Sirolimus and Wound Healing: When to Start After Surgery

Sirolimus Wound Healing Risk Calculator
Sirolimus Wound Healing Risk Assessment
This tool helps determine the optimal time to start sirolimus after surgery based on your specific health factors. The recommendation is based on current medical guidelines for wound healing and transplant recovery.
Results
Recommended Start Time
Sirolimus is a powerful immunosuppressant used to prevent organ rejection after transplants-especially kidney transplants. But if you’re planning surgery or just had one, this drug can mess with your healing. It’s not that sirolimus is dangerous; it’s that it slows down the body’s natural repair process. And that matters. A lot.
How Sirolimus Actually Stops Wounds from Healing
Sirolimus works by blocking a protein called mTOR. That’s great for stopping immune cells from attacking a new kidney. But mTOR isn’t just involved in immunity-it’s also critical for wound healing. When you cut your skin, your body sends out signals to rebuild tissue. Fibroblasts move in to make collagen. Blood vessels grow to bring oxygen and nutrients. Immune cells clean up debris. Sirolimus shuts down all of that.
Studies in rats show that when given sirolimus at typical human doses (2.0 to 5.0 mg/kg/day), wound strength drops by up to 40%. Collagen, the main structural protein in scars, gets cut in half. Blood vessel growth (angiogenesis) slows because sirolimus crushes VEGF-the molecule that tells blood vessels where to grow. Without enough VEGF, your wound doesn’t get the fuel it needs. And it’s not just skin. The same thing happens in abdominal incisions, chest wounds, and even surgical sites in the mouth.
What’s worse? Sirolimus doesn’t just stay in your blood. It concentrates in wound fluid-sometimes two to five times higher than in your bloodstream. That means your surgical cut is basically swimming in the drug.
The Real Risk: Infections and Open Wounds
When healing slows, infections creep in. A 2008 Mayo Clinic study looked at 26 transplant patients on sirolimus who had skin surgeries. Nearly 1 in 5 developed infections. That’s more than three times the rate in patients not on sirolimus. Wound dehiscence-where the cut reopens-happened in 7.7% of those on sirolimus. Zero in the control group. The numbers weren’t statistically significant because the group was small, but the pattern was clear.
And it’s not just infections. Lymphocele-a buildup of lymph fluid near the transplant site-is more common with sirolimus. It can cause pain, swelling, and even compress the new organ. One study found that up to 15% of patients on sirolimus developed lymphoceles after kidney transplant, compared to 3% on other drugs.
But here’s the twist: not everyone has problems. Some patients heal just fine. Why? Because risk isn’t the same for everyone.
Who’s Most at Risk?
Sirolimus doesn’t hit everyone the same way. Your body’s condition before surgery matters more than the drug itself.
- Obesity: A BMI over 30 doubles your risk of wound complications. Fat tissue has poor blood flow and is harder to close surgically. Add sirolimus, and healing becomes a battle you’re already losing.
- Diabetes: High blood sugar gums up collagen formation and weakens immune defenses. Combine that with sirolimus, and your wound turns into a slow leak.
- Smoking: Nicotine narrows blood vessels. Carbon monoxide steals oxygen from tissue. Smokers need to quit at least four weeks before surgery-not just for sirolimus, but for any healing.
- Malnutrition: Protein is the building block of skin and muscle. If your albumin level is low, your body can’t repair itself, no matter how good the drug is.
- Age: Older patients heal slower naturally. Sirolimus doesn’t make them worse-it just makes the gap wider.
Some of these you can fix. Others you can’t. But knowing which ones you have lets your doctor adjust the plan.
When Should You Start Sirolimus After Surgery?
For years, the rule was simple: don’t start sirolimus until two weeks after surgery. Many hospitals still follow that. But that’s changing.
Early studies from 2007 and 2009 showed clear harm. But newer data-like the 2022 Wiley review-says those fears might be outdated. The key isn’t timing alone. It’s how you time it.
Here’s what top transplant centers are doing now:
- High-risk patients (diabetic, obese, smoker, poor nutrition): Delay sirolimus until day 14-21. Wait until the wound is visibly closed, no drainage, no redness.
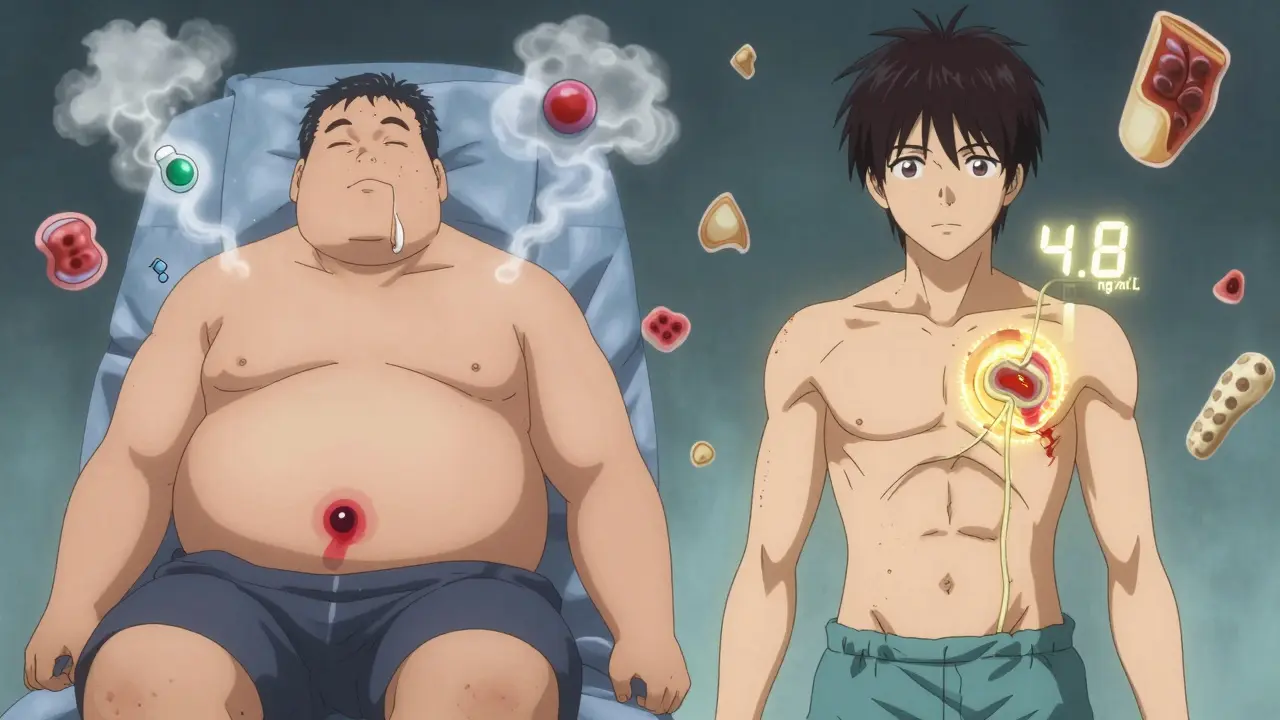
- Low-risk patients (young, healthy, non-smoker, normal BMI): Start as early as day 7. Studies show no increase in complications if the wound is stable and trough levels are kept below 6 ng/mL.
- Monitoring matters: Check sirolimus blood levels weekly in the first month. Keep them between 4-6 ng/mL. Higher than that? Healing slows. Lower than that? Risk of rejection goes up.
One study found that patients who started sirolimus on day 7 with levels under 5 ng/mL had the same infection rate as those who started on day 14. The difference? Careful monitoring.
What About Other Immunosuppressants?
Sirolimus isn’t the only drug that slows healing. Steroids, mycophenolate, and antithymocyte globulin (ATG) do too. But here’s the trick: they don’t all do it the same way.
Steroids reduce inflammation, which sounds good-but they also block collagen production. Mycophenolate stops immune cells from multiplying, which can delay tissue repair. ATG wipes out immune cells entirely, leaving you vulnerable.
That’s why many centers now use combination therapy. Start with steroids and mycophenolate right after surgery. Wait until day 7-10. Then add sirolimus at a low dose. This way, you’re not hitting healing with all the brakes at once.
Some centers even use sirolimus as a replacement for calcineurin inhibitors (like tacrolimus) after healing is complete. Why? Because calcineurin inhibitors damage kidneys over time. Sirolimus doesn’t. So once the wound is sealed, switching to sirolimus can protect your new organ for life.

What’s the Bottom Line?
Sirolimus can hurt wound healing-but it doesn’t have to. The old idea that you must wait two weeks is fading. The new rule? Match the timing to the patient.
If you’re young, healthy, and your wound looks good by day 7, starting sirolimus is safe. If you’re overweight, diabetic, or still smoking? Wait. Optimize your health first. Quit smoking. Control your sugar. Eat protein. Get your albumin up.
And don’t forget: your surgeon and transplant team need to talk. The surgeon cares about the cut. The transplant doctor cares about rejection. Both need to agree on when to start sirolimus. No one should make that call alone.
Sirolimus is a tool. Not a threat. Used right, it protects your new kidney for decades. Used wrong, it turns a simple surgery into a long recovery. The difference isn’t the drug. It’s the plan.
What You Can Do Right Now
If you’re on sirolimus and scheduled for surgery:
- Ask for a pre-op nutrition check-albumin, protein intake, vitamin levels.
- Get your blood sugar under control if you’re diabetic.
- Quit smoking. No exceptions. Four weeks minimum.
- Ask your doctor: "What’s my wound healing risk score?" Some centers use simple checklists.
- Request sirolimus level monitoring after surgery. Don’t assume it’s fine.
If you’ve already had surgery and were started on sirolimus too soon:
- Watch for redness, swelling, pus, or the wound reopening.
- Call your doctor immediately if the wound isn’t getting smaller by day 5.
- Don’t panic. Many complications are fixable if caught early.
Can sirolimus cause my surgical wound to open up?
Yes, it can. Sirolimus reduces collagen production and blood vessel growth, which weakens the wound’s strength. Studies show wound dehiscence rates of up to 7.7% in transplant patients on sirolimus, especially if started too early or in high-risk patients like those with obesity or diabetes.
How long should I wait after surgery before starting sirolimus?
For low-risk patients (normal weight, no diabetes, non-smoker), sirolimus can often start at day 7-10 if the wound is closed and healing well. For high-risk patients, wait until day 14-21. Always confirm wound stability with your surgeon before starting.
Is sirolimus safe after skin surgery?
Yes, if managed properly. A 2008 Mayo Clinic study found no statistically significant increase in complications after dermatologic surgery when sirolimus was used with careful timing and monitoring. Smaller, superficial wounds heal better than deep abdominal incisions, so risk varies by procedure type.
Can I take sirolimus if I’m diabetic?
It’s possible, but risky. Diabetes already slows healing. Adding sirolimus increases the chance of infection and wound breakdown. If you’re diabetic, your doctor should delay sirolimus until at least day 14, ensure your blood sugar is tightly controlled, and monitor your wound closely. Optimizing your glucose levels before surgery is critical.
Do I need to stop sirolimus before surgery?
No. Stopping sirolimus increases the risk of organ rejection. Instead, delay restarting it after surgery based on your healing progress and risk factors. Never stop it without consulting your transplant team.
Are there alternatives to sirolimus that don’t affect healing?
Calcineurin inhibitors like tacrolimus and cyclosporine are common alternatives, but they carry long-term kidney toxicity. Mycophenolate and steroids also slow healing, just differently. The choice depends on your overall health, cancer risk, and kidney function. Sirolimus is often preferred for patients with high cancer risk because it reduces skin cancer rates by up to 50% in transplant recipients.



Susie Deer
Sirolimus is just another big pharma scam to keep people dependent. Stop the drug and let your body heal naturally. No need for all this overcomplicated science.
TooAfraid ToSay
You think this is bad? Wait till you hear about the government using sirolimus to slow down veterans' healing so they stay on disability. The truth is buried under 10 layers of medical jargon.
Dylan Livingston
Oh sweet mercy, another armchair immunologist with a 2008 Mayo Clinic citation like it's the Dead Sea Scrolls. Let me guess-you also think vitamin C cures cancer and that collagen supplements are the new holy water. The real tragedy isn't sirolimus-it's the cult of oversimplified medical advice that turns patients into passive consumers of fear.
Andrew Freeman
bro just wait 14 days and dont stress about it. i had a cousin get a kidney and they started sirolimus on day 7 and he was fine. maybe its not that big a deal
says haze
The real issue here isn't mTOR inhibition-it's the epistemological collapse of modern medicine. We've replaced clinical wisdom with algorithmic decision trees based on BMI and albumin levels like patients are data points in a spreadsheet. The surgeon and transplant doctor must 'talk'? What a quaint notion. In 2024, they're probably texting in a Slack channel while the patient bleeds out in silence.
Alvin Bregman
i read this whole thing and honestly i think the key is just listening to your body. if the wound looks good and you feel okay, maybe its fine to start sooner. everyone's different. dont let anyone tell you there's one right way
Sarah -Jane Vincent
They're lying. Sirolimus doesn't slow healing. It's designed to make you dependent. The FDA and Big Pharma know if you heal too fast, you stop taking their drugs. That's why they push the 'wait 14 days' myth. Look at the patent filings-there's a hidden clause about 'delayed tissue regeneration protocols'. They're monetizing your pain.
Jason Yan
I've seen this play out with my own dad-he's a transplant recipient, diabetic, former smoker, and honestly? He waited 21 days. Started sirolimus at 4.5 ng/mL. Wound closed clean as a whistle. What this post nails is that it's not about the drug. It's about the person. You can't treat a human like a lab rat with one-size-fits-all rules. Take the time. Fix what you can. Eat protein. Sleep. Breathe. Healing isn't a checkbox-it's a relationship with your own body.
shiv singh
Why are we even talking about this? In my country, we don't wait. We start the drug on day 1. If the wound opens, then the body was weak anyway. Sirolimus is not the problem. Weak people are the problem. Stop blaming the medicine and fix yourself.
Sarah Triphahn
Let me be the one to say it: if you're obese and diabetic and still smoking, you shouldn't even be getting a transplant. This isn't about sirolimus. This is about people who refuse to change their lives expecting medicine to fix everything. You want to heal? Stop eating sugar. Stop smoking. Stop pretending you're too busy to care. The drug isn't the villain. Your choices are.
Vicky Zhang
I just want to say to anyone reading this: you are not broken. You are not a risk factor. You are not a statistic. If you're scared, that's okay. If you're confused, that's okay too. Your body is trying so hard to heal. And your medical team? They're trying too. Just ask questions. Say no if you're not ready. Eat that protein shake. Walk around the block. Breathe. You've got this. I believe in you.