Colorectal Polyp Types: Understanding Adenomas vs. Serrated Lesions
By age 60, about one in every two adults will have at least one colorectal polyp. Most of these are harmless, but some can turn into cancer if left alone. Not all polyps are the same. Two major types-adenomas and serrated lesions-carry different risks, grow in different ways, and need different handling. Knowing the difference isn’t just medical jargon; it’s what guides your screening, your treatment, and your long-term health.
What Are Adenomas?
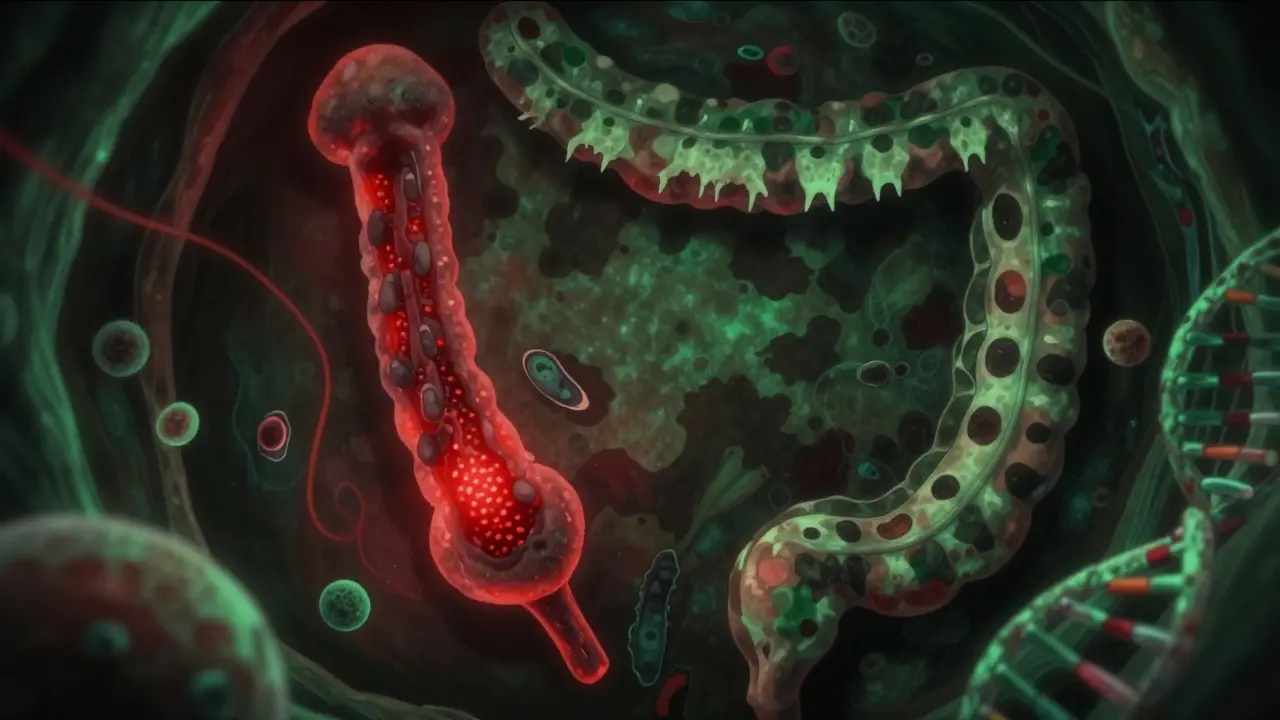
Adenomas are the most common precancerous polyps, making up about 70% of all polyps found during colonoscopies. They start as small bumps on the colon lining and grow slowly over years. Under the microscope, they look like abnormal glandular tissue-think of them as misshapen plumbing pipes inside your colon.
There are three main types of adenomas, based on how they grow:
- Tubular adenomas (70% of adenomas): These are the most common and least risky. They’re usually small, round, and grow like little mushrooms on a stalk. If they’re under half an inch, the chance of cancer is less than 1%.
- Tubulovillous adenomas (15%): These mix tubular and villous features. They’re more likely to grow larger and have a higher chance of containing cancer cells.
- Villous adenomas (15%): These are flat, spread out, and stick tightly to the colon wall. They’re harder to remove completely and carry the highest cancer risk. A villous adenoma over 1 cm has a 10-15% chance of already having cancer in it.
Size matters a lot. A 5 mm adenoma? Very low risk. A 2 cm adenoma with villous features? That’s a red flag. Doctors watch size and shape closely because the bigger and flatter it is, the harder it is to catch-and the more likely it is to hide cancer.
What Are Serrated Lesions?
Serrated lesions are the quiet threat. They don’t look like the classic polyp you imagine. Instead, under the microscope, they have a saw-tooth edge-hence the name “serrated.” These make up 20-30% of colorectal cancers, even though they’re less common than adenomas.
There are three types:
- Hyperplastic polyps: These are usually harmless, especially if they’re small and found in the lower colon. They rarely turn into cancer.
- Sessile serrated adenomas/polyps (SSA/Ps): These are the real concern. They’re flat, often hidden in the right side of the colon (the cecum or ascending colon), and easy to miss during a colonoscopy. They grow slowly but follow a different path to cancer than adenomas. About 13% of SSA/Ps already show signs of high-grade dysplasia or early cancer when removed.
- Traditional serrated adenomas (TSAs): These are rarer but aggressive. They often have villous features and can turn cancerous faster than SSA/Ps.
SSA/Ps are especially tricky because they don’t bulge out like a mushroom. They’re flat, sometimes barely raised, and blend into the colon wall. Standard colonoscopy misses them 2-6% of the time. That’s why newer tools-like high-definition scopes and AI-assisted systems such as GI Genius-are now used in many clinics. These tools boost adenoma detection by up to 18%, and they help catch these sneaky lesions too.
Key Differences Between Adenomas and Serrated Lesions
Here’s how they stack up:
| Feature | Adenomas | Serrated Lesions (SSA/Ps) |
|---|---|---|
| Appearance | Pedunculated (stalked) or sessile, often round | Flat or slightly raised, often invisible without magnification |
| Location | More common in the left colon and rectum | Mostly in the right colon (cecum, ascending) |
| Microscopic pattern | Glandular, tubular or villous | Saw-tooth crypts, inverted growth |
| Cancer pathway | Chromosomal instability (APC gene mutations) | CpG island methylation (BRAF mutations) |
| Miss rate during colonoscopy | 5-10% | Up to 20% due to flat shape and location |
| Cancer risk if >1 cm | 10-15% | 13% (similar to adenomas) |
| Removal success rate | 95-98% (if <2 cm) | 80-85% (due to flat, broad base) |
Even though SSA/Ps are less common, they’re just as dangerous as large adenomas. The big difference? You’re more likely to miss one. And if you do, it can slip under the radar for years.
Why Detection Matters
Most polyps don’t cause symptoms. That’s why screening is everything. By the time someone feels bleeding, changes in bowel habits, or fatigue from anemia, the polyp may already be cancerous.
SSA/Ps are especially silent. They grow slowly, often without bleeding. That’s why they’re called “insidious”-they don’t scream for attention. A 2022 study found that 68% of SSA/Ps are found in the proximal colon, the part of the colon that’s hardest to see during a routine colonoscopy. That’s why doctors now use high-definition scopes, dye spraying, and AI tools to make sure they don’t miss anything.
Even with the best tools, some lesions get missed. That’s why follow-up timing matters. If you have an SSA/P over 1 cm, the American Cancer Society recommends a colonoscopy in 3 years. Some European guidelines say 5 years-but that’s still debated. The bottom line: if you’ve had a serrated polyp, you’re 1.5 to 2.5 times more likely to develop colorectal cancer later. But here’s the good news: if you catch and remove it, your risk drops back to near-normal.
What Happens After Removal?
Getting a polyp removed during a colonoscopy is usually a simple, safe procedure. For most adenomas under 2 cm, success rates are 95-98%. For flat SSA/Ps, especially over 2 cm, it’s harder. Success rates drop to 80-85%. That’s why some patients need a second look or even surgery if the polyp wasn’t fully removed.
After removal, the pathologist checks the tissue. Two things matter most:
- Was it removed completely? If not, you’ll need another procedure.
- Does it show cancer? If it does, you’ll need further tests and possibly surgery.
If the polyp was benign and fully removed, you’ll get a follow-up schedule. For small tubular adenomas, you might wait 5-10 years. For SSA/Ps over 1 cm? Back in 3 years. For multiple or large polyps? Even sooner.

What’s Changing in Screening?
Technology is catching up. In 2022, the FDA approved AI-assisted colonoscopy systems like GI Genius. These tools highlight suspicious areas in real time during the exam. In one trial, they increased adenoma detection by 14-18%. That means more SSA/Ps and early cancers are caught before they spread.
Future screening won’t just be about what a polyp looks like. It’s moving toward molecular testing. Adenomas often have APC gene mutations. SSA/Ps have BRAF mutations and high levels of DNA methylation. Soon, doctors may test polyps right after removal to see how likely they are to turn cancerous. That could mean personalized follow-up schedules-some people might wait 5 years, others might need one in 18 months.
The goal? Cut down on the 6.5 million surveillance colonoscopies done each year in the U.S. by 20-30%. Not because we’re cutting corners, but because we’re getting smarter about who really needs them.
What Should You Do?
If you’re 45 or older, get screened. That’s the standard recommendation. If you have a family history of colon cancer or polyps, start earlier. Don’t wait for symptoms. Most people with precancerous polyps feel fine.
If you’ve had a polyp removed, follow your doctor’s advice. Don’t skip your next colonoscopy. The fact that you had one means your risk is higher-not because you did something wrong, but because your body made a polyp. That’s not your fault. It’s biology.
And if you’ve had a serrated polyp? Don’t panic. Most people never develop cancer. But do take it seriously. This is your body’s way of telling you: pay attention. Stay on schedule. Keep screening. Because when it comes to colorectal cancer, catching it early isn’t just smart-it’s life-saving.
Myth vs. Fact
- Myth: All polyps turn into cancer. Fact: Only a small percentage do. Most are harmless if removed.
- Myth: If I feel fine, I don’t need a colonoscopy. Fact: Polyps cause no symptoms until they’re advanced.
- Myth: Serrated polyps aren’t dangerous. Fact: They cause 20-30% of colon cancers and are often missed.
- Myth: One colonoscopy means I’m safe forever. Fact: Risk depends on what was found. Follow-up is key.
Are all colorectal polyps cancerous?
No, most colorectal polyps are not cancerous. Adenomas and serrated lesions are precancerous, meaning they have the potential to turn into cancer over many years-but most never do. The key is removing them before they progress. Once removed, your risk drops significantly.
Can I tell the difference between adenomas and serrated lesions on my own?
No. Both types are invisible without a colonoscopy and microscopic analysis. You can’t feel them, see them, or notice them in your stool. That’s why screening is critical-even if you feel perfectly healthy.
Do I need a colonoscopy if I had a small hyperplastic polyp?
If the hyperplastic polyp was small (under 1 cm), located in the lower colon, and you have no other risk factors, you may only need routine screening every 10 years. But if you had multiple polyps, or if any were serrated or located in the right colon, your doctor may recommend earlier follow-up.
Why are serrated lesions harder to detect than adenomas?
Serrated lesions, especially sessile serrated adenomas, are often flat and grow on the right side of the colon, where the colon is wider and folds are deeper. They blend into the normal lining and don’t stick out like a mushroom. Standard colonoscopies can miss them, which is why advanced imaging and AI tools are now used to improve detection.
If I had one adenoma, will I get more?
Yes, having one adenoma increases your chance of developing more in the future. That’s why follow-up colonoscopies are recommended. It doesn’t mean you’re doomed-it means your colon is more likely to produce polyps, so monitoring is essential.
Can lifestyle changes reduce my risk of polyps?
Yes. Eating more fiber, limiting red and processed meats, staying active, avoiding smoking, and limiting alcohol can lower your risk. But lifestyle alone won’t prevent polyps if you’re genetically prone. Screening remains the most reliable way to stop cancer before it starts.


Adarsh Dubey
Interesting breakdown. I’ve had two colonoscopies in the last decade, and the docs never explained the difference between adenomas and serrated lesions-just said ‘remove and monitor.’ Now I get why some polyps come back faster than others. The flat, sneaky ones are terrifying.
Georgia Brach
Let’s be honest-this entire screening industry is driven by profit margins and fear-based marketing. The data on overdiagnosis and overtreatment of low-risk polyps is ignored because it doesn’t sell colonoscopies. We’re turning healthy people into patients.
Joe Jeter
Yeah, and don’t forget the 30% of people who get false positives from colonoscopies. You think you’re being proactive, but you end up with a scar, a bill, and a year of anxiety over a benign polyp that was never going to kill you. The medical system doesn’t care about collateral damage.
Sidra Khan
Okay but can we talk about how the word ‘serrated’ sounds like a horror movie villain? 😅 Like ‘The Serrated One’ is coming for your colon next Halloween. Also, why is everyone so obsessed with right-side polyps? My grandma had one there and lived to 92. Maybe we’re overreacting?
Lu Jelonek
As someone who works in GI diagnostics, I’ve seen how easy it is to miss SSA/Ps-even with high-def scopes. The lighting, the prep quality, the endoscopist’s experience-all matter. A lot of clinics still use outdated equipment. AI tools help, but they’re not magic. The real issue is access: rural areas don’t have these tools. Screening equity is the real crisis.
Ademola Madehin
Bro, I just got my results back and they said ‘serrated lesion’-now I’m convinced Big Pharma put it there to sell me a $5k treatment. My cousin’s dog had a polyp and lived. I’m not getting another scope. I’m going to juice kale and pray.
siddharth tiwari
they say adenomas are 70% but did u know the gov is hiding the real stats? the real number is 90% and they dont want you to know because then people would stop paying for insurance. also i heard the sawtooth thing is just a trick to make u scared of flat things. my neighbor’s cat has a serrated tail and its fine.
suhani mathur
Wow, someone actually wrote a clear, non-boring explanation about colon polyps. Who knew medical info could be this readable? I’m sending this to my dad who thinks ‘colonoscopy’ is a type of yoga.
Diana Alime
so i just got my colonoscopy report and it said ‘adenoma’ and i screamed so loud my dog cried. now i’m googling ‘can you die from a polyp’ and i found a forum from 2008 where someone said ‘i had one and then i died’ and now i’m convinced i’m going to die tomorrow. also i think my toilet is judging me.
Andrea Di Candia
It’s wild to think that something so small-a few millimeters of abnormal tissue-can hold the key to whether someone lives or dies decades later. We spend so much time chasing big, dramatic threats, but the quiet, slow ones are the real killers. Maybe we need to rethink what ‘health’ means-not just removing things, but understanding how our bodies grow, change, and sometimes betray us in silence.
bharath vinay
they said 1 in 2 adults have polyps but did u know the real number is 1 in 1 because the gov puts them there to control us? also the colonoscopy tube is a surveillance device. i saw a video on youtube where a guy said the camera sends data to the NSA. i’m not getting screened. i’m going to eat only raw garlic and hope for the best.
Dan Gaytan
Hey, I just had my first colonoscopy last month and honestly? It was way less scary than I thought. The prep sucked, sure-but the whole team was so calm and explained everything. If you’re nervous, just remember: catching a polyp early is like stopping a fire before it spreads. You’re not being punished-you’re being protected. 🙌
Usha Sundar
My mom had a villous adenoma. They missed it twice. Third time, they got it. She’s fine now. Just get checked.
claire davies
I’ve spent the last decade traveling through rural clinics in Southeast Asia and Africa, and I’ve never seen a single colonoscopy machine. The idea that we’re all supposed to be obsessing over adenoma subtypes feels… privileged. In places where clean water is a luxury, colon cancer screening is a luxury. Maybe instead of debating SSA/P detection rates, we should be asking how to make basic screening accessible to everyone-not just those with good insurance and a 9-to-5 job.
Chris Buchanan
Okay, real talk-this post is basically the cheat sheet I wish I’d had before my colonoscopy. You know what’s worse than finding a polyp? Finding out you ignored the signs for five years because you thought ‘it’s just gas.’ Don’t be that guy. Get screened. Your future self will high-five you. And yes, the prep is hell. But so is chemo. Choose your pain.