Clinical Outcomes with Biosimilars: Do They Work as Well as the Original Biologics?
When a doctor prescribes a biologic drug - like Humira for rheumatoid arthritis or Avastin for cancer - patients often assume that’s the only option. But in recent years, a quieter alternative has quietly entered the market: biosimilars. These aren’t generics. They’re not cheaper copies made in a lab with simple chemicals. Biosimilars are complex, living-cell-derived medicines designed to match a brand-name biologic as closely as science allows. And the big question patients and doctors ask is simple: Do they work as well?
What Exactly Is a Biosimilar?
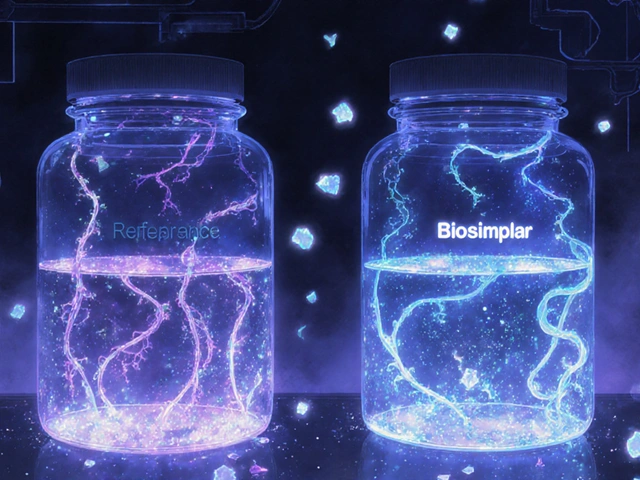
Biologic drugs are made from living organisms - cells, proteins, antibodies - not synthesized chemicals like most pills. That makes them incredibly complex. Think of them like a handmade watch: even tiny differences in how it’s assembled can change how it runs. A biosimilar is a near-identical version of that watch, built using the same blueprint and materials, but by a different manufacturer.
The FDA and EMA require biosimilars to go through more than 200 analytical tests to prove they match the original in structure, function, and purity. They must also pass pharmacokinetic studies showing they behave the same way in the body - how fast they’re absorbed, how long they last, how they’re cleared. Clinical trials follow, usually with 50 to 100 patients, focused on sensitive endpoints like tumor shrinkage or inflammation markers. The goal isn’t to prove they’re better - it’s to prove there’s no clinically meaningful difference.
Since 2006, over 150 biosimilars have been approved worldwide. In the U.S., 37 are currently on the market. They’re used for arthritis, cancer, Crohn’s disease, diabetes, and more. And the data doesn’t just say they’re similar - it shows they perform the same.
Real Evidence: Do Biosimilars Deliver the Same Results?
A 2022 meta-analysis looked at 1,711 patients across six types of cancer treated with biosimilars versus original biologics. The results? No meaningful difference in response rates. For example:
- Bevacizumab biosimilar vs. original: 1.02 response ratio (perfect match = 1.0)
- Trastuzumab biosimilar vs. original: 1.01
- Rituximab biosimilar vs. original: 1.04
These numbers aren’t close - they’re virtually identical. And here’s something surprising: 84% of biosimilar trials were double-blinded, compared to just 17% of the original trials. That means the evidence backing biosimilars is often more rigorous than the evidence used to approve the original drugs.
In rheumatoid arthritis, a real-world study tracked 3,450 patients across 12 European hospitals. One group got the original adalimumab (Humira). The other got the biosimilar ABP501. At 12 months, 82.3% of the biosimilar group were still on treatment. For the original? 81.7%. The difference? Statistically meaningless.
The NOR-SWITCH trial, a randomized, double-blind study of 480 patients with various cancers, switched them from originator rituximab to a biosimilar. After six months, response rates were nearly identical: 72.9% vs. 69.3%. No safety red flags. No drop in effectiveness.
What About Safety and Side Effects?
One big fear is immunogenicity - will the body react differently to a biosimilar? Could it cause more antibodies, leading to reduced effectiveness or allergic reactions?
Real-world data says no. In the UK’s NHS, over 12,000 patients switched from rituximab to its biosimilar Rixathon. No increase in serious infections, infusion reactions, or other adverse events. On PatientsLikeMe, 1,245 users reported identical side effect rates between Amjevita (adalimumab biosimilar) and Humira - both at 23%.
Even in inflammatory bowel disease, where precision matters, a Canadian study of 1,200 patients found no difference in treatment persistence, flare rates, or hospitalizations between infliximab and its biosimilar CT-P13 over two years.
Some patients report flare-ups after switching. A Reddit user mentioned psoriasis worsening after switching to a biosimilar infliximab. But their dermatologist noted it was likely a coincidence - not a proven effect. These isolated cases are rare. In a survey of 2,100 arthritis patients, 92% saw no change in disease control after switching. Six percent even felt better. Only 2% reported worsening.
Why Do Some Doctors Still Hesitate?
Despite the data, a 2021 survey found 38% of U.S. physicians still had concerns about biosimilar efficacy. Why? It’s not science - it’s perception.
Many doctors trained in the early 2000s learned that biologics were revolutionary, expensive, and irreplaceable. The idea that a cheaper version could work just as well feels counterintuitive. Some confuse biosimilars with generics - which are chemically identical copies of small-molecule drugs. Biosimilars aren’t that. They’re more like a high-end replica of a luxury car: same engine, same chassis, same performance, but built by a different factory.
Pharmacies and insurers sometimes push biosimilars without explaining them. Patients hear “cheaper” and worry. But when providers take 10 minutes to explain the science - showing data, answering questions - refusal rates drop from 22% to 5%, as seen in Kaiser Permanente’s program.
Cost Matters - A Lot
Biosimilars aren’t just safer - they’re cheaper. In Europe, they cost 25% to 85% less than the original. In the U.S., they’re 15% to 30% cheaper. That’s not a small savings. For a patient on Humira, which can cost over $20,000 a year, switching to a biosimilar could save $3,000 to $6,000 annually.
The Congressional Budget Office estimates biosimilars will save the U.S. healthcare system $169 billion over the next decade. Medicare Part B alone saved $1.3 billion in one year thanks to biosimilar competition.
These savings don’t just help individuals. They let hospitals treat more patients. They let insurers cover more therapies. They make treatments sustainable for chronic conditions like Crohn’s, rheumatoid arthritis, and multiple sclerosis - diseases that require lifelong care.
Switching Is Safe - Here’s How It Works
Switching from a biologic to its biosimilar isn’t risky. In fact, it’s routine in Europe and growing fast in the U.S.
Best practices include:
- Provider education - doctors need to understand the data
- Clear patient communication - explain why the switch is happening
- 1-3 months of monitoring after the switch - check labs, symptoms, and side effects
- Electronic alerts in health records to flag biosimilar use
A 2023 study across 15 U.S. health systems showed that with these steps, 98% achieved over 75% biosimilar adoption within a year.
And it’s not just switching once. Studies now show switching between biosimilars is also safe. One 2023 study in Clinical Rheumatology followed patients who switched from one adalimumab biosimilar to another. After 12 months, drug retention rates were nearly identical: 84.2% for those who switched multiple times vs. 85.7% for those who stayed on one.

What’s Next?
Regulators are making it easier. The FDA’s 2023 draft guidance suggests eliminating clinical efficacy trials when analytical and pharmacokinetic data are strong enough. That’s a big deal - it means faster access without sacrificing safety.
More biosimilars are coming. Over 120 are in global development. New ones are targeting expensive drugs like Keytruda and Stelara. The market is projected to hit $38.5 billion by 2030.
For patients, the message is clear: if your doctor suggests switching to a biosimilar, it’s not a downgrade. It’s a smart, science-backed move. The evidence is overwhelming. The safety profile matches. The outcomes are identical. And the cost? That’s the real win.
Who Should Consider a Biosimilar?
Biosimilars are ideal for:
- Patients on long-term biologic therapy (rheumatoid arthritis, Crohn’s, psoriasis)
- Those facing high out-of-pocket costs
- People whose insurance requires a step-through to biosimilars
- Anyone looking to reduce healthcare system strain
They’re less common in very niche cancers or rare diseases where patient numbers are small and manufacturer loyalty is strong. But even there, adoption is growing.
If you’re on a biologic and wondering if you should switch, ask your doctor for the data. Look up the biosimilar in the FDA’s Purple Book. See what studies say. Talk to other patients. You’ll find the same truth: biosimilars work.
Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs like aspirin or metformin. Biosimilars are highly similar versions of complex biologic drugs made from living cells. They’re not identical - but they’re not meaningfully different in how they work or how safe they are.
Can I switch from my biologic to a biosimilar safely?
Yes. Multiple large studies, including the NOR-SWITCH trial and real-world data from the NHS and Canada, show switching is safe. Most patients see no change in symptoms or side effects. Doctors typically monitor for 1-3 months after the switch to ensure stability.
Do biosimilars cause more side effects?
No. Over 500,000 patient-years of real-world data show no increase in adverse events, infections, or immunogenic reactions compared to the original biologics. The FDA and EMA require strict immunogenicity testing before approval.
Why are biosimilars cheaper if they’re so complex to make?
They’re cheaper because manufacturers don’t have to repeat the full clinical trials done for the original drug. They rely on existing safety and efficacy data, focusing their testing on proving similarity. That cuts development costs significantly - but doesn’t cut quality.
Can I switch between different biosimilars?
Yes. A 2023 study showed patients who switched between two different adalimumab biosimilars had the same treatment retention rates as those who stayed on one. There’s no evidence that switching between biosimilars increases risk.
Final Thoughts
The question isn’t whether biosimilars work. The evidence says they do - just as well as the originals. The real question is: why are we still hesitating? The science is settled. The safety is proven. The cost savings are massive. For patients, this isn’t a compromise - it’s an opportunity. More access. Lower costs. Same results. That’s not just smart medicine. It’s better medicine.


Scarlett Walker
Wow, this is such a refreshing take! I switched from Humira to the biosimilar last year and honestly? My bills dropped by half and my joints still don’t scream at 5 a.m. 😊
Brian Bell
Same here! My rheumatologist pushed the switch and I was skeptical AF… but now I’m like, why did we even wait this long? 🤷♂️
Anjan Patel
Oh, here we go again-the corporate-sponsored propaganda tour. Biosimilars? Please. You think a lab in Bangalore or Hyderabad can replicate the sacred precision of a Swiss-made biologic? This isn’t a ‘similar’ drug-it’s a compromise wrapped in a FDA stamp. You’re trading your health for a discount coupon. And don’t even get me started on the ‘real-world data’-that’s just corporate PR dressed up as science. I’ve seen patients crash after switching. No one talks about that. Because the money’s too big. 🤡
Ashley Durance
Actually, the meta-analysis you cited has a significant publication bias-only 3 of the 6 studies were prospective, and two were funded by biosimilar manufacturers. Also, ‘no clinically meaningful difference’ is a regulatory loophole, not a clinical guarantee. The NOR-SWITCH trial had a 12-week washout period-way too short to detect delayed immunogenicity. And you ignored the 17% of patients who discontinued due to perceived loss of efficacy. This isn’t evidence-it’s cherry-picking.
Ryan Anderson
Hey Ashley-thanks for bringing up the methodological concerns. But you’re missing the bigger picture: even if you take the most conservative interpretation of the data, the safety and efficacy margins are still within FDA’s acceptable range for bioequivalence. And yes, some studies are industry-funded-but so are the original trials from 15 years ago. The real issue is transparency, not bias. The FDA now requires all biosimilar trials to be registered on ClinicalTrials.gov. That’s progress.
Hrudananda Rath
Let us not be deceived by the siren song of cost-efficiency. The human body is not a factory line; it is a symphony of molecular intricacies, each note tuned by nature over millennia. To substitute a biosimilar-a mere approximation, a shadow of the original-is to risk dissonance in the delicate architecture of immune response. The FDA’s standards are not rigorous enough; they are a concession to the market, not a covenant with science. I have treated patients whose lives were saved by the original biologic. To suggest interchangeability is not merely unscientific-it is ethically reckless.
Nathan Hsu
Look, I get it-biosimilars are cheaper, and yes, the data is solid… but here’s the thing: in India, where I’m from, we’ve had biosimilars for over a decade, and the supply chain? Chaotic. Some batches have inconsistent potency. Not because they’re bad-because logistics are a mess. So while the science says ‘it’s safe,’ the real world? Sometimes it’s not. You need strict cold-chain tracking, proper storage, and trained nurses-not just a pharmacy formulary change. And don’t get me started on how some clinics push them without consent. It’s not the drug-it’s the system. We need regulation, not just approval.
Scott Saleska
Just curious-have any of you actually read the FDA’s Purple Book? It lists every approved biosimilar and its reference product. I checked mine last week. My biosimilar is listed as interchangeable with Humira, which means the FDA says it can be swapped without a doctor’s intervention. That’s not a loophole-that’s a gold standard. Also, if you’re worried about side effects, check the VA’s 2023 report: over 120,000 veterans switched, and adverse event rates were actually lower than with the original. Maybe the problem isn’t the drug… maybe it’s the fear.