Electrolyte Imbalances: Managing Potassium, Phosphate, and Magnesium
Why Electrolyte Imbalances Matter More Than You Think
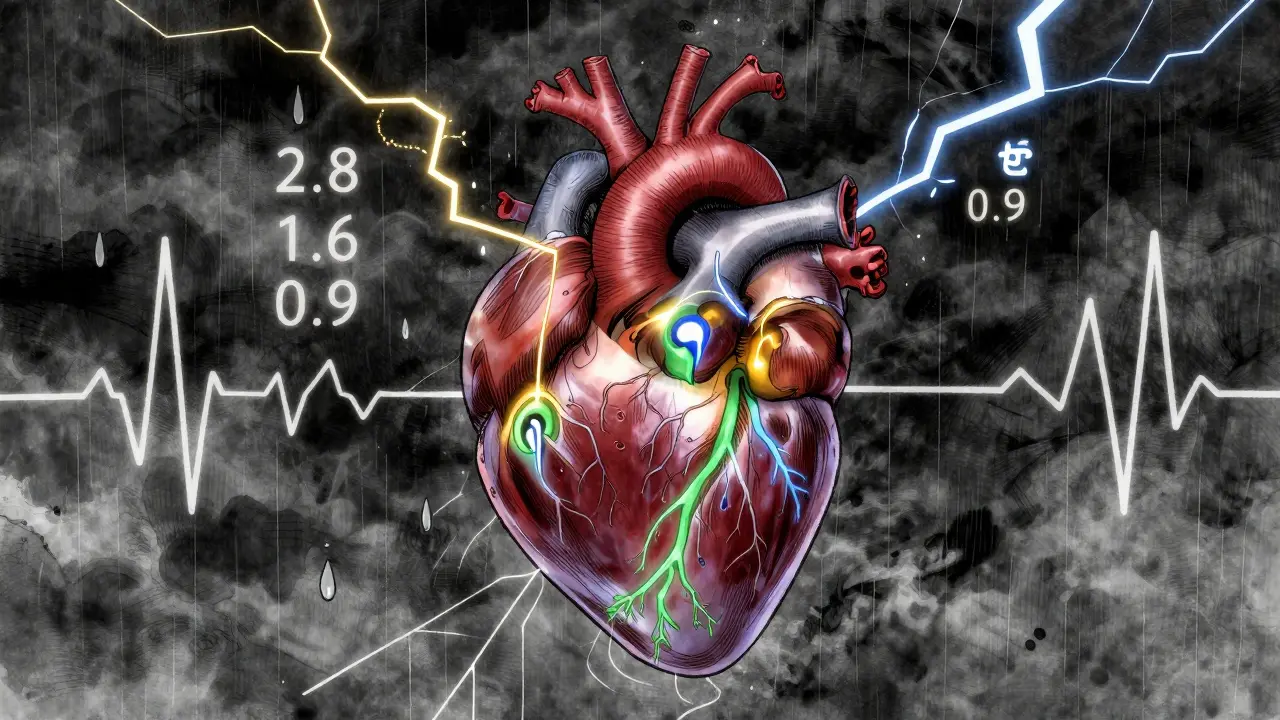
When your body runs low on potassium, phosphate, or magnesium, it doesn’t just feel tired-it can stop working properly. These three electrolytes are the quiet guardians of your heart rhythm, muscle strength, and nerve signals. In people with kidney problems, even small shifts can trigger dangerous arrhythmias, breathing failure, or sudden collapse. You won’t always feel it coming. That’s why checking levels isn’t optional-it’s lifesaving.
What Normal Levels Look Like (And When to Worry)
Normal ranges aren’t just numbers on a lab report. They’re the tightrope your body walks every day. For potassium, anything below 3.2 mEq/L or above 5.0 mEq/L is outside safe limits. Critical danger kicks in at under 3.0 or over 6.5. Magnesium should stay between 1.7 and 2.2 mg/dL. Below 1.0 mg/dL, your muscles twitch uncontrollably. Above 2.5, you risk paralysis. Phosphate sits between 2.5 and 4.5 mg/dL. Drop below 1.0, and your lungs can’t expand. Rise above 4.5, and calcium crashes, leading to bone pain and calcification.
These numbers aren’t abstract. A patient on diuretics for high blood pressure might wake up with a racing heart because their potassium dropped to 2.8. A diabetic in ketoacidosis could slip into respiratory failure because phosphate vanished overnight. In the hospital, these aren’t rare events-they’re daily emergencies.
The Hidden Link Between Magnesium and Potassium
Here’s the truth most people miss: you can give someone 100 mEq of potassium and still see no change in their blood level. Why? Because low magnesium is stealing it. Magnesium isn’t just another mineral-it’s the key that unlocks potassium’s entry into cells. Without enough magnesium, the kidneys keep dumping potassium, no matter how much you replace it.
Studies show that in patients with heart failure or those on digoxin, correcting low magnesium first cuts arrhythmia risk by over 60%. The American Heart Association’s 2023 guidelines now say this outright: check magnesium before you treat low potassium. If magnesium is under 1.8 mg/dL, give 4 grams of IV magnesium sulfate before touching potassium. Otherwise, you’re just wasting time-and risking a fatal rhythm.
How to Replace Potassium Safely
Oral potassium is fine for mild drops. But if levels are below 3.0 or the patient has chest pain or ECG changes, you need IV. The rule? Never rush it. Giving more than 10 mEq per hour through a peripheral line can burn veins or stop the heart. Even through a central line, don’t exceed 40 mEq/hour.
Each 20 mEq of IV potassium chloride raises serum potassium by about 0.25 mEq/L. That’s it. So if someone is at 2.9 and you want to get them to 3.5, you’re looking at roughly 40-50 mEq total, spread over 2-4 hours. After each dose, check potassium again at 1 hour, 2 hours, 4 hours, 6 hours, and 24 hours. Why? Because insulin, glucose, or even a single meal can shift potassium again.
For severe hyperkalemia (above 7 mEq/L with peaked T-waves or widened QRS), act fast: give 10 units of regular insulin with 50g of dextrose over 15 minutes to pull potassium into cells. Then give 10-20 mL of calcium gluconate to protect the heart. Finally, use a potassium binder like patiromer or sodium zirconium cyclosilicate-both approved by NICE in early 2023-to remove excess potassium from the gut. Dialysis is the last resort, but it’s life-saving when kidneys are failing.

Phosphate: The Silent Killer in ICU Patients
Phosphate doesn’t get much attention-until someone can’t breathe. In the ICU, hypophosphatemia is common. Why? Refeeding syndrome. Diabetic ketoacidosis. Long-term use of phosphate binders. And since 2020, the FDA has flagged ferric carboxymaltose, a common IV iron treatment, as a major cause.
When phosphate drops below 1.0 mg/dL, muscles weaken-including the diaphragm. Patients start gasping. Their oxygen levels crash. They need intubation. But replacing phosphate is tricky. Too fast, and you get rebound hyperphosphatemia, which locks up calcium and causes seizures or heart rhythm issues.
For mild cases (1.0-1.9 mg/dL), oral phosphate works: 8 mmol three times a day. For severe cases, use IV. The standard dose is 7.5 mmol of elemental phosphorus, infused slowly over 4-6 hours. Never push it. Monitor calcium every 4-6 hours during replacement. Watch for tingling, muscle cramps, or low blood pressure-signs calcium is dropping too.
Hypermagnesemia: Rare, But Deadly
Too much magnesium? That’s mostly seen in kidney failure patients on magnesium-containing laxatives or antacids. Or after magnesium sulfate for preeclampsia. Levels above 2.5 mg/dL cause drowsiness. At 4.0, reflexes vanish. At 5.0, breathing stops.
Treatment is simple but urgent. Give 10-20 mL of IV calcium gluconate 10% to reverse the muscle and nerve blockade. If kidneys are still working, give a loop diuretic like furosemide to flush out the excess. If not, dialysis is the only option. Don’t wait for symptoms to get worse. In renal patients, magnesium builds up quietly-and kills fast.
Who Needs Routine Screening?
You don’t need to check everyone. But you should check these groups weekly-or even daily:
- Patients on diuretics (especially loop diuretics like furosemide)
- People with chronic kidney disease (stages 3-5)
- Those taking ACE inhibitors, ARBs, or spironolactone
- Patients with heart failure on digoxin
- Anyone recently admitted to the ICU or recovering from major surgery
- People on long-term IV iron (ferric carboxymaltose)
- Those with eating disorders or alcohol use disorder
Since 2021, teaching hospitals that added automated electrolyte alerts to their EHR systems saw a 22.4% drop in electrolyte-related adverse events, according to JAMA Internal Medicine. That’s not luck-it’s protocol.
What’s New in 2025-2026?
Point-of-care testing is now standard in ERs. You can get potassium, sodium, and magnesium results in under 10 minutes-down from 90 minutes just five years ago. That’s 37 minutes faster on average, according to Annals of Emergency Medicine (2023).
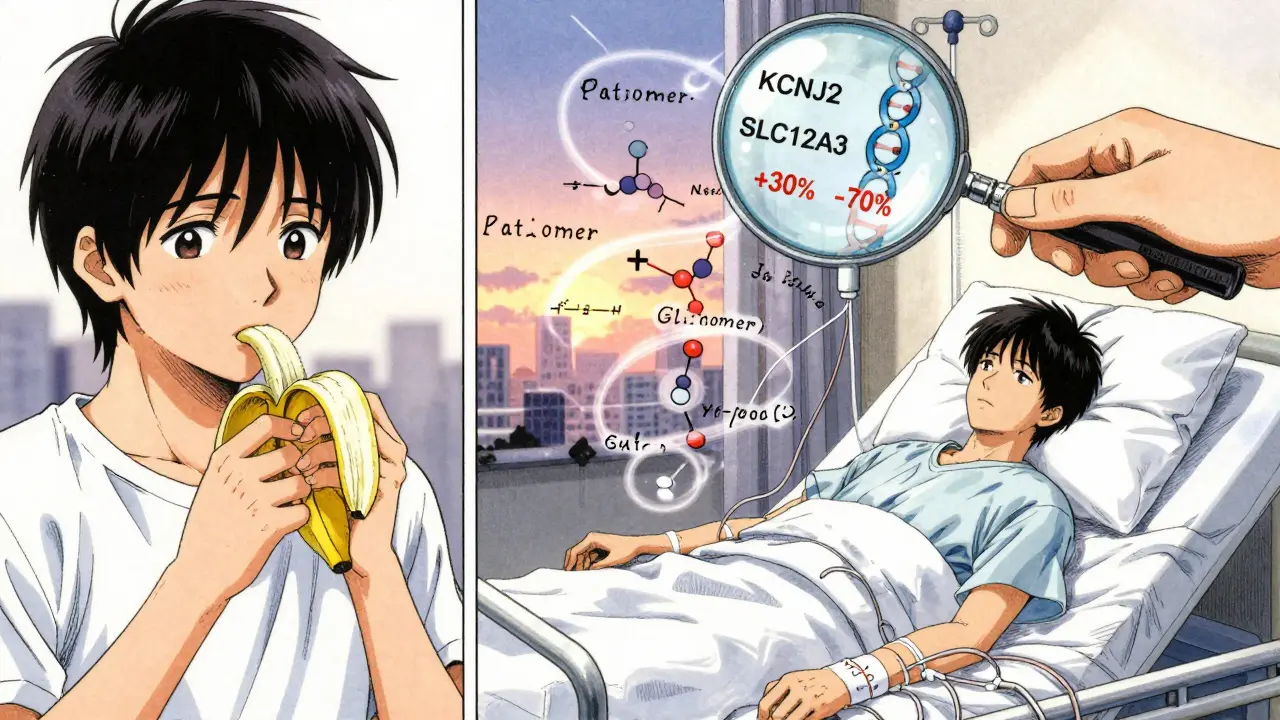
New phosphate binders like lanthanum carbonate and sevelamer are now designed to reduce hypophosphatemia risk in dialysis patients. And in late 2024, phase 3 trials for genotype-guided potassium replacement began. Early data shows people with certain gene variants need 30% less potassium to reach the same level. Personalized dosing is coming.
The biggest shift? Doctors are no longer treating electrolytes in isolation. It’s a system. Low potassium? Check magnesium. Low phosphate? Check vitamin D and calcium. High magnesium? Check kidney function and meds. It’s not just about the number-it’s about the story behind it.
Practical Takeaways for Daily Practice
- Always check magnesium before replacing potassium. If it’s low, treat it first.
- Never give IV potassium faster than 10 mEq/hour through a peripheral line.
- If someone’s phosphate is below 1.0, assume they’re at risk for respiratory failure-monitor closely.
- For hyperkalemia above 7 mEq/L with ECG changes: insulin + glucose, then calcium, then binder.
- For renal patients on IV iron, check phosphate monthly.
- Use potassium binders (patiromer, sodium zirconium cyclosilicate) instead of kayexalate-they’re safer and more effective.
These aren’t suggestions. They’re standards. And in renal patients, skipping one step can cost a life.
Can low potassium cause heart palpitations?
Yes. Low potassium (hypokalemia) disrupts the electrical signals in your heart, leading to extra beats, skipped beats, or dangerous rhythms like ventricular tachycardia. The risk spikes when low potassium happens with low magnesium-this combo is a known trigger for sudden cardiac arrest, especially in people with heart disease.
Why is magnesium checked before potassium in hospitals?
Because low magnesium causes the kidneys to keep throwing out potassium, no matter how much you give. If you replace potassium without fixing magnesium, the level won’t rise-or it’ll drop again fast. Studies show that correcting magnesium first makes potassium replacement work 70% more effectively.
Can eating bananas fix low potassium?
For mild cases, yes. One banana has about 420 mg of potassium, or 11 mEq. But if your level is below 3.0, or you’re on diuretics or have kidney disease, food alone won’t cut it. Oral supplements are needed. In emergencies, IV potassium is the only option.
What causes low phosphate in people with diabetes?
In diabetic ketoacidosis, insulin levels drop, and cells start burning fat for energy. This shifts phosphate into cells, draining it from the blood. When insulin is given to treat the ketoacidosis, it pushes even more phosphate inside cells-causing a sudden, dangerous drop. That’s why phosphate levels are checked hourly in these patients.
Is IV magnesium dangerous?
It’s safe when given correctly. The standard dose is 4 grams mixed in 100 mL of fluid, infused at 1 gram per minute. Too fast, and you can get low blood pressure, flushing, or even cardiac arrest. Always monitor blood pressure and reflexes during infusion. In kidney failure, avoid magnesium unless absolutely necessary.
Can electrolyte imbalances be prevented?
Absolutely. Regular blood tests for people on diuretics, kidney disease, or heart meds catch problems early. Avoid overuse of laxatives or antacids with magnesium. Monitor phosphate if you’re on IV iron. Use potassium binders instead of old-school resins. Simple steps, done consistently, prevent 90% of serious cases.
Next Steps: What to Do If You’re at Risk
If you have kidney disease, take a diuretic, or have heart failure, ask your doctor for a basic metabolic panel every 3 months. If you’re in the hospital, insist on a magnesium check before any potassium is given. If you’re on IV iron, get your phosphate checked before and after each dose.
Keep a list of your meds. Many common drugs-like ACE inhibitors, NSAIDs, and certain antibiotics-mess with electrolytes. Bring it to every appointment. Don’t assume your doctor knows. Most don’t.
Electrolyte imbalances aren’t mysterious. They’re predictable. And with the right checks, they’re preventable. The difference between life and death isn’t always a fancy treatment. Sometimes, it’s just asking the right question before it’s too late.


Simran Kaur
I saw a patient in Delhi last month-72, on furosemide for years, woke up with palpitations, potassium at 2.6. Magnesium? 1.3. Gave her 4g IV magnesium first. Then 40 mEq potassium over 3 hours. She sat up and asked for chai by noon. This isn’t just medicine-it’s respect for the body’s quiet systems.
People think bananas fix everything. No. It’s the *story* behind the number. And we’re not telling the story right.
Jessica Knuteson
Potassium is just a number. Magnesium is the real boss. The system doesn’t care about your lab values. It cares about gradients. Electrons. Membranes. You’re treating symptoms. The body’s just screaming in biochemistry.
rasna saha
As a nurse in Mumbai, I’ve seen this too many times. A patient gets potassium IV, no change. We check magnesium-low. Give it. Boom. Potassium climbs. It’s like trying to fill a bucket with holes. No one talks about the holes.
Just please-check magnesium first. Always. Even if the patient looks fine. They’re not always fine.
Skye Kooyman
I used to think phosphate was just for bones. Then I saw a guy on IV iron crash in the ER. No breathing. Phosphate 0.8. We gave 7.5 mmol slow IV. He woke up 3 hours later. Mind blown.
James Nicoll
So we’re giving IV magnesium now because… the AHA said so? Cool. Next they’ll tell us to kiss our pets before giving insulin. Look, if you’re giving potassium without checking magnesium, you’re not a doctor-you’re a guy with a syringe and a prayer.
Also, who the hell still uses kayexalate? That’s like using a horse and buggy to get to the moon.
Uche Okoro
The pathophysiological cascade is non-linear and context-dependent. Hypokalemia secondary to diuretic-induced volume depletion induces compensatory aldosterone secretion, which potentiates renal potassium excretion and magnesium wasting via TRPM6 downregulation. Concurrently, insulin-mediated transcellular shift in DKA exacerbates hypophosphatemia through GLUT4-mediated phosphate internalization. The clinical imperative is not merely supplementation but systems-level correction.
Failure to recognize this multivariate interdependency constitutes iatrogenic negligence.
Ashley Porter
Point-of-care magnesium testing in the ER? Game changer. We used to wait 2 hours for labs. Now we get a result in 8 minutes. Saved two code blues last month alone. No more guessing.
Peter Sharplin
I’ve been in this game 22 years. I used to think potassium was the star. Then I saw a guy on digoxin go into VT because his magnesium was 1.1. We gave 4g IV mag. He stabilized in 10 minutes. Potassium? Still low. But the rhythm? Gone.
Here’s the truth: magnesium isn’t a supplement. It’s the key. And if you’re not checking it before potassium, you’re not just behind the curve-you’re on the wrong track.
Also, if you’re giving IV potassium faster than 10 mEq/hour through a peripheral line, you’re playing Russian roulette with a 9mm. Stop it.
And for the love of God, stop using kayexalate. Patiromer is cheaper, safer, and doesn’t turn the colon into a cement mixer.
John Wippler
This post? It’s not just a guide. It’s a manifesto.
Electrolytes aren’t numbers on a screen. They’re the silent symphony of life. One note out of tune? The whole thing collapses.
I’ve watched people die because someone checked potassium and forgot magnesium. I’ve watched others live because a nurse asked, ‘What’s their mag?’
Don’t treat labs. Treat people. And if you’re not asking the right questions before the crisis hits-you’re not healing. You’re just hoping.
So check the mag. Slow the drip. Watch the calcium. Read the story. The body’s always whispering. Are you listening?
Kipper Pickens
2025 genotype-guided potassium dosing? Fascinating. But let’s not get ahead of ourselves. We still have hospitals where the EHR doesn’t alert for magnesium < 1.8. We’re talking about precision medicine while the basics are still broken.
Also-ferric carboxymaltose causing hypophosphatemia? That’s not new. It’s just now getting labeled. Pharma’s been doing this since 2012. We just didn’t look.
Aurelie L.
I work in the ER. We had a 68-year-old woman crash last week. Potassium 2.4. Magnesium 1.2. We gave potassium. No change. Then mag. She woke up. Don’t be that guy.
Sally Dalton
OMG this is SO important!! I’m a med student and I just learned this last week and I’m like WHY ISN’T THIS TAUGHT IN FIRST YEAR??
My grandma was on diuretics and they kept giving her potassium pills and she kept feeling awful. If they’d checked her mag…
pls everyone just check the mag first!! I’m crying typing this 😭
Betty Bomber
I work in a rural clinic. We don’t have fancy binders. But we do have bananas, oral KCl, and a fridge with magnesium sulfate. We do what we can. This post? Saved my last patient.
Mohammed Rizvi
They say potassium is the heart’s best friend. But magnesium? That’s the body’s therapist. You give potassium without magnesium? You’re yelling at someone who’s been silenced for years. They’re not listening. You gotta fix the silence first.