better together against resistant strains of Aspergillus fumigatus. The PPI itself seemed to help the antifungal penetrate fungal cells. That’s led to a new NIH clinical trial (NCT05678901) testing whether combining low-dose omeprazole with low-dose itraconazole could treat drug-resistant fungal infections.
So while we’ve spent decades treating this interaction as a problem, we might soon be using it as a tool.
Why This Matters More Than You Think
Over 150 million PPI prescriptions were filled in the U.S. in 2022. About 68% of those were generic omeprazole. Meanwhile, systemic antifungals are used in 5-7% of hospitalized patients. That means thousands of people are getting these two drugs together-often without anyone realizing the risk.The financial cost is also huge. A 2021 study estimated that unnecessary PPI use with pH-dependent antifungals costs the U.S. healthcare system $287 million a year. That’s from wasted drugs, repeat hospital visits, and longer treatments.
And the problem isn’t going away. PPI use is projected to grow 14% annually in older adults, while fungal infections are becoming more common in immunocompromised patients. We’re not going to stop prescribing PPIs. But we need to be smarter about when and how we use them with antifungals.
Final Takeaway: Don’t Assume It’s Safe
If you’re taking a PPI and your doctor prescribes an antifungal, don’t assume it’s fine. Ask: Which antifungal? What formulation? Do I need to change anything? Many patients never get this conversation. That’s dangerous.Fluconazole? Safe with PPIs. Itraconazole capsules? High risk. Itraconazole solution? Much safer. Tolsura? Best option if available. Posaconazole tablets? Watch out. Posaconazole suspension? Better.
And if you’re on a PPI for a condition like GERD or ulcers, ask your doctor if you still need it. Many people stay on PPIs long after they’re necessary. Stopping it might not just help your antifungal-it might help your whole body.
Can I take omeprazole and itraconazole together?
Taking omeprazole and itraconazole capsules together is not recommended. Omeprazole raises stomach pH, which prevents itraconazole capsules from dissolving and being absorbed. This can reduce blood levels by 50-60%, leading to treatment failure. If you must take both, switch to itraconazole solution and separate doses by at least 2 hours. Alternatively, switch from omeprazole to famotidine and take itraconazole 10 hours after the H2 blocker.
Does fluconazole interact with PPIs?
No, fluconazole does not interact with proton pump inhibitors. It is highly water-soluble and absorbs well regardless of stomach pH. This makes it the preferred antifungal for patients on long-term PPI therapy who need systemic treatment for fungal infections.
What’s the best antifungal to use with a PPI?
Fluconazole is the safest choice. If you need an azole and fluconazole isn’t appropriate, use itraconazole solution instead of capsules. Posaconazole suspension is better than the delayed-release tablet. Tolsura, the newer itraconazole formulation, is designed to work even with PPIs and reduces absorption loss to just 8%.
Can I take antacids with antifungals?
Yes, but timing matters. Antacids cause a short spike in stomach pH that lasts only a few hours. If you take your antifungal at least 2 hours before or after the antacid, absorption won’t be significantly affected. This is much safer than using a PPI, which suppresses acid for a full day.
Should I stop my PPI if I need an antifungal?
It depends. If you’re on a PPI for a high-risk reason-like recent GI bleeding or severe ulcers-stopping it could be dangerous. In those cases, switch to fluconazole or itraconazole solution instead. If your PPI was prescribed for mild heartburn and you’ve been on it for years, talk to your doctor about whether you still need it. Many people take PPIs longer than necessary.
Are there new antifungals that don’t interact with PPIs?
Yes. Tolsura, a newer formulation of itraconazole approved in 2023, is designed to be absorbed regardless of stomach pH. It reduces absorption loss with PPIs to just 8%, compared to 50% for older capsules. This makes it a much safer option for patients who must stay on acid-reducing medications.
What to Do Next
If you’re currently taking both a PPI and an antifungal:- Check which antifungal you’re on-capsules or solution?
- Look up whether your specific antifungal is pH-dependent.
- Ask your pharmacist or doctor if your dose needs adjustment.
- Don’t stop either drug without talking to your provider.
- If you’re on itraconazole capsules and a PPI, ask about switching to Tolsura or the solution.
This interaction is preventable. But only if you know it’s happening. Don’t let a simple stomach acid issue become a treatment failure.




Jordan Wall
OMG this is *such* a critical point-I’ve been seeing this in my clinical rotations and it’s wild how many docs just prescribe PPIs like water 😅. Itraconazole capsules + omeprazole? That’s not just suboptimal-it’s *pharmacologically negligent*. The fact that 50-60% absorption drop is *common* and yet still overlooked? We’re basically giving patients placebo antifungals. And don’t even get me started on posaconazole tablets… 🤦♂️
Also, Tolsura? Game. Changer. Why isn’t this the default yet? Pharma needs to stop making us jump through hoops. Also-cola with posaconazole? Genius. I’m telling my preceptor tomorrow. #PharmDlife
Gareth Storer
So let me get this straight-stomach acid is suddenly a *drug delivery system*? Next you’ll tell me my tears are just saline IVs. 🤨
Meanwhile, my grandma’s on omeprazole for ‘indigestion’ she’s had since 1998 and just got prescribed itraconazole for ‘athlete’s foot that went to war.’ She’s gonna die of fungus. Or boredom. Same thing.
Pavan Kankala
This is all corporate BS. PPIs are just a tool to make you dependent so Big Pharma can sell you more drugs. They don’t care if your antifungal fails-they care if your *bill* goes up. Fluconazole? Too cheap. Tolsura? Too new. They want you stuck on omeprazole forever. Why? Because they own the patents. And the FDA? Paid off. I’ve seen it. They suppress data on drug interactions all the time. This isn’t science-it’s capitalism with a stethoscope.
Also, why are we even using antifungals at all? Fungi are just nature’s way of cleaning up our toxic lifestyles. Let the fungus win. Maybe then we’ll stop eating processed garbage and taking 12 pills a day.
Martyn Stuart
Thank you for this incredibly clear, well-structured, and clinically vital post. I’m a hospital pharmacist, and I’ve had to intervene in at least three cases this month alone because of this exact interaction. The 68% statistic? I believe it. One patient had a recurrent invasive aspergillosis because their PPI was never flagged. They were on itraconazole capsules. We switched them to the solution-and their levels normalized within 72 hours. It’s *that* simple. And yet, so many prescribers still don’t know.
For anyone reading this: if you’re on a PPI and prescribed an azole antifungal, ask for the formulation. Ask if fluconazole is an option. Ask if Tolsura is available. Don’t assume. Don’t wait. And if you’re the prescriber-check your interactions before you hit ‘send.’ It’s not just a recommendation-it’s a standard of care.
Also: H2 blockers aren’t perfect, but famotidine 20mg, taken 10 hours before itraconazole? Viable. Antacids? Fine if timed right. But PPIs? They’re the silent killers here.
Jessica Baydowicz
Okay I just read this and I’m like… WHY ISN’T THIS ON EVERY MED SCHOOL SYLLABUS?! 😱
I have a cousin who was on omeprazole for years and then got fungal pneumonia-and the antifungal didn’t work for months. They thought it was ‘resistant’ but it was just the PPI! They finally switched to fluconazole and boom-she’s back to hiking and baking sourdough. This is life-changing info. Please, please, please share this with your doctor. Or your aunt. Or your yoga instructor. Everyone needs to know this!! 💪✨
Shofner Lehto
Let’s not romanticize fluconazole as the universal solution. It’s not always appropriate-especially in invasive mold infections. I’ve seen patients with aspergillosis who had to be switched to voriconazole, and even then, the PPI interaction was a nightmare. The key isn’t just substitution-it’s awareness. Every time you prescribe an antifungal, ask: Is this pH-dependent? What’s the formulation? What’s the patient’s acid status? That’s the new triage.
And yes-Tolsura is a breakthrough. But access? Cost? Insurance? It’s still a luxury in many places. We need formulary changes, not just academic awareness.
Also, the NIH trial on low-dose omeprazole + itraconazole? Fascinating. Maybe we’ve been treating this as a problem when it’s actually a pathway. Science is weird like that.
Karl Barrett
This is the kind of post that reminds me why I love pharmacology. It’s not just about molecules-it’s about the invisible environments inside us. The stomach isn’t just a bag of acid; it’s a chemical reactor. And we’ve been treating it like a dumb switch: on/off. But pH is a gradient. And gradients matter.
The fact that a 2-unit pH shift can tank drug absorption by half… that’s elegance. And tragedy. We’re not just giving pills-we’re altering the terrain of the body. And we rarely check if the terrain still supports the medicine.
I wonder if this applies to other weak base drugs. Antibiotics? Antivirals? Maybe we’re underdosing a whole class of meds because we assume stomach acid is ‘just’ for digestion. It’s not. It’s a gatekeeper. And we’re letting it be turned off by accident.
And that NIH trial? If low-dose PPI helps antifungals penetrate biofilms? That’s not a side effect. That’s a new mechanism. Maybe we’re not just fixing interactions-we’re discovering synergies.
George Graham
I just want to say thank you for writing this. I’ve been on PPIs for 12 years for GERD, and last year I got a fungal sinus infection. My ENT prescribed itraconazole capsules. I took them for three weeks. Nothing happened. I thought I was just ‘bad at healing.’ Turns out, my stomach was too calm for the drug to work. My pharmacist flagged it when I filled the refill. We switched to fluconazole. Two weeks later, the fungus was gone.
I didn’t know any of this. No one told me. I just took the pills. And I’m not dumb-I’m a teacher. If this happened to me, imagine how many others are suffering silently.
Please, if you’re reading this and you’re on a PPI-ask your doctor if your meds are talking to each other. It’s not paranoia. It’s responsibility. And it might save your life.
John Filby
Wait so… cola helps posaconazole? 😳 I’m going to start drinking Coke with my antifungals now. That’s either genius or a terrible idea. Either way, I’m telling my mom. She’s on omeprazole and just got antifungals for her toenails. She thinks it’s ‘just fungus’-but now she’s got a whole new reason to hate soda. 😆
Also Tolsura? Sounds like a superhero drug. I’m rooting for it. Maybe next they’ll make a version that also fixes your Wi-Fi.
Elizabeth Crutchfield
oh my god i just realized i’ve been taking my itraconazole with my morning coffee and omeprazole… for months… 😬 i thought the coffee was helping? guess i was just making it worse. gonna call my dr tomorrow. thanks for the wake-up call!!