Generic vs Brand Identification in Pharmacy Systems: Best Practices for Accurate Medication Management
When a pharmacist fills a prescription, they’re not just handing out pills-they’re making a decision that can affect a patient’s safety, cost, and trust in their care. The difference between a brand-name drug and its generic version might seem small on the surface, but in pharmacy systems, it’s a complex puzzle of codes, regulations, and clinical judgment. Getting this right isn’t optional. It’s foundational.
What Makes a Generic Drug Really a Generic?
The U.S. Food and Drug Administration (FDA) doesn’t just say a generic is "similar"-it requires it to be the same. A generic drug must have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. It must also be bioequivalent, meaning it delivers the same amount of medicine into the bloodstream at the same rate. That’s not marketing speak. It’s science. The FDA requires generic manufacturers to prove this through rigorous testing, without repeating full clinical trials, thanks to the 1984 Hatch-Waxman Act.
But here’s where things get messy: not all generics are created equal in the eyes of the system. The FDA’s Orange Book lists every approved drug and assigns a Therapeutic Equivalence (TE) code. If you see an "AB" code, that means the generic is therapeutically equivalent to the brand. But "A" codes like "AN" or "AO" mean it’s equivalent only under certain conditions. Pharmacy systems need to read these codes correctly-or they risk making dangerous assumptions.
The NDC Code: Your System’s First Line of Defense
Every single drug product-brand or generic-has a National Drug Code (NDC). This 10- or 11-digit number is like a fingerprint. It breaks down into three parts: labeler code, product code, and package code. A change in any of those? That’s a new NDC. That means a generic version of lisinopril made by Company A has a different NDC than the same drug made by Company B. Even if they’re both AB-rated, they’re different products in the system.
Pharmacy software like Epic, Cerner, and Rx30 rely on NDCs to track inventory, process insurance claims, and prevent errors. But here’s the catch: if your system doesn’t update its NDC database regularly, you could be dispensing the wrong version. The FDA updates its NDC directory about 3,500 times a month. If your system is only synced weekly, you’re working with outdated data. That’s not just inconvenient-it’s risky.
Authorized Generics and Branded Generics: The Hidden Confusion
Not all generics are obvious. An authorized generic is the exact same drug as the brand, made by the same company, just sold under a different label. For example, the brand-name drug Propecia is made by Merck. Merck also sells an authorized generic version of finasteride under a different name. Same pill, same factory, same inactive ingredients. But your system might treat it as a separate product.
Then there are branded generics. These are generics that have a brand name-like Errin or Jolivette for birth control pills. They went through the ANDA process, so they’re not the original brand, but they’re marketed like one. Pharmacists often get confused because the packaging looks like a brand, the name sounds like a brand, and the patient expects it to be one. Systems that don’t clearly flag these as generics can lead to billing errors, insurance denials, and patient frustration.
Narrow Therapeutic Index Drugs: When Substitution Can Be Dangerous
Some drugs don’t play nice with substitutions. These are called narrow therapeutic index (NTI) drugs. A tiny change in blood levels-just 5%-can cause serious side effects or make the drug stop working. Warfarin, phenytoin, levothyroxine, and lithium fall into this category.
Pharmacy systems should have built-in safeguards. Systems like Epic’s Beacon Oncology block automatic substitution for these drugs. They don’t just flag them-they require a prescriber override. This isn’t bureaucracy. It’s protection. A 2021 ISMP report found 147 adverse events over 18 months tied to inappropriate generic substitution of warfarin. Most of those were avoidable if the system had properly flagged the risk.
Even then, it’s not foolproof. A 2019 U.S. Pharmacist study found that 0.8% of patients switching from brand to generic antiepileptic drugs reported issues-likely due to differences in inactive ingredients. Your system can’t see those. But your pharmacist can. That’s why education matters.
How Systems Should Be Set Up: Best Practices
Here’s what works in real-world pharmacies:
- Default to generics-unless there’s a clinical reason not to. ASHP recommends this. Most EHR systems already do. Your system should too.
- Integrate the FDA Orange Book API-not just a static file. Real-time updates mean you’re seeing the latest TE codes, new generic approvals, and withdrawn products. The FDA’s 2023 modernization initiative is pushing for this. Don’t wait.
- Flag authorized and branded generics clearly-don’t let them hide in plain sight. Use color coding, icons, or notes in the dispensing screen.
- Build in NTI alerts-no exceptions. If your system can’t do this, upgrade it.
- Train staff on the difference between generic, authorized generic, and branded generic. A 2022 survey found 78% of pharmacists were confused about birth control brands versus generics. That’s not a patient issue-it’s a system training issue.
Humana’s pharmacy system reduced brand use by 22% without safety issues by using automated therapeutic interchange alerts. That’s not magic. That’s smart design.
What Patients Need to Know
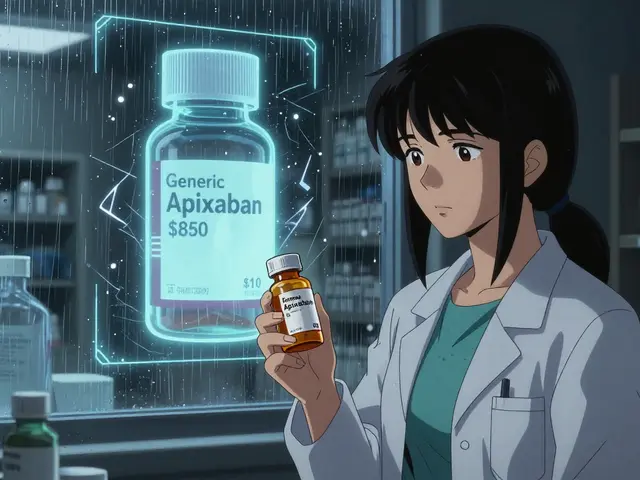
Patients aren’t dumb. They just don’t know what they don’t know. A 2022 Consumer Reports survey found that 89% of patients were satisfied with generics-when they were explained. Only 63% were satisfied when substitution happened without context.
Kaiser Permanente’s solution? A simple medication comparison tool in their patient portal. It shows the brand, the generic, the price difference, and a note: "Same active ingredient. FDA-approved equivalent." Result? A 37% drop in patients asking for the brand.
Don’t assume patients know generics are safe. Don’t assume they know they’re saving money. Give them the facts. A printed card. A quick verbal note. A digital pop-up. Anything that turns confusion into confidence.
State Laws and Compliance: It’s Not the Same Everywhere
California requires pharmacists to document why they didn’t substitute a generic. Texas lets pharmacists substitute without a note. New York has special rules for thyroid meds. CMS mandates that all Medicare Part D pharmacies hit 99.5% accuracy in TE code usage. That’s not a suggestion-it’s a requirement.
If your pharmacy operates in multiple states, your system must adapt. A one-size-fits-all configuration will get you fined. Make sure your software can toggle rules by location. If it can’t, you’re operating blind.
The Future: AI, Pharmacogenomics, and Real-Time Data
The next wave of pharmacy systems won’t just identify drugs-they’ll predict problems. A 2023 study in the Journal of the American Medical Informatics Association showed AI systems that analyze prescription patterns can flag potential equivalence issues with 87.3% accuracy. Imagine a system that notices a patient keeps switching between three different levothyroxine generics and flags it for review.
And it’s not just about the drug. The FDA’s Precision Medicine Initiative is exploring whether genetic markers could one day tell us which patients need the brand version of a drug-even if it’s technically equivalent. That’s not science fiction. It’s coming.
Right now, the market for pharmacy identification software is growing at 12.7% a year. LexID and Medi-Span power most hospital systems. But independent pharmacies? Only 63% have full systems in place. That’s a gap. And it’s dangerous.
Final Thought: Accuracy Isn’t Optional
Generic drugs save the U.S. healthcare system nearly $2 trillion every decade. They’re safe. They’re effective. But only if the system knows which one it’s giving out. A wrong NDC. A missed TE code. A hidden branded generic. One small error can ripple into a patient’s health, a pharmacy’s reputation, or a legal claim.
The tools are there. The data is available. The standards are clear. What’s missing is consistent execution. If your pharmacy system isn’t set up to handle generic vs brand identification with precision, you’re not just behind-you’re exposed.
Fix the system. Train the team. Educate the patient. That’s not just best practice. It’s the baseline.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. They must deliver the same amount of medicine into the bloodstream at the same rate. Studies, including one published in PLOS ONE, show no significant difference in outcomes between generic and authorized generic users across multiple medications.
What does an AB rating mean in the FDA Orange Book?
An "AB" rating means the generic drug is therapeutically equivalent to the brand-name reference drug. It has been proven to be bioequivalent and can be substituted without clinical concern. Other ratings like "AN," "AO," or "BX" indicate limited or no substitution-these require special attention from pharmacists.
Why do some pharmacies still dispense brand-name drugs when generics are available?
Sometimes, the prescriber writes "Do Not Substitute" on the prescription. Other times, the patient has had a bad reaction to a generic in the past, or the drug is a narrow therapeutic index medication like warfarin or levothyroxine. In some cases, branded generics are marketed to look like the original brand, confusing both patients and pharmacists. Systems must allow overrides and flag these exceptions clearly.
Can inactive ingredients in generics cause problems?
Yes. While generics must match the active ingredient, their inactive ingredients (fillers, dyes, preservatives) can differ. In rare cases, these can trigger allergies or affect absorption. A 2019 study found 0.8% of patients switching to generic antiepileptic drugs reported new side effects. Pharmacy systems can’t detect this-but pharmacists can ask patients about reactions after a switch.
How often should pharmacy systems update their drug databases?
At minimum, weekly. The FDA updates its NDC directory about 3,500 times a month. The Orange Book is updated monthly, and new generic approvals are published weekly. Systems that sync only quarterly or monthly risk dispensing outdated or incorrect drug information. Real-time API integration is the gold standard.
What’s the difference between an authorized generic and a branded generic?
An authorized generic is made by the original brand manufacturer but sold under a generic label-same pill, same factory. A branded generic is made by a different company, went through the ANDA process, but carries a proprietary brand name (like Errin for birth control). Authorized generics are identical to the brand; branded generics are chemically equivalent but marketed differently. Pharmacy systems must distinguish between them to avoid billing and patient confusion.
Do all states allow pharmacists to substitute generics?
Yes-49 states allow pharmacists to substitute therapeutically equivalent generics without prescriber approval. California is the exception: it requires documentation of the reason if substitution is refused. Pharmacy systems must be configured to follow state-specific rules automatically to remain compliant.
How can pharmacies improve patient trust in generics?
By explaining it clearly. Use simple visuals: "Same medicine. Lower price." Provide printed materials, offer brief verbal explanations, or use digital tools like Kaiser Permanente’s Medication Comparison feature. When patients understand generics are FDA-approved and equivalent, satisfaction jumps from 63% to 89%.



William Liu
Pharmacy systems need to stop treating generics like second-class citizens. The science is solid-FDA approval isn’t a suggestion. If your software can’t handle NDC updates in real time, it’s not just outdated, it’s dangerous.
Frank Drewery
I’ve seen pharmacists get tripped up by branded generics more times than I can count. That Errin package looks just like Yaz. Patients think they’re getting the brand. Systems need to scream ‘GENERIC’ in bright red, not whisper it in tiny font.
Danielle Stewart
One thing I’ve learned working in community pharmacy: patients don’t care about TE codes. They care about whether their pill looks different or costs less. If we don’t explain it simply, they assume we’re cutting corners. A printed card with ‘Same medicine. Lower price.’ makes all the difference.
It’s not about the system-it’s about the conversation. We’re the last line of defense against misinformation.
Training staff isn’t optional. A 2022 survey showed 78% of pharmacists were confused about birth control brands vs. generics. That’s on us.
Stop assuming patients know the difference. They don’t. And that’s not their fault.
Kaiser’s patient portal tool? Genius. Simple visuals. Clear language. No jargon. That’s how you build trust.
When patients understand generics are FDA-approved equivalents, satisfaction jumps from 63% to 89%. That’s not magic. That’s communication.
We can fix this. But only if we stop treating patients like they’re stupid.
It’s not about the drug. It’s about the dignity of the interaction.
Every time we hand over a generic without explanation, we’re silently telling them their health doesn’t matter enough to warrant clarity.
That’s not just bad practice. It’s unethical.
Let’s change that.
mary lizardo
It is profoundly irresponsible to suggest that generic substitution is universally safe without acknowledging the profound regulatory arbitrage inherent in the Hatch-Waxman Act. The FDA’s bioequivalence thresholds are statistically permissive, permitting up to a 20% variance in AUC and Cmax-conditions under which pharmacokinetic divergence may manifest clinically in vulnerable populations, particularly the elderly or those with hepatic impairment. Furthermore, the absence of mandatory post-marketing surveillance for generics creates a systemic blind spot that compromises patient safety. This article exhibits a dangerous naivete regarding pharmaceutical regulation.
jessica .
THEY WANT YOU TO THINK GENERICS ARE THE SAME SO THEY CAN SELL YOU POISON FROM CHINA. THE FDA IS IN BED WITH BIG PHARMA. THEY LET THEM USE TOXIC FILLERS THAT CAUSE CANCER. MY COUSIN GOT SICK AFTER A GENERIC AND THEY COVERED IT UP. THEY’RE HIDING THE TRUTH. THE NDC DATABASE IS MANIPULATED. TRUST NO ONE.
Ryan van Leent
Why are we even talking about this like it’s complicated? If the doctor writes brand only then use brand. If they don’t then use generic. End of story. Stop overengineering everything. Your system should just flag NTI drugs and leave the rest alone. Stop making pharmacists into data entry clerks. We didn’t go to school for this.
Sajith Shams
India manufactures over 60% of the world’s generic drugs. The US imports 80% of its API from China and India. If your pharmacy system can’t track the origin of the API, you’re flying blind. No one talks about this. The FDA doesn’t require country-of-origin labeling on generics. That’s a massive gap. You think a 10-digit NDC tells you where the active ingredient came from? It doesn’t. Your system is lying to you.
Real-time API updates? Useless if the source data is corrupted. You need blockchain-level traceability, not just FDA syncs. Until then, you’re gambling with people’s lives.
Adrienne Dagg
Can we just agree that branded generics are the worst? 😤 I had a patient cry because she thought she was getting the brand and got Errin instead. She said it "felt different." It’s the same damn pill. But the packaging? Looks like a luxury product. That’s the problem. Systems need to slap a giant "GENERIC" sticker on the screen. 🚨
Erica Vest
There’s a critical distinction between therapeutic equivalence and clinical interchangeability that this post glosses over. AB-rated does not automatically mean clinically interchangeable in every patient population. For NTI drugs like levothyroxine, even minor excipient differences can affect absorption in patients with malabsorption syndromes or gastric hypochlorhydria. The FDA’s bioequivalence criteria are population-based averages-not individual guarantees. Pharmacy systems must not only flag NTI drugs but also maintain a patient-specific substitution history. This requires longitudinal data tracking, not just static TE codes.
Additionally, the 0.8% adverse event rate in antiepileptic generics cited in the 2019 study is statistically significant when scaled across millions of prescriptions. That’s not noise-it’s signal. Systems should integrate patient-reported outcome (PRO) modules to capture post-substitution symptoms. Without this feedback loop, we’re operating in the dark.
Real-time API integration with the FDA’s Orange Book is non-negotiable. But so is closing the loop with pharmacovigilance data. We need to treat pharmacogenomic variability as a first-class concern, not an afterthought.
Chris Davidson
Generic drugs are fine if you don’t mind your meds working inconsistently. The FDA lets them get away with 20% variation. That’s not science. That’s a loophole. Why are we still pretending this is safe? Systems should block all substitutions unless the prescriber explicitly approves. Period. No more excuses.
Kinnaird Lynsey
It’s funny how we treat pharmacy systems like they’re infallible. The truth is, most of them are barely functional. I’ve seen systems that still use 2017 NDC data. I’ve seen pharmacists manually override flags because the software won’t let them dispense a generic that’s technically AB-rated but the patient’s insurance won’t cover it. The system isn’t broken-it’s being used by humans who are exhausted. Maybe the real issue isn’t the software. It’s the burnout.
Maybe we need to stop trying to automate everything and just give pharmacists more time to talk to patients. The tech is there. But the human bandwidth? Not so much.
Glen Arreglo
As someone who’s worked in pharmacies across three countries, I’ve seen how this plays out differently everywhere. In the US, it’s about cost. In Germany, it’s about regulation. In Australia, it’s about trust. The real solution isn’t software-it’s cultural. We need to normalize generics as the default everywhere, not just in the US. But that requires education, not just system updates.
Patients aren’t the problem. The stigma is.
shivam seo
Generic drugs are just corporate greed dressed up as healthcare. The FDA is a puppet. The NDC system is a joke. You think your pharmacy software is protecting you? It’s just making the profit margins for Big Pharma bigger. Wake up. This isn’t medicine. It’s a business model.
benchidelle rivera
Let’s be real: most independent pharmacies can’t afford real-time API integrations. They’re stuck with weekly or monthly updates because their software vendor charges $15,000 a year for live data. That’s not a technical gap-it’s an equity gap. The people most at risk? Low-income patients in rural areas. They’re the ones getting outdated NDCs and wrong TE codes. This isn’t just about best practices. It’s about justice.
Fix the system? Yes. But also fund it. The government should subsidize API access for small pharmacies. Not as a perk. As a public health imperative.
Anna Sedervay
The entire premise of this article is dangerously flawed. The FDA’s bioequivalence standards are not based on clinical outcomes-they are based on statistical tolerances that permit pharmacokinetic divergence in up to 20% of individuals. This is not science. It is regulatory capitulation to multinational pharmaceutical conglomerates. Furthermore, the so-called "authorized generics" are merely brand-name drugs repackaged under a different label to circumvent antitrust scrutiny and maintain market dominance. The distinction between "branded generic" and "authorized generic" is a semantic sleight-of-hand designed to confuse clinicians and patients alike. The system isn’t broken-it was designed this way. And you are complicit by normalizing it.
Chris Davidson
They just said the same thing in the article. Why are you still arguing? Just use the brand if you’re scared. No one’s forcing you.