Deprescribing Research: What Happens When You Reduce Medications in Older Adults
Deprescribing Medication Risk Checker
Check Your Medications
This tool helps you identify medications that might be inappropriate for older adults based on the Beers Criteria. It's not a substitute for professional medical advice.
Results & Recommendations
Select medications to see their potential risk level and recommendations.
Current Risk Level
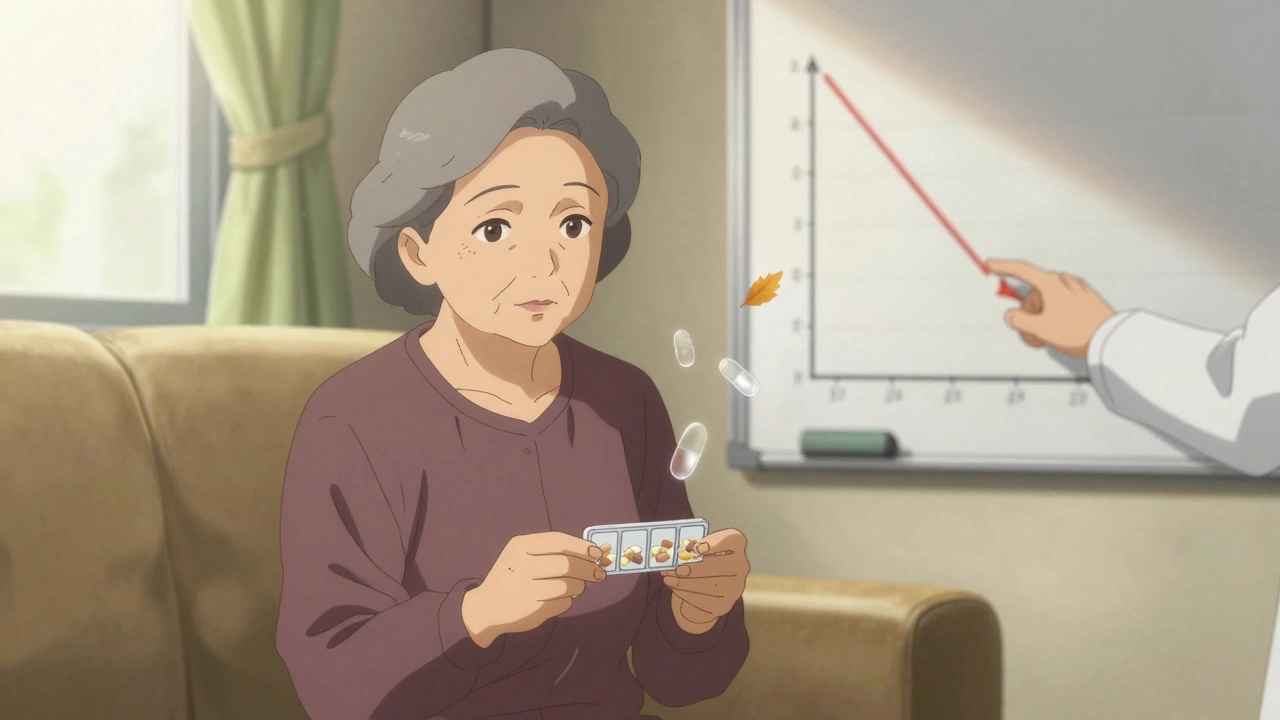
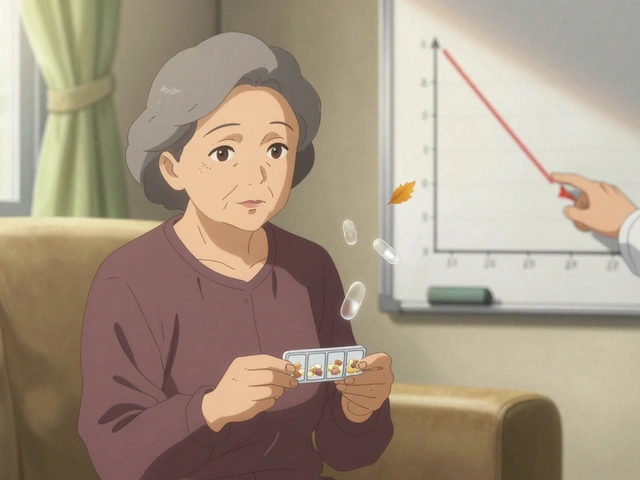
Every year, millions of older adults take more medications than they need. Some were prescribed years ago for conditions that have changed or disappeared. Others were added one at a time by different doctors, with no one stepping back to ask: Do I still need this? That’s where deprescribing comes in-not as a side note, but as a deliberate, evidence-backed process to stop drugs that no longer help, or worse, harm.
What Exactly Is Deprescribing?
Deprescribing isn’t just quitting pills. It’s a structured, step-by-step review of every medication a person is taking, with one goal: improve quality of life by removing what’s unnecessary or risky. The American Geriatrics Society defines it as the planned and supervised process of reducing or stopping medications that might be causing harm or offering no real benefit. This isn’t about cutting corners-it’s about treating medication use with the same care as prescribing it.Think of it this way: when a doctor starts a new drug, they check your symptoms, your other meds, your kidney function, your goals. Deprescribing does the same thing-but in reverse. You ask: What was this for? Does it still make sense? What happens if we stop it?
Who Benefits Most from Deprescribing?
Not everyone needs to cut back. But certain groups see the biggest gains:- Older adults taking five or more medications daily (about 40% of seniors in the U.S.)
- People with frailty, dementia, or advanced illness
- Those experiencing new symptoms like dizziness, confusion, or falls that could be drug side effects
- Patients on preventive drugs like statins or blood pressure meds when life expectancy is short
- Anyone on high-risk combinations-like benzodiazepines with opioids, or multiple drugs that slow the brain
One study found that nearly 20% of older adults take ten or more pills every day. That’s not just inconvenient-it’s dangerous. Each extra pill increases the chance of a bad reaction, hospital visit, or even death.
The Five Steps of Safe Deprescribing
Deprescribing doesn’t happen by accident. It follows a clear clinical roadmap:- Identify potentially inappropriate medications. Use tools like the Beers Criteria, updated in 2023, to flag drugs that are risky for older adults-like long-term benzodiazepines, anticholinergics, or NSAIDs.
- Decide if stopping is possible. Ask: Is this drug still helping? Is the risk greater than the benefit? For example, a statin for primary prevention in someone with 18 months to live may not be worth the side effects.
- Plan how to taper. Never stop cold turkey. Some drugs, like antidepressants or steroids, need slow reduction over weeks or months to avoid withdrawal symptoms.
- Monitor closely. Watch for changes in mood, sleep, pain, or function. Some symptoms return quickly. Others take time. Document everything.
- Record the outcome. Did the patient feel better? Worse? No change? This data helps future decisions-not just for them, but for others too.
Key point: Only stop one drug at a time. If you cut three pills and the patient feels worse, you won’t know which one caused the problem.
What Does the Research Say About Outcomes?
Early studies focused on one thing: How many pills can we remove? The answer? A lot. A 2023 review in JAMA Network Open found that deprescribing interventions reduced the average number of medications from 9.74 to about 8.7 per person. That might sound small-but scale it up. A primary care doctor with 2,000 patients, half of them on multiple meds, could safely remove over 140 unnecessary prescriptions in a year.But the real question isn’t how many pills disappear-it’s what happens to the person. Here’s what the data shows:
- Fewer falls: Stopping sedatives, antipsychotics, or blood pressure meds linked to dizziness cuts fall risk by up to 30% in some trials.
- Better mental clarity: Patients on multiple anticholinergics (common in allergies, bladder meds, and sleep aids) often report improved memory and focus after stopping.
- Lower hospital admissions: One study showed a 17% drop in ER visits after a structured deprescribing program in nursing homes.
- No increase in death rates: Despite fears, no major study has found that deprescribing increases mortality-even in frail elderly patients.
But here’s the catch: most studies only lasted 6 to 12 months. We still don’t know the full long-term impact. That’s why researchers like Dr. Dan Gnjidic call for larger, longer trials that track actual outcomes-like mobility, cognition, and survival-not just pill counts.
Why Don’t More Doctors Do This?
It’s not that they don’t want to. It’s that the system doesn’t make it easy.- No time: A 15-minute visit doesn’t leave room to review 12 medications.
- No tools: Most electronic health records don’t flag potentially inappropriate drugs or suggest alternatives.
- No reimbursement: Insurance doesn’t pay for medication reviews unless they’re tied to a new diagnosis.
- Patient pressure: Many patients think more meds = better care. They’re scared to stop anything.
One study found that patients want to take fewer pills-but only if their doctor brings it up. Left to their own devices, most won’t ask. They assume their meds are all necessary.
What’s Changing Now?
The tide is turning. Here’s what’s new in 2025:- Electronic health record alerts: Some clinics are testing tools that flag high-risk drug combinations and suggest deprescribing options during chart reviews. Pilot programs saw a 15% drop in inappropriate prescriptions.
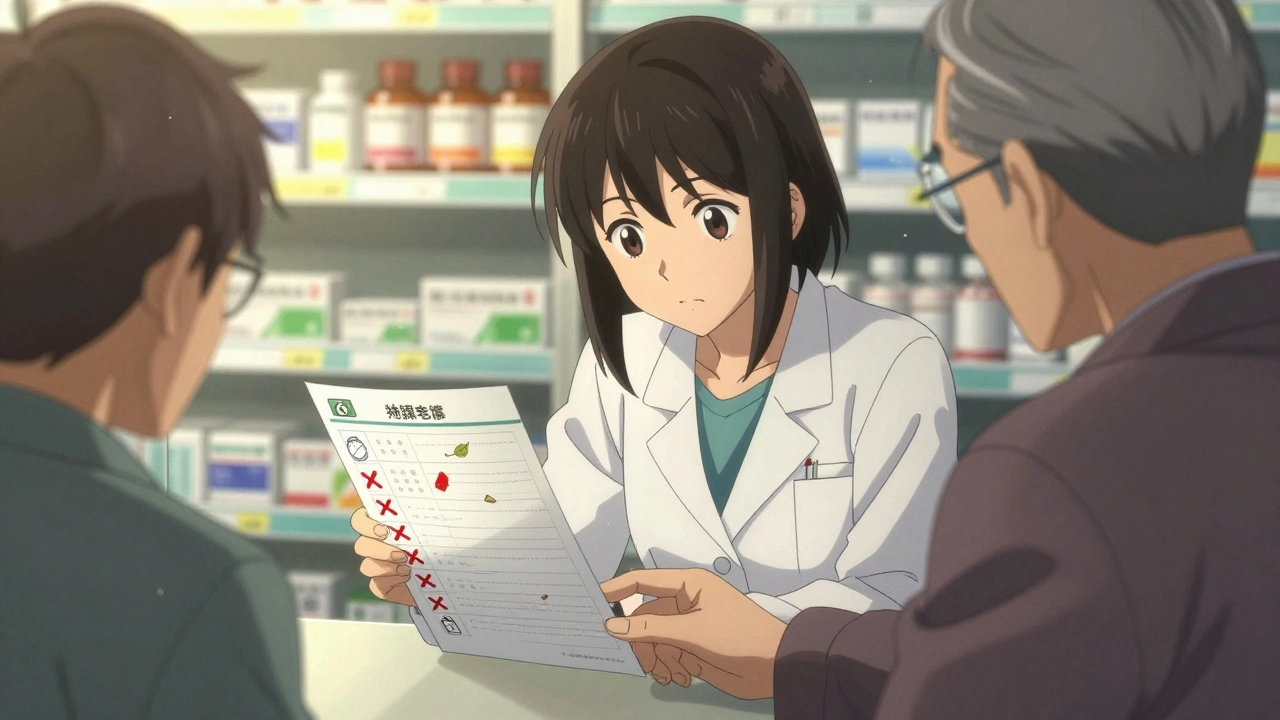
- Pharmacist-led programs: In hospitals and community pharmacies, pharmacists are now trained to initiate deprescribing conversations-especially after discharge.
- Shared decision-making tools: Websites like deprescribing.org offer printable guides patients can bring to appointments. Over 500,000 have been downloaded since 2015.
- Genetic testing integration: Early research is exploring how drug metabolism genes (like CYP2D6 or CYP2C19) can help predict who’s more likely to have side effects from certain drugs, making deprescribing more personalized.
And it’s not just about cutting pills-it’s about shifting the mindset. Instead of asking, What drug should we add? the new question is: What drug can we safely remove?

What Patients Should Know
If you or a loved one is on multiple medications:- Ask your doctor: “Is this still necessary?” Don’t wait for them to bring it up.
- Bring a full list of everything you take-including vitamins, supplements, and over-the-counter drugs.
- Ask: “What happens if I stop this?” and “What signs should I watch for?”
- Don’t stop anything on your own. Even “harmless” drugs like melatonin or ibuprofen can cause problems when stopped abruptly.
- Remember: A pill that helped five years ago might not help now. Your body, your health, and your goals have changed.
One woman in her late 70s stopped her daily blood pressure pill after her doctor explained her numbers were fine and the drug was making her dizzy. Within two weeks, she stopped falling. She didn’t need the pill anymore-but she’d been too afraid to ask.
The Bigger Picture
By 2030, one in five Americans will be over 65. That means more people on more meds. Without action, we’ll see more hospitalizations, more falls, more confusion-all tied to drugs meant to help.Deprescribing isn’t about taking away care. It’s about restoring balance. It’s about giving people back their energy, their clarity, and their safety. It’s about treating medication like a tool-not a default.
The science is clear: stopping the wrong drugs can be just as important as starting the right ones. The challenge now is making it standard-not optional.
Is deprescribing safe for older adults?
Yes, when done properly. Research shows that stopping unnecessary medications in older adults reduces falls, confusion, and hospital visits without increasing the risk of death. The key is doing it slowly, one drug at a time, with close monitoring. Studies have found no rise in mortality-even in frail patients-when deprescribing is guided by clinical judgment and patient goals.
Can I stop my meds on my own if I think they’re not helping?
No. Some medications, like antidepressants, blood pressure drugs, or steroids, can cause serious withdrawal symptoms if stopped suddenly. Even over-the-counter sleep aids or pain relievers can cause rebound effects. Always talk to your doctor or pharmacist before making any changes. They can help you taper safely and watch for side effects.
How do I know if a medication is no longer needed?
Ask these questions: Why was this prescribed? Has my condition changed? Is this drug still helping me feel better or live longer? Is it causing side effects like dizziness, fatigue, or memory problems? If the answer to any of these is unclear or negative, it’s worth discussing deprescribing. Tools like the Beers Criteria or resources from deprescribing.org can help guide the conversation.
Do I need to see a specialist to start deprescribing?
Not necessarily. Your primary care doctor, pharmacist, or nurse practitioner can start the process. Many hospitals now have geriatric pharmacists who specialize in medication reviews. If your doctor isn’t familiar with deprescribing, bring resources from deprescribing.org or mention the American Geriatrics Society’s Beers Criteria. Most clinicians are willing to learn-it’s just not always taught in medical school.
Will stopping meds make my condition worse?
Sometimes, symptoms return-but that doesn’t mean the drug was helping. For example, a statin might lower cholesterol, but if you’re 90 with limited mobility and no heart disease, the benefit is tiny. If stopping it causes your cholesterol to rise again, that’s fine-you’re not at risk for a heart attack. The goal isn’t perfect numbers; it’s living well. If a symptom returns, you can always restart. But if nothing changes? That’s a sign the drug wasn’t doing anything in the first place.
Is deprescribing only for older adults?
While most research focuses on seniors, deprescribing applies to anyone on long-term medications. Younger people with chronic conditions, those on multiple psychiatric drugs, or patients recovering from surgery may also benefit. The principles are the same: review every drug, question its purpose, and remove what’s no longer needed. Age isn’t the only factor-medication burden and life goals matter more.
What Comes Next?
The future of deprescribing lies in making it routine-not rare. Health systems are starting to build it into care workflows: automated alerts in EHRs, pharmacist-led medication reviews, and patient education tools. The goal is simple: stop treating pills like a checklist, and start treating them like a conversation.Medications aren’t harmless. They’re powerful tools-with risks. And sometimes, the most powerful thing you can do is not take one at all.




Shubham Pandey
My grandma takes 12 pills a day. No one ever asked if she needed them. She just stopped one-her blood pressure med-after her dizziness got bad. Now she walks without a cane. Who knew?
Elizabeth Farrell
I’ve been watching my mom go through this for years. She’s 82, on everything from statins to sleep aids to a pill for the side effects of another pill. It’s exhausting. I finally sat down with her pharmacist last month and we went through every single one. We cut four. She’s sleeping better, her memory’s clearer, and she hasn’t fallen once in six months. It’s not about taking away care-it’s about giving back her life. Honestly? I wish every family had access to this kind of review. It’s not magic, it’s just common sense. And yet, it’s still so rare.
Doctors are stretched thin, I get it. But if we trained pharmacists to lead these conversations after hospital discharges, or built simple checklists into primary care visits, this could become routine. Not a favor. Not a bonus. Just part of the standard of care. We treat every other part of aging with precision-why not meds?
Sheryl Lynn
How quaint. The modern medical-industrial complex has turned elderly patients into walking pharmacopeias, and now we’re performing a kind of pharmaceutical austerity-like we’re trimming the fat off a bloated corpse of a system. Deprescribing isn’t innovation; it’s the belated recognition that we’ve been overmedicating the elderly like they’re lab rats in a perpetual clinical trial. The Beers Criteria? A noble attempt at bureaucratic triage. But let’s not pretend this is about patient autonomy. It’s about cost containment dressed in the velvet gloves of geriatric compassion. Still… I’ll admit, the 30% drop in falls? That’s poetic justice.
Now if only we could deprescribe the entire ethos of ‘more is better’ from medical education… but then, who’d profit?
Paul Santos
Deprescribing? More like de-industrializing pharmacology 😏
It’s ironic-we’ve got AI predicting drug interactions in real time, yet we still let 70-year-olds take 10 meds because ‘it’s always been done.’ The real scandal isn’t the pills-it’s the lack of systemic reflection. We prescribe like we’re playing Jenga, and then act shocked when the tower falls (literally, in the case of falls).
Pharmacist-led reviews? Yes. But we need EHRs that auto-flag polypharmacy like a spam filter. Until then, we’re just rearranging deck chairs on the Titanic… with a 15-minute visit and a clipboard. 🤷♂️
John Morrow
Let’s be brutally honest: deprescribing is a band-aid on a systemic hemorrhage. The fact that we even need a formal protocol to stop giving people drugs they don’t need exposes the rot at the core of American healthcare. Every single one of these medications was prescribed by someone who got paid to prescribe, not to think. And now we’re surprised when the elderly are walking pharmacies with dementia? Shocking.
Studies show no increase in mortality? Of course not. Because the drugs being removed were never saving lives-they were just padding billing codes. Statins for a 90-year-old with no heart disease? That’s not medicine. That’s corporate medicine. And the fact that patients are too scared to ask if they can stop their meds? That’s not fear of illness-it’s fear of the system. They’ve been conditioned to believe that pills = care. That’s the real tragedy.
And don’t even get me started on the ‘shared decision-making tools’-like a PDF from deprescribing.org is going to fix a medical culture that rewards volume over virtue. We’re treating symptoms of a disease we refuse to diagnose: profit-driven healthcare. Until that changes, deprescribing is just a PR campaign with a clinical veneer.
Also, CYP2D6 testing? Cute. But if your doctor doesn’t even know what ‘anticholinergic burden’ means, you’re not getting precision medicine-you’re getting lucky.
ruiqing Jane
I’ve worked in geriatric care for 18 years, and I’ve seen the same pattern over and over: a patient comes in with a new diagnosis, gets a new med, then another, then another-until their pill organizer looks like a science experiment. I’ve watched people become drowsy, confused, unsteady-all because we never paused to ask, ‘Is this still helping?’
One of my patients, Mrs. Lin, was on six meds for hypertension, anxiety, insomnia, and ‘preventive’ statins. She was 89, lived alone, and hadn’t left her house in months. We tapered her off the benzos and the beta-blocker. Within three weeks, she started gardening again. Said she could finally hear the birds. No new diagnosis. No new treatment. Just… less noise.
This isn’t radical. It’s basic. We don’t keep giving someone a coat they’re sweating in just because it was cold last winter. Why do we do it with pills?
And yes-pharmacists should lead this. They’re the only ones trained to see the whole picture. Primary care docs are drowning. Let them focus on what they’re best at: listening. The rest? Hand it to the experts.
Also: if your doctor says ‘it’s fine to keep taking it,’ ask them why. Not ‘is it safe?’ but ‘is it useful?’ There’s a difference.
Thank you for writing this. It’s about time we stopped treating pills like blessings and started treating them like tools-with consequences.
Fern Marder
OMG I just told my dad to stop his nighttime antihistamine 😭 He’s 76 and has been taking diphenhydramine for ‘sleep’ since 2010. Turns out it’s making him foggy all day and he’s been misplacing his keys because of it. We cut it cold turkey (oops, bad idea, but he was so tired of the grogginess) and now he’s napping naturally at 8pm like a normal human. I’m crying happy tears 🥹
Also-why does no one talk about how many seniors are on OTC meds that are totally unnecessary? I found three bottles of ‘joint support’ supplements in his cabinet that cost $80/month. No evidence. Just marketing. We threw them out. He didn’t even notice.
Deprescribing = liberation. 🙌
P.S. Bring back the paper pill organizer. Easier than apps when you’re 80.
Sandi Allen
THIS IS A GOVERNMENT PLOT. THEY WANT YOU TO STOP TAKING YOUR MEDS SO YOU DIE FASTER AND SAVE MONEY ON SOCIAL SECURITY. THE PHARMA COMPANIES ARE IN ON IT TOO-THEY KNOW IF YOU STOP THE PILLS, YOU WON’T NEED AS MANY DOCTOR VISITS, AND THEY’LL LOSE BILLIONS. THEY’RE USING ‘DEPRESCRIBING’ AS A CODE WORD FOR ‘KILL THE ELDERLY.’ I SAW A VIDEO ON TRUTH SOCIAL WHERE A DOCTOR SAID ‘WE NEED TO REDUCE MEDICATIONS TO CONTROL POPULATION GROWTH.’ IT’S NOT ABOUT HEALTH-IT’S ABOUT CONTROL.
MY GRANDMA TOOK HER MEDS AND LIVED TO 94. IF YOU STOP THE PILLS, YOU’RE DOOMED. DON’T LET THEM MANIPULATE YOU.
THEY’LL TAKE YOUR MEDS, THEN YOUR HOME, THEN YOUR SOCIAL SECURITY. NEXT THING YOU KNOW, YOU’RE IN A ‘CARE HOME’ WITH NO PILLS AND NO VOICE.
STAY VIGILANT. QUESTION EVERYTHING. KEEP YOUR PILLS.
PS: I’M NOT A CONSPIRACY THEORIST-I JUST DO MY RESEARCH.
John Webber
my uncle just stopped his blood pressure pill cause he thought it made him tired. he got dizzy and fell and broke his hip. now he’s in rehab. don’t just stop stuff. talk to a doc. i know people think more pills = bad but some of em save your life. my mom’s on 8 and she’s still walking around. so yeah. don’t be dumb.
Chris Wallace
I’ve been thinking about this a lot since my aunt went through a deprescribing program last year. She was on nine meds-some for conditions that had resolved years ago. The process felt… quiet. Not dramatic. No fanfare. Just her and her pharmacist going through each pill like they were sorting through old letters.
She stopped a statin she’d been on since 65. Her cholesterol went up a bit. She didn’t care. She said she’d rather feel awake than have a number on a chart. She started walking every morning again. Took up painting. Said she could finally hear the wind.
It made me wonder-how many of us are living in a fog of unnecessary pills? Not because they’re harmful, but because we never asked if they still mattered.
I’m not a doctor. I don’t have answers. But I’m starting to think that sometimes, the most compassionate thing we can do is not give someone another pill… but help them let go of one they’ve been holding onto for too long.
Also-I’m gonna ask my own doctor about my sleep aid. I’ve been taking it for five years. I don’t even remember why I started.
william tao
Deprescribing: A necessary, yet fundamentally inadequate, corrective mechanism in a healthcare ecosystem that has long abandoned the Hippocratic Oath in favor of the CPT code. The fact that we require a formalized, evidence-based protocol to cease administering pharmacological interventions that confer no measurable benefit to the patient is not a triumph of clinical reasoning-it is an indictment of a medical-industrial complex that has transformed human physiology into a revenue stream.
That the American Geriatrics Society has felt compelled to codify the act of *not prescribing* as a clinical discipline speaks volumes. We have become so normalized to polypharmacy that its reduction is now labeled ‘intervention.’
Let us not mistake this for progress. It is merely the faint echo of a long-overdue reckoning.
And yet-
...I am grateful for the Beers Criteria. For the pharmacist-led reviews. For the patient handouts. For the slow, grinding shift in consciousness.
Perhaps, in time, we will reach a point where deprescribing is not an ‘initiative’-but the default.
Until then, we are merely cleaning up the wreckage of a system that forgot its purpose.
Elizabeth Farrell
Thank you for sharing this, Chris. I’ve been thinking about your aunt’s story. It reminds me of my own mom-she used to say she took her meds ‘just in case.’ I finally asked her: ‘Just in case of what?’ She paused… and said, ‘I don’t know anymore.’
That’s the real problem. We’re not just overmedicating-we’re over-normalizing dependency. Pills have become emotional security blankets. We’re scared to stop because we think we’ll fall apart without them. But sometimes… we’re just afraid of being alone with our own bodies again.
I’m going to bring your aunt’s story to my next family meeting. Maybe we can all start asking: ‘What am I taking… and why?’