Antifungals and Liver Safety: What You Need to Know About Drug Interactions and Risks
When you’re fighting a stubborn fungal infection-whether it’s nail fungus, a yeast infection, or something more serious like invasive aspergillosis-you’re counting on antifungals to work. But behind their effectiveness lies a quiet danger: liver damage. Many people don’t realize that these common medications can quietly harm the liver, sometimes without warning. And when you’re taking other drugs, the risk doesn’t just go up-it can multiply.
Which Antifungals Are Most Likely to Hurt Your Liver?
Not all antifungals are created equal when it comes to liver safety. The big four classes are azoles, polyenes, echinocandins, and allylamines. Each carries different risks.Among azoles-fluconazole, itraconazole, voriconazole, posaconazole, and ketoconazole-ketoconazole stands out for its danger. It’s so risky that the FDA restricted its use in 2013 and the European Medicines Agency pulled it off the market entirely in 2013. Studies show about 1 in 500 people taking ketoconazole develop serious liver injury. Some cases led to liver failure or transplant. That’s why it’s now only used as a last resort for rare fungal infections when nothing else works.
Voriconazole and itraconazole aren’t far behind. Data from the FDA’s adverse event database shows they cause liver injury more often than fluconazole. Voriconazole, especially, can spike liver enzymes within 2 to 8 weeks of starting treatment. If you’re on this drug, your doctor should check your liver function every week during the first month.
Fluconazole is the safest of the azoles, but it’s not risk-free. If you’re taking it for more than two weeks-or if you already have liver disease, drink alcohol, or take other liver-stressing meds-your risk goes up. That’s why monitoring is still needed, even with this “safer” option.
Terbinafine, used mostly for nail fungus, has a lower overall risk-about 0.1% of users. But here’s the catch: when it does hurt the liver, it can be severe. There’s a black box warning for it because of rare cases of liver failure. Most injuries show up within the first six weeks, which is why labs are often checked at 4 to 6 weeks into treatment.
Echinocandins like caspofungin and micafungin were once thought to be liver-safe. But newer data tells a different story. While micafungin appears to be the gentlest among them, anidulafungin has the highest mortality rate among antifungals linked to liver injury-50% in some cases. That doesn’t mean it’s deadly for half the people who take it. It means that among the small group who develop severe liver injury on this drug, half die. Why? Likely because it’s often given to patients already very sick, with existing liver problems. That’s called “indication bias.”
How Do These Drugs Damage the Liver?
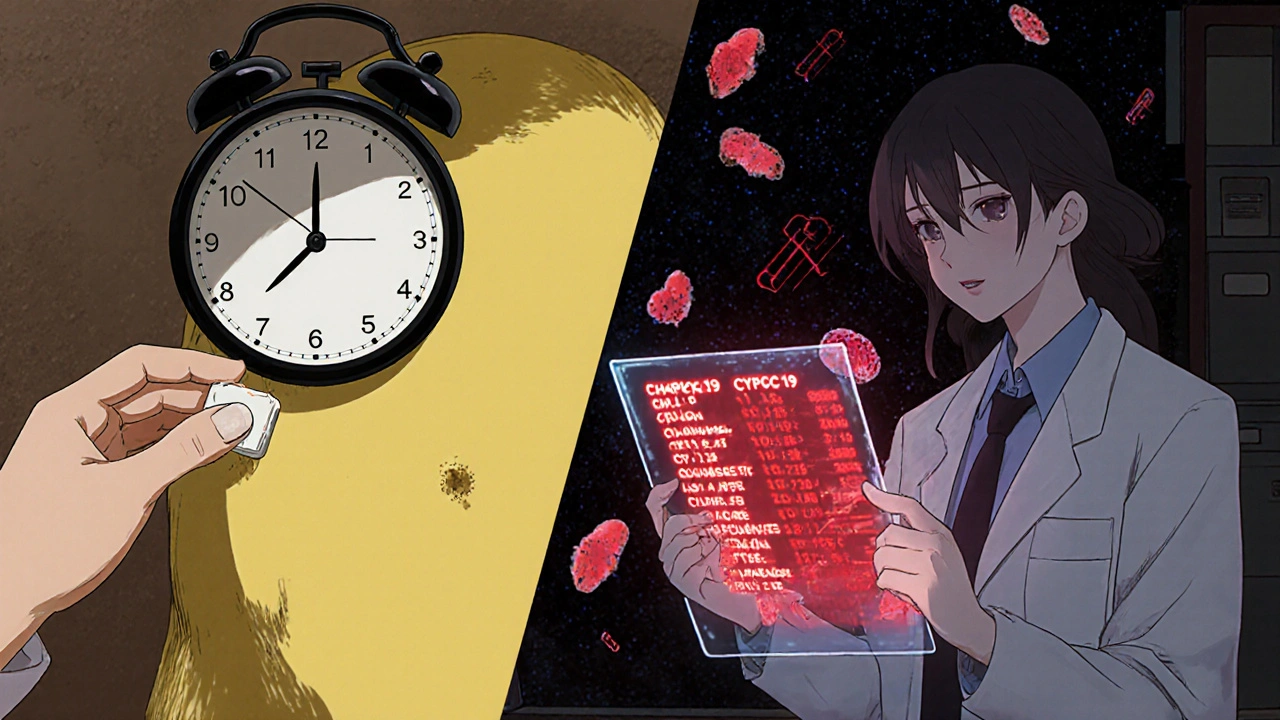
Antifungals don’t attack the liver on purpose. The damage happens because of how your body processes them. Most are broken down by liver enzymes-especially the CYP450 family. When these enzymes get overloaded or blocked, toxic byproducts build up. That’s what injures liver cells.For example, voriconazole is metabolized by CYP2C19. If you have a genetic variation that makes this enzyme work too slowly, the drug sticks around longer and builds up to dangerous levels. A 2022 study found people with this genetic quirk are 3.7 times more likely to get liver damage from voriconazole. That’s why some hospitals now test for this gene before prescribing.
Ketoconazole is even worse because it doesn’t just get broken down by the liver-it shuts down key liver enzymes. That means it interferes with how other drugs are processed. If you’re on blood thinners, statins, or certain antidepressants, ketoconazole can cause those drugs to pile up in your system. That’s a recipe for disaster.
Terbinafine works differently. It doesn’t interfere much with liver enzymes, but it can still cause direct toxicity to liver cells. That’s why liver injury from terbinafine often shows up suddenly, with no warning signs-until your ALT levels are through the roof.
Drug Interactions: The Silent Killer
One of the biggest dangers isn’t the antifungal alone-it’s what you’re taking with it.Ketoconazole is the worst offender. It’s a strong inhibitor of CYP3A4, the enzyme that breaks down over 50% of all prescription drugs. Taking it with statins like simvastatin can cause muscle breakdown. With blood thinners like warfarin, it can spike your INR and lead to dangerous bleeding. Even common heartburn meds like omeprazole can become toxic when mixed with ketoconazole.
Voriconazole plays the same game. It interacts with many HIV meds, cancer drugs, and even some seizure medications. A patient on voriconazole and tacrolimus (a transplant drug) can end up with kidney failure because the levels of tacrolimus skyrocket.
Even fluconazole, the “mild” one, can interfere with blood thinners, diabetes drugs, and certain antidepressants. The problem? Many patients don’t tell their doctors they’re taking over-the-counter supplements. St. John’s Wort, for example, can make voriconazole less effective. Garlic pills can thin the blood even more when combined with antifungals.
Doctors often miss these interactions because they’re focused on the infection, not the cocktail of meds. But a 2020 study found that nearly 40% of patients on long-term antifungals were taking at least one interacting drug-and half of them had no liver monitoring at all.
Who’s at Highest Risk?
Not everyone who takes an antifungal will have liver problems. But some people are sitting ducks.Elderly patients (65+) are at nearly 8 times higher risk of liver injury than younger adults. Their livers don’t process drugs as well, and they’re more likely to be on multiple meds.
People with pre-existing liver disease-even mild fatty liver or hepatitis C-should avoid ketoconazole and use other antifungals with extreme caution. A 2021 study showed that patients with liver cirrhosis had a 60% higher chance of liver failure when given any systemic antifungal.
Those on long-term therapy are also at risk. Nail fungus treatment with terbinafine can last 3 to 6 months. That’s long enough for liver damage to sneak up. One Reddit user reported jaundice and fatigue at week 5 of terbinafine-symptoms they ignored until their skin turned yellow.
People taking multiple hepatotoxic drugs-like acetaminophen, certain antibiotics, or alcohol-should avoid antifungals unless absolutely necessary. The combined effect can be deadly.
What Should You Do? Monitoring and Safety Steps
The good news? Liver damage from antifungals is often preventable-if you’re watched closely.Baseline liver tests are non-negotiable. Before starting any systemic antifungal, you need a blood test for ALT, AST, bilirubin, and alkaline phosphatase. If these are already high, your doctor should reconsider the drug.
Regular monitoring is key:
- Ketoconazole, itraconazole, voriconazole: Weekly liver tests for the first month, then every 2 weeks.
- Fluconazole: Only if you’re on it longer than 2 weeks or have liver issues.
- Terbinafine: Check at 4 to 6 weeks, then every 4 to 8 weeks if treatment continues.
Know the warning signs: Fatigue, nausea, loss of appetite, dark urine, jaundice (yellow skin or eyes), and pain under your right ribs aren’t just “off days.” They could be your liver screaming for help.
Stop the drug immediately if your ALT or AST rises above 3 times the normal level and you have symptoms-or above 5 times normal, even without symptoms. Don’t wait for your next appointment. Call your doctor now.
Don’t self-treat. Over-the-counter antifungals for nail fungus (like terbinafine tablets) are available in many countries. But they’re not harmless. A 2020 study found only 37% of primary care doctors ordered liver tests before prescribing them. Don’t assume your pharmacist knows your full med list. Tell them everything.
What’s Changing in the Future?
The tide is turning. Doctors are moving away from ketoconazole entirely. Newer antifungals like isavuconazole and ibrexafungerp are being designed with liver safety as a top priority. Early trials show they cause 78% fewer liver enzyme spikes than older azoles.Genetic testing is becoming more common. If you’re being prescribed voriconazole, your doctor might soon check your CYP2C19 gene before writing the script. That’s precision medicine in action.
The FDA’s Sentinel Initiative now tracks antifungal liver injury in real time using millions of electronic health records. That means dangerous patterns are spotted faster-and warnings come out quicker.
But here’s the reality: no drug is perfectly safe. The goal isn’t to avoid antifungals altogether-it’s to use them wisely. For life-threatening infections, the risk of not treating is far greater than the risk of liver damage. But for mild nail fungus? There are safer options. Topical treatments, laser therapy, or even waiting it out might be better than risking your liver.
Final Takeaway: Know Your Meds, Know Your Body
Antifungals save lives. But they can also harm them-if you’re not paying attention. The key is awareness. Know which drug you’re taking. Ask your doctor: “Is this the safest option for my liver?” and “What drugs or supplements should I avoid?” Get your blood tested before and during treatment. Don’t ignore fatigue or nausea. And never, ever take ketoconazole unless your doctor has ruled out every other option.Your liver doesn’t complain until it’s too late. Be the one who speaks up for it.
Can antifungals cause permanent liver damage?
Yes, in rare cases. While most liver injuries from antifungals reverse after stopping the drug, some patients develop acute liver failure requiring transplant. Ketoconazole and terbinafine have been linked to irreversible damage in a small number of cases. Early detection and stopping the drug quickly greatly reduce this risk.
Is fluconazole safe for the liver?
Fluconazole is the safest oral azole for the liver, but it’s not risk-free. It’s generally safe for short-term use (under 2 weeks). For longer courses, especially in people over 65, with existing liver disease, or on other liver-affecting drugs, monitoring is required. Cases of liver injury are rare but documented.
Why is ketoconazole banned in Europe but still available in the U.S.?
The European Medicines Agency banned oral ketoconazole in 2013 due to its high risk of liver failure and adrenal problems. The FDA didn’t ban it but severely restricted it to second-line use only-for rare fungal infections when no other antifungals work. It’s no longer approved for fungal nail infections, athlete’s foot, or dandruff. Most U.S. doctors avoid it entirely.
Should I get genetic testing before taking voriconazole?
It’s not standard yet, but it’s becoming more common in hospitals treating high-risk patients-like transplant or cancer patients. If you have a history of liver problems or are on other medications metabolized by CYP2C19, ask your doctor about testing. A 2022 study showed people with certain gene variants are nearly 4 times more likely to develop liver damage from voriconazole.
Can I drink alcohol while taking antifungals?
No. Alcohol stresses the liver and can worsen antifungal-induced liver injury. This is especially dangerous with ketoconazole, itraconazole, and voriconazole. Even moderate drinking can push your liver over the edge. Avoid alcohol entirely while taking any systemic antifungal-and for at least a week after stopping.
What are the alternatives to oral antifungals for nail fungus?
Topical antifungals like efinaconazole or tavaborole are much safer for the liver-they don’t enter the bloodstream in significant amounts. Laser therapy and nail removal are other options. For mild cases, some people choose to wait and monitor, since nail fungus isn’t life-threatening. Always discuss alternatives with your doctor before starting oral meds.
If you’re currently on an antifungal and haven’t had liver tests, schedule them now. If you’ve had unexplained fatigue or jaundice while on these drugs, tell your doctor-even if it happened months ago. Your liver can’t speak, but your actions can save it.


Sullivan Lauer
Let me tell you, I was on terbinafine for nail fungus for six months. No one warned me about the liver risks. I started feeling like a zombie at week four-fatigue, nausea, the whole deal. I thought it was just stress. Turns out my ALT was through the roof. Got lucky-caught it early, stopped the drug, and my liver bounced back. But I’m telling you, if you’re taking these pills, get tested. Don’t wait until your skin turns yellow. Your liver doesn’t text back.
Steven Howell
As a clinical pharmacologist with over two decades of experience in hepatotoxic drug monitoring, I must emphasize that the risk stratification presented in this article is both accurate and clinically indispensable. The pharmacokinetic interplay between CYP450 inhibition and polypharmacy in elderly populations remains grossly underappreciated in primary care settings. I routinely recommend baseline and serial liver function tests for all patients prescribed systemic azoles, particularly those with concomitant statin or anticoagulant use. The data on ketoconazole’s hepatotoxicity profile is unequivocal, and its continued off-label use for dermatophytosis represents a dangerous deviation from evidence-based guidelines.
Robert Bashaw
Y’all are acting like antifungals are some kind of poison fairy dust. Look-I’ve been on voriconazole for aspergillosis since last year. My liver? Still ticking. My doctor checks my enzymes every week like clockwork. I don’t need a panic attack every time I swallow a pill. The real danger? Not taking the meds when you need them. I’ve seen people die because they were too scared of their own liver to fight the fungus. This isn’t a horror story-it’s a management protocol. Get your labs, don’t drink, don’t self-medicate, and stop acting like every pill is a death sentence.
stephen idiado
Pharmacovigilance data misinterpretation. Indication bias confounds mortality attribution. Echinocandins: low incidence, high case-fatality due to ICU comorbidities. Terbinafine: idiosyncratic hepatotoxicity, not dose-dependent. CYP2C19 PMs: 3.7x risk, yes-but only in pharmacogenomic-competent centers. Most global populations lack access. Hence, blanket monitoring protocols are impractical. Topical > oral for onychomycosis. End of discussion.
Subhash Singh
This is an exceptionally well-researched and clinically nuanced overview. I am a physician in India, and I can confirm that antifungal-induced hepatotoxicity is severely underreported in our healthcare system. Many patients self-medicate with terbinafine or fluconazole from local pharmacies without any baseline LFTs. The cultural reluctance to undergo blood tests-even for non-acute conditions-is alarming. I now routinely counsel patients using the analogy: ‘Your liver is your silent bodyguard. Don’t make it fight alone.’ Thank you for this.
Sohini Majumder
Okay but like… why is everyone so obsessed with liver damage?? I mean, yeah, it’s important, but like… have you seen how many people are on 17 different meds and still think they’re fine?? I took fluconazole for a yeast infection for 10 days and my liver is fine. I also drink wine. And eat pizza. And sleep 4 hours. So… maybe stop scaring people?? 😅
tushar makwana
Man, I really appreciate this post. My mom was on ketoconazole for a bad fungal infection and ended up in the hospital. We had no idea. She didn’t even know what ‘liver enzymes’ meant. After that, I started asking every doctor, ‘What’s this gonna do to her liver?’ Now I do the same for my friends. It’s not about being scared-it’s about being smart. Thanks for helping people like me speak up.
Richard Thomas
It is imperative to underscore the systemic inadequacies in pharmacological education among non-specialist practitioners. The prevalence of concurrent CYP3A4 substrate administration-such as simvastatin, cyclosporine, or even certain SSRIs-in patients prescribed azole antifungals remains alarmingly high, particularly in ambulatory care settings where electronic health record alerts are either absent or routinely overridden. Furthermore, the normalization of over-the-counter terbinafine use without mandatory baseline hepatic assessment constitutes a public health vulnerability that regulatory bodies have thus far failed to adequately address. A standardized, tiered monitoring algorithm, integrated into prescribing workflows, is not merely advisable-it is ethically obligatory.
Mary Kate Powers
You’re not alone if you’re scared. I was too. But knowledge is power. I got my bloodwork done before starting fluconazole, told my doctor about my alcohol habit, and we picked the safest option. Now I’m fungus-free and my liver is happy. You don’t have to be a doctor to protect yourself-just ask questions, get tested, and don’t feel dumb for caring. Your body is worth it.
Sara Shumaker
It’s funny how we fear the medicine more than the disease. We’ll take antibiotics for a sore throat without blinking, but the moment it’s an antifungal, we panic. Maybe it’s because fungi feel… more alien. But the real issue isn’t the drug-it’s how disconnected we are from our own bodies. We don’t listen to fatigue. We ignore nausea. We think ‘I feel fine’ means ‘I’m fine.’ But your liver doesn’t scream until it’s screaming for a transplant. This post is a wake-up call-not a scare tactic. Thank you.
Scott Collard
Fluconazole is safe. Period. If you’re over 65 and on statins, sure, monitor. But most people? Fine. Stop fearmongering. Also, your ‘black box’ warning for terbinafine? It’s for 0.01% of users. You’re treating a 1-in-10,000 risk like it’s a pandemic. Chill.
Peter Axelberg
I’m a 58-year-old mechanic. Took terbinafine for toenail fungus. Didn’t think twice. Six weeks in, I couldn’t get out of bed. Thought I had the flu. Went to the ER. Turned out my liver was fried. I didn’t know I was at risk. I don’t drink. I don’t take other meds. Just this one pill. Now I’m on the transplant list. Don’t be like me. Get tested. Even if you think you’re fine. Your liver doesn’t care if you’re ‘healthy.’
Matthew Higgins
Man, I read this and just thought… we’re so good at making meds that kill us. Like, we’ve got these crazy powerful antifungals, but we treat our bodies like they’re machines you can just plug and play. No maintenance. No checkups. Just swallow and hope. I’ve got a cousin who’s on voriconazole for aspergillosis. His doc checks his liver every week. That’s the difference between surviving and… not. If you’re on this stuff, be the person who asks the questions. Even if it feels weird.
Sullivan Lauer
Scott, I get where you’re coming from. Fluconazole *is* the safest. But ‘safe’ doesn’t mean ‘risk-free.’ I’ve seen two cases in my clinic alone where patients on fluconazole for 3 months developed acute hepatitis-no alcohol, no other meds. One needed a transplant. It’s rare, yes. But it happens. And if you’re the one it happens to? ‘Safe’ doesn’t matter anymore. That’s why monitoring isn’t fear-it’s responsibility.