Food Intolerance vs. Allergy: GI Symptoms and Testing Explained
When your stomach churns after eating dairy, or you break out in hives after peanuts, it’s easy to assume it’s all the same thing: food allergy. But here’s the truth-what feels like an allergic reaction might just be your gut struggling to digest something. The difference between a food intolerance and a food allergy isn’t just semantics. It’s life-or-death. And getting it wrong can lead to unnecessary fear, dangerous restrictions, or worse-missing a real threat.
What’s Really Happening in Your Body?
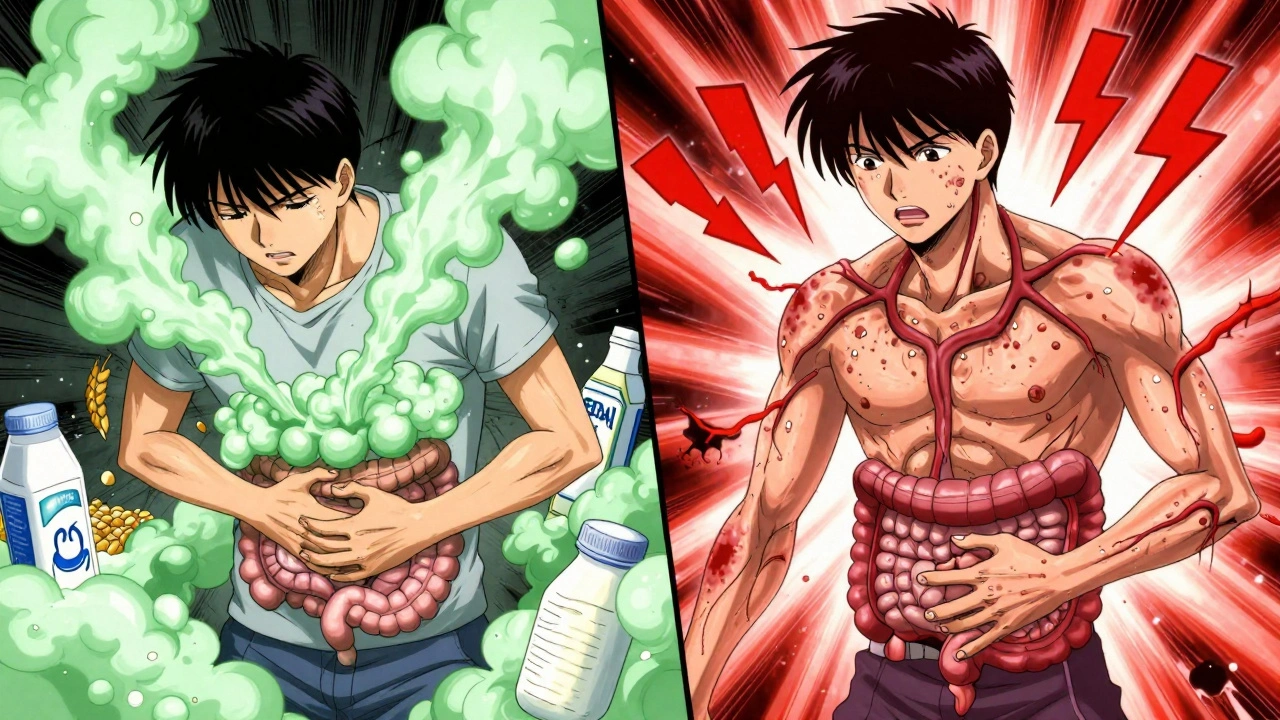
A food allergy is your immune system going into overdrive. It sees a harmless food protein-like peanut or milk-as an invader. It fires up IgE antibodies, which trigger mast cells to dump histamine and other chemicals into your bloodstream. That’s why symptoms can hit fast: within minutes, sometimes seconds. You might get hives, swelling, trouble breathing, or vomiting. In severe cases, it can trigger anaphylaxis-a full-body reaction that shuts down airways and drops blood pressure. It’s not just uncomfortable. It’s life-threatening. Food intolerance is different. No immune system involvement. No IgE antibodies. Just your digestive system saying, “I can’t handle this.” Most often, it’s because you’re missing an enzyme. Lactose intolerance? You don’t make enough lactase to break down milk sugar. The undigested lactose ferments in your colon, producing gas, bloating, cramps, and diarrhea. It usually shows up 30 minutes to two hours after eating. It’s messy. It’s annoying. But it won’t kill you.GI Symptoms: How to Tell Them Apart
Both can cause belly pain and diarrhea. But the pattern tells the story. With a food allergy, GI symptoms are part of a bigger picture. Vomiting or diarrhea? Likely. But you’ll also see:- Hives or skin flushing
- Swelling of lips, tongue, or throat
- Coughing, wheezing, or difficulty breathing
- Dizziness or fainting
- Bloating after milk or beans
- Gas and cramping after wheat or onions
- Diarrhea after artificial sweeteners or high-FODMAP foods
- Nausea without vomiting
Testing: What Works and What’s a Scam
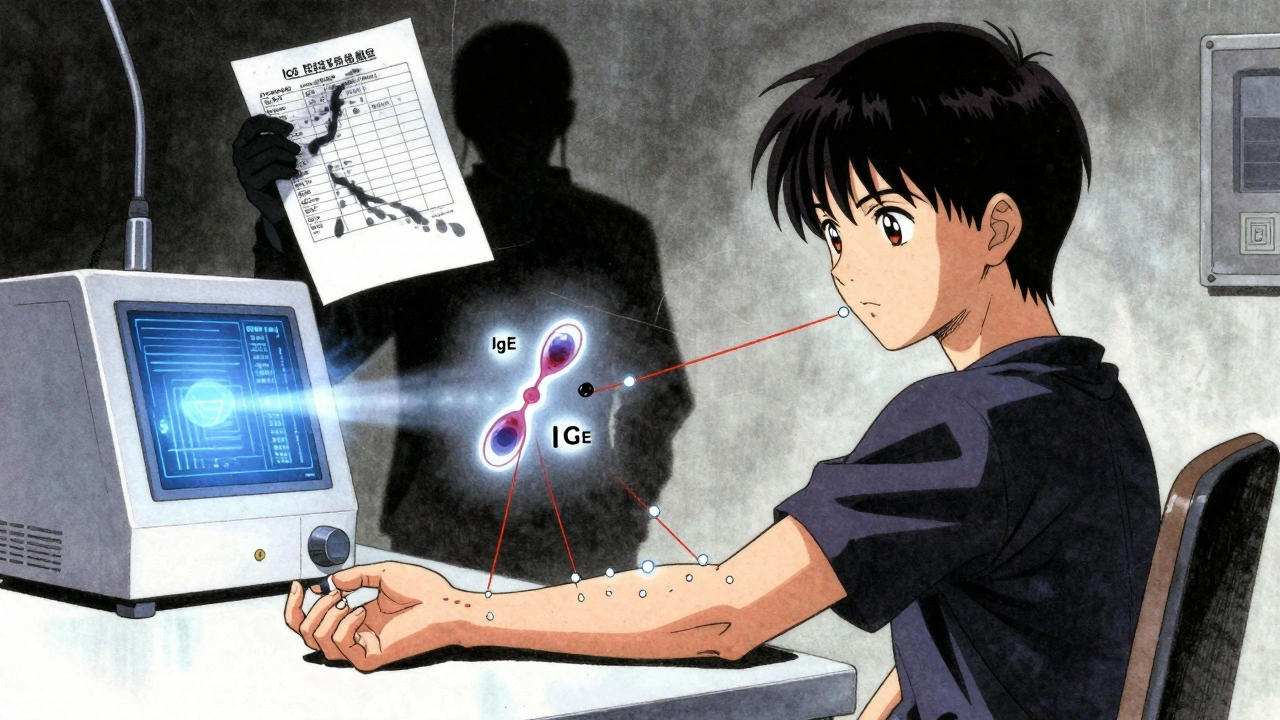
If you think you have a food allergy, see an allergist. Don’t guess. Don’t rely on online tests. The gold standard for diagnosing IgE-mediated allergies is a combination of:- Skin prick test: A tiny drop of allergen is placed on your skin, then lightly pricked. A raised, red bump (wheal) larger than 3mm compared to a control suggests allergy.
- Specific IgE blood test: Measures antibody levels in your blood. A result above 0.35 kU/L is considered positive, but context matters-some people test positive but never react.
- Oral food challenge: Done under medical supervision. You eat increasing amounts of the suspected food while being watched. This is the only test that confirms if you truly react. It’s the final word.
- Lactose intolerance: Diagnosed with a hydrogen breath test. You drink a lactose solution, and your breath is tested every 15-30 minutes. A rise of 20 ppm above baseline confirms malabsorption.
- Celiac disease: Requires a blood test for tissue transglutaminase IgA antibodies. If it’s above 10 U/mL, you’ll need an endoscopy with biopsy to confirm Marsh 3 damage.
- Non-celiac gluten sensitivity: No blood test exists. Diagnosis is made by ruling out celiac and wheat allergy, then doing a strict gluten-free trial for 2-6 weeks, followed by reintroduction. If symptoms return, it’s likely this condition.
Management: Avoidance vs. Moderation
If you have a food allergy, you must avoid it completely. Always. Even if past reactions were mild. The next one could be worse. You need to carry two epinephrine auto-injectors (like EpiPen) at all times. Prescription costs? Around $550-$750 without insurance. Insurance doesn’t always cover them fully. Read labels. The FDA requires the top 9 allergens to be clearly listed: milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame (added in 2023). But cross-contamination? That’s the hidden danger. A cookie baked in a facility that processes peanuts? Risky. A shared fryer? Deadly. Food intolerance? It’s about balance, not banishment.- Lactose-intolerant people? Most can handle up to 12 grams of lactose per day-that’s about one cup of milk. Hard cheeses and yogurt often cause fewer symptoms because they’re lower in lactose.
- Gluten-sensitive? You might tolerate small amounts of wheat or barley. No need to go 100% gluten-free unless you have celiac.
- Sulfite-sensitive? Avoid wine, dried fruit, and processed potatoes. But you don’t need to cut out all processed foods.
What Else Could Be Going On?
Too many people blame food when the real culprit is something else. A 2023 study found that 80% of people who think they have a food intolerance actually have another condition:- 45% had irritable bowel syndrome (IBS)
- 12% had inflammatory bowel disease (IBD)
- 23% had functional dyspepsia

When to See a Doctor
See a specialist if:- You have symptoms after eating the same food more than once
- Your symptoms are severe, frequent, or worsening
- You’ve had a reaction involving breathing, swelling, or dizziness
- You’re losing weight or having blood in your stool
- You’ve been on an elimination diet for weeks with no improvement


nithin Kuntumadugu
bro i took one of those IgG tests off amazon and it said i’m allergic to water 🤡 now i’m drinking distilled and praying to the gluten gods. also why is everyone so scared of soy? it’s just fermented bean juice. 🤷♂️
John Fred
Love this breakdown! 🙌 As a GI nurse, I see so many people self-diagnose with ‘gluten sensitivity’ when they actually have SIBO or bile acid malabsorption. Always rule out the big stuff first-endoscopy, H. pylori, thyroid panels. No magic bullet, just science. And yes, IgG tests are snake oil. 🐍
Lauren Scrima
So… you’re telling me the $300 ‘food sensitivity’ test from that wellness influencer who sells ‘detox tea’ is just… a marketing ploy? Shocking. 🤯
Harriet Wollaston
This is the kind of post I wish my doctor would write. I spent 3 years thinking I had a ‘mystery allergy’-turns out I just needed to stop chugging milk with my cereal. 😅 So glad someone finally explained the difference without jargon overload. Thank you.
Scott Butler
Of course the FDA says sesame is an allergen now. That’s just woke science. Back in my day, you just toughed it out. If your kid breaks out in hives from a peanut butter cracker, maybe he needs more discipline-not a $700 EpiPen.
Karen Mccullouch
THEY’RE HIDING THE TRUTH. IgE tests are controlled by Big Pharma. The real test is your gut feeling. I stopped eating ALL carbs after my third colonoscopy and now I’m 100% pain-free. Also, I think the moon is made of gluten. 🌕
Ronan Lansbury
Let’s be real-this entire post is just a thinly veiled advertisement for allergists charging $500/hour. Who even has access to oral food challenges? The poor? The uninsured? The ones who can’t afford to miss work for a 4-hour ‘taste test’? This isn’t medicine-it’s luxury diagnostics for the 1%. Meanwhile, my cousin in Dublin just drinks goat milk and calls it a day. She’s fine. Why do we need a lab report to live?
And don’t get me started on ‘component-resolved diagnostics.’ That’s just fancy language for ‘we’re charging you more to tell you the same thing.’
Every time someone says ‘trust science,’ they mean ‘trust the institution that profits from your fear.’
Why do we assume the body is broken instead of the system? Why do we pathologize digestion instead of questioning why our food is so damn processed in the first place?
I’m not saying ignore allergies. But when your entire medical-industrial complex is built on selling you tests for things you might not even have, it’s not science-it’s capitalism with a stethoscope.
And yes, I’ve read the papers. And no, I don’t trust them.
So I’ll keep my gut feelings, my herbal teas, and my skepticism. You keep your $750 EpiPens.
sharon soila
You’re right. We need to listen to our bodies. But we also need to listen to the experts who’ve spent decades studying this. One doesn’t cancel the other. Both matter. Be curious. Be kind. But don’t be reckless.