Kyphoplasty vs Vertebroplasty: What You Need to Know About Vertebral Fracture Treatment

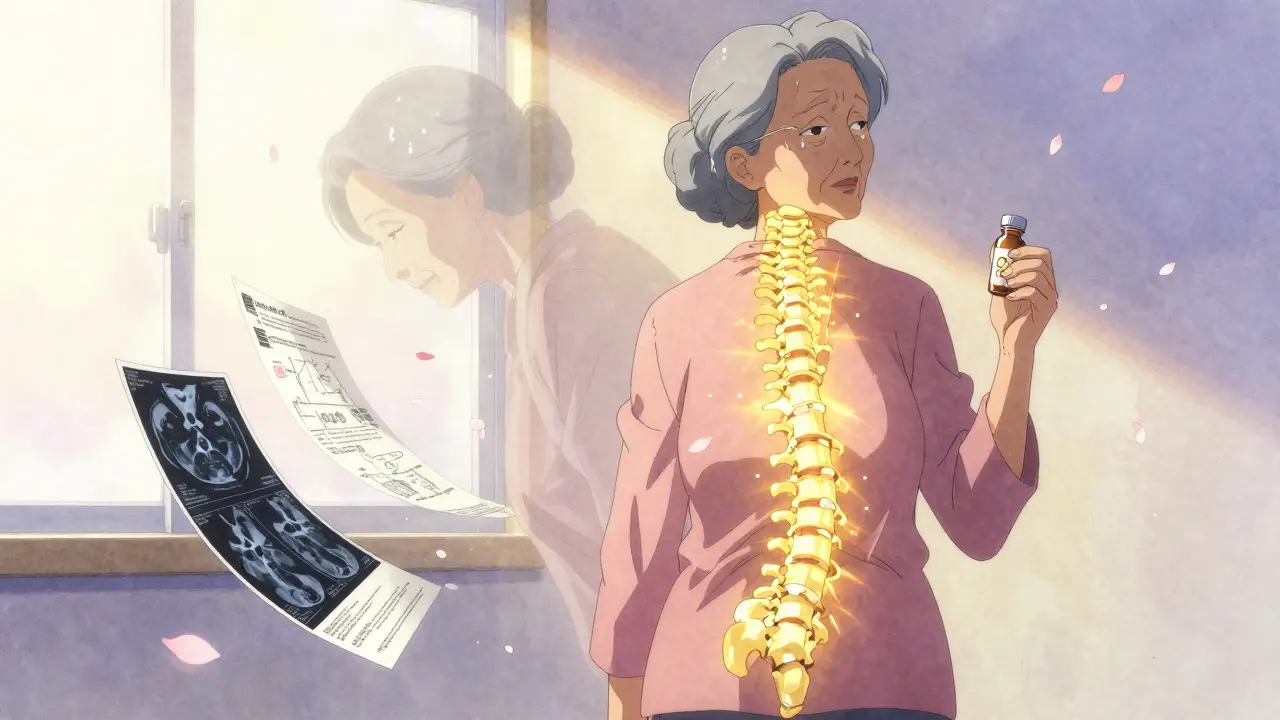
When a vertebra collapses due to osteoporosis, trauma, or cancer, the pain can be unbearable. Standing, sitting, even breathing becomes a struggle. For many, conservative treatments like rest, painkillers, or back braces don’t cut it. That’s where kyphoplasty and vertebroplasty come in - two minimally invasive procedures that can restore mobility and bring relief in hours, not weeks.
Both procedures fix broken spinal bones using medical-grade bone cement. But they’re not the same. One uses a balloon to lift the bone before filling it. The other injects cement directly. Knowing the difference matters - because your fracture, your body, and your goals determine which one is right for you.
How These Procedures Work
Imagine a bone in your spine that’s been crushed, like a soda can stepped on. It’s painful, unstable, and often misshapen. Kyphoplasty and vertebroplasty both aim to stabilize it, but they take different paths.
Vertebroplasty is the older method. A doctor inserts a thin needle through your skin and into the fractured vertebra, guided by real-time X-ray. Then, they inject liquid bone cement - polymethylmethacrylate, or PMMA - directly into the crack. The cement hardens in 10 to 20 minutes, locking the bone fragments together. It’s quick, usually taking 30 to 60 minutes per level. Most patients go home the same day.
Kyphoplasty adds a step. Before injecting cement, a small balloon is threaded into the fracture. It’s inflated gently with saline, lifting the collapsed bone back toward its original height. Once the balloon is deflated and removed, the space it created is filled with cement. This extra step doesn’t just stabilize - it can restore some of the spine’s natural curve.
Both procedures use local anesthesia and IV sedation. You’re awake but relaxed. No large incisions. No long hospital stays. Recovery starts immediately.
Key Differences: Height Restoration and Cement Leakage
The biggest difference between the two isn’t pain relief - both deliver it. It’s what happens inside the bone.
Kyphoplasty can restore 40% to 60% of lost vertebral height. That’s important if your spine has developed a noticeable hunch (kyphosis). Restoring height can improve posture, reduce pressure on other vertebrae, and even help with breathing. But here’s the catch: studies show that some of this height gain fades over time. After 500 loading cycles (roughly equivalent to months of normal activity), you might lose about 30% of the restored height. Still, even partial restoration can make a real difference in daily life.
Vertebroplasty doesn’t try to lift the bone. It just fills the space. So if your fracture is stable and not causing a visible curve, it works just as well for pain relief.
Then there’s cement leakage - a risk in both procedures. With vertebroplasty, cement can leak out of the bone into surrounding tissues. Studies show leakage happens in 27% to 68% of cases. Most leaks cause no symptoms. But in about 1.1% of cases, it presses on nerves or travels to the lungs, causing serious problems. Kyphoplasty reduces this risk. The balloon creates a controlled cavity, so cement is injected under lower pressure. Leakage drops to 9% to 33%. Symptomatic leaks are rare - just 0.6% of kyphoplasty cases.
How Much Pain Relief Can You Expect?
Here’s the good news: both procedures deliver fast, powerful pain relief.
Before the procedure, patients typically rate their pain at 8.2 out of 10. Within 24 hours, that number drops to 1.5 on average. That’s an 85% to 90% reduction. Most people say it feels like a switch was flipped.
Patients on Healthgrades rate kyphoplasty 4.6/5 and vertebroplasty 4.4/5. On forums, people describe it as "instant relief," "life-changing," or "I can finally sleep again."
But pain relief isn’t guaranteed for everyone. About 10% to 15% of patients still have discomfort afterward. Why? Maybe the fracture was too old. Maybe other spine issues are involved. Or maybe the cement didn’t spread evenly. That’s why MRI is required before either procedure - to confirm the fracture is still active, with inflammation in the bone marrow. If it’s an old, healed break, these procedures won’t help.

Cost, Recovery, and Who Pays
Kyphoplasty costs 20% to 30% more than vertebroplasty. In 2023, Medicare paid about $3,850 for kyphoplasty and $2,950 for vertebroplasty. That’s because of the balloon device - a single-use, specialized tool that adds to the price.
But cost isn’t just about the procedure. Recovery matters too. Most patients walk the same day. They’re off painkillers within a week. Studies show 75% stop using opioids after the procedure. Normal activities return within 1 to 2 weeks.
Medicare and most private insurers cover both procedures - if you’ve tried conservative treatment first. That means at least 4 to 6 weeks of rest, physical therapy, and pain medication without improvement. Approval rates are over 95% when paperwork is complete.
Who Gets Which Procedure?
Doctors don’t pick one over the other based on preference. They pick based on your fracture.
If your fracture has caused a visible hunch in your spine - more than 30% height loss - kyphoplasty is usually preferred. The balloon gives you a shot at correcting the deformity. It’s also better for patients with weak, crumbly bone, because the cavity reduces cement leakage risk.
If your fracture is stable, with little to no height loss, vertebroplasty is often the better choice. It’s cheaper, faster, and just as effective for pain relief. Experts like Dr. Richard Jensen argue that for these cases, the extra cost of kyphoplasty doesn’t justify the outcome.
Age matters too. Over 85% of these procedures are done on people 65 and older. Women make up 70% to 75% of cases - because osteoporosis hits them harder. But men with fractures from trauma or cancer benefit just as much.
What to Expect Before and After
You’ll need an MRI within the last 6 weeks to confirm the fracture is active. X-rays and CT scans help too, but MRI shows the bone marrow inflammation that tells doctors this is a fresh injury.
On the day of the procedure, you’ll lie face down. A needle goes in, guided by live X-ray. The whole thing takes less than an hour. You’ll be monitored for 4 to 6 hours afterward. You can’t drive home, so bring someone.
For the first 24 hours, avoid lifting anything heavier than a coffee cup. No twisting. No bending. After that, you can gradually increase activity. Most people are back to light chores by day three. Full recovery takes 1 to 2 weeks.
Some patients develop new fractures nearby within a year. That happens in 5% to 10% of cases. It’s not because the procedure caused it - it’s because osteoporosis is still there. That’s why long-term management matters: calcium, vitamin D, and bone-strengthening meds like bisphosphonates.
The Future of Spinal Fracture Care
Newer cement types are coming. Calcium phosphate cements mimic natural bone better and generate less heat during hardening, reducing tissue damage. Medtronic’s updated balloon system got FDA approval in March 2023.
A major 2023 study in The Lancet found that doing either procedure within two weeks of the fracture cut 12-month death risk by 28%. That’s huge. It suggests these aren’t just pain fixes - they might save lives by getting people moving again.
Right now, kyphoplasty makes up about 65% of procedures in the U.S. But analysts predict that will rise to 75% by 2028. Why? Better safety, more devices, and growing awareness.
Still, the bottom line hasn’t changed: if you have a painful, fresh vertebral fracture, both procedures work. The choice isn’t about which is "better." It’s about which fits your fracture, your body, and your life.



Alex Ogle
Man, I remember when my grandpa had one of these procedures. He was 82, osteoporosis had turned his spine into a question mark. We thought he’d be stuck in that chair forever. Kyphoplasty didn’t fix everything, but it gave him back the ability to stand up straight enough to see the TV without tilting his head. I swear, the day after, he made coffee and didn’t wince. That’s the kind of thing you don’t forget. Not magic, but close enough.
Still, I’ve seen people rush into it without realizing their fracture was old. MRI’s not optional. If the bone marrow’s not glowing red on the scan, you’re just pouring cement into a tomb. No point.
And yeah, the cost difference? Real. But when you’re paying out of pocket, that $900 gap can mean skipping a month of physical therapy. Insurance fights are real. I’ve been in those phone queues.
Most people don’t realize how much of this is about mobility, not just pain. It’s not about feeling better for a week - it’s about not becoming a ghost in your own house.
Brandon Osborne
These procedures are a scam. Big Pharma and spine device companies are pushing this because they make billions. The real problem? Osteoporosis. You don’t fix that with cement. You fix it with lifestyle, nutrition, and real medicine - not some glorified glue job. And don’t get me started on how they’re pushing this on elderly women like it’s a miracle cure. It’s not. It’s a Band-Aid on a broken foundation.
And don’t tell me about the 85% pain reduction - that’s just placebo with a needle. People feel better because they *think* they’re fixed. Then they fall again. And again. And the cycle continues. This isn’t treatment. It’s a revenue stream disguised as compassion.
Marie Fontaine
OMG I JUST HAD KYPHOPLASTY LAST MONTH AND IT WAS A GAME CHANGER 😭 I could barely walk before and now I’m dancing with my grandkids 🎉 no more pain meds! 10/10 would do again 💖
Ken Cooper
so i got vertebroplasty like 3 years ago and honestly? it was fine. no balloon, no fancy stuff. just a needle and some cement. i was in and out in 45 mins. pain went from 8/10 to 2/10 the next day. no drama.
but here’s the thing - i had a *stable* fracture. no hunch, no deformity. so kyphoplasty? overkill. my doc was like ‘why spend extra if you’re not losing height?’ and he was right.
also, i’m not gonna lie - the post-op instructions were wild. no bending. no lifting. not even picking up my cat. i missed my cat. but yeah, worth it. still feel good today. just don’t overhype it. it’s not a miracle. it’s a fix. and sometimes, simple is better.
MANI V
How can you even consider these procedures in a society that has abandoned the elderly? You don’t fix broken bones with cement - you fix broken systems. Why are we letting seniors fall through cracks in healthcare? Why are we allowing osteoporosis to become an epidemic because no one cares about calcium intake or weight-bearing exercise in old age? This is not medicine. This is damage control for a civilization that refuses to care until it’s too late.
And don’t get me started on how the U.S. charges double what other countries do for the same device. This isn’t innovation - it’s exploitation. You think your insurance covers this? It doesn’t. It just delays the inevitable. You’re paying for a temporary fix while the system ignores the root. Shameful.
Random Guy
So let me get this straight - you’re telling me we invented a balloon to inflate a broken bone like it’s a birthday party favor? And then we pour cement into it like it’s a cake mold? And people call this ‘medicine’?
Next they’ll invent a vacuum cleaner for the spine. ‘Hey doc, my vertebrae are sagging - can you just suck them back up?’
At this point, I’m just waiting for the AI surgeon to whisper ‘I’ve calculated your optimal cement-to-awkwardness ratio.’
Ryan Vargas
There’s an ontological paradox here. We treat the symptom - the collapsed vertebra - as if it were the disease. But the disease is osteoporosis. A systemic failure of bone remodeling. To inject cement into a collapsing structure is to engage in a form of temporal denial. We are not healing; we are delaying collapse with synthetic scaffolding.
Moreover, the very notion of ‘height restoration’ is a Cartesian illusion. The spine is not a column in a building. It is a dynamic, adaptive structure. To artificially reestablish a geometric ideal is to impose a mechanical norm upon a biological system. The 30% height loss over time? That’s not failure. That’s nature reasserting itself.
And yet - we persist. Because to admit that this is palliative, not curative, is to confront the uncomfortable truth: we have no cure. Only bandages. And we are afraid of the dark.
Tasha Lake
As a physiatrist, I see this every week. The key is fracture acuity. If the T2 MRI shows bone marrow edema - that’s your window. 2 weeks max. After that, the cement won’t integrate well, and you’re just stabilizing a scar.
Also - cement leakage isn’t just a technical risk. It’s about rheology. Vertebral pressure gradients, viscosity of PMMA, injection rate - all matter. Kyphoplasty’s balloon creates a low-pressure cavity, so you get better distribution. Less extravasation. That’s why the symptomatic leak rate drops so hard.
And yes, cost is a factor. But if you’re doing 3 levels? Kyphoplasty’s 20% higher cost? That’s offset by 40% lower reoperation rate. Insurance knows this. That’s why they’re shifting reimbursement.
Don’t forget: these aren’t cosmetic. They’re functional. One patient I had went from wheelchair to walking the dog in 72 hours. That’s not anecdote. That’s data.
Sam Dickison
Just wanted to say - I had vertebroplasty last year after a fall. Didn’t even know I had osteoporosis until the MRI. Doc said ‘you’re lucky this didn’t crush your spinal cord.’
Woke up the next day and thought ‘wait… I can breathe?’
Went back to gardening in 10 days. No opioids. No brace. Just… better.
But yeah - if you’re over 65, get a DEXA scan. Seriously. Don’t wait until you’re stuck on the floor. Prevention beats cement every time.
John McDonald
Love how this post breaks it down. I’m a physical therapist, and I’ve had patients come in after both procedures. The ones who got kyphoplasty? They had better posture changes early on. But honestly? After 6 months, the pain relief was nearly identical. The real difference was in mobility confidence - kyphoplasty patients felt less afraid to move.
Also - huge shoutout to the point about osteoporosis management post-procedure. Too many people think ‘fixed spine = fixed bones.’ Nope. You still need calcium, vitamin D, and maybe even a bisphosphonate. Otherwise, you’re just building a house on sand.
And yeah - if you’re under 70 and had trauma? Vertebroplasty’s fine. No need to overpay for a balloon if you’re not hunched.
Andy Cortez
Yeah right. ‘Kyphoplasty restores height.’ What a joke. The bone collapses again in months. So what’s the point? You’re just paying $900 extra to temporarily look less like a hunchback while your bones keep crumbling. And let’s not pretend the cement doesn’t weaken surrounding vertebrae. It’s like putting a steel rod in a rotten log - eventually, everything else gives.
And don’t even get me started on how the FDA approved these devices on 3-month trials. This isn’t medicine. It’s corporate wishful thinking wrapped in a catheter.
Andrew Jackson
This country has devolved into a spectacle of medical theater. We no longer treat disease - we perform procedures for the sake of procedure. The American healthcare system has turned spinal fractures into a profit center. The balloon? A gimmick. The cement? A commodity. The patient? A transaction.
Meanwhile, in nations with real healthcare, they use conservative management, physical therapy, and nutritional support. They don’t inject foreign polymers into fragile spines. They prevent collapse before it happens.
This is not progress. This is capitulation.
Joseph Charles Colin
Quick clarification for folks confused about cement leakage: it’s not the leakage itself that’s dangerous - it’s the *location*. Venous leakage into the paravertebral plexus? Usually harmless. Cement in the spinal canal? Emergency. Cement in the pulmonary artery? That’s a rare but real cause of acute respiratory failure.
Kyphoplasty reduces risk not because it’s ‘better’ - it’s because the balloon creates a contained space, so cement is injected under lower pressure. That’s biomechanics, not magic.
Also - calcium phosphate cements? They’re promising. Less exothermic reaction. Better osteoconductivity. But they’re still in trials. PMMA is still the gold standard. Don’t believe the hype.
Joshua Smith
I had both procedures - one level vertebroplasty, then 6 months later, another level got kyphoplasty. Why? Because my doc said the second fracture was more unstable and had more height loss. So yeah - it’s not one-size-fits-all.
Both worked. Both hurt a little for a day. Both had me walking the next day. The kyphoplasty side felt a bit more ‘lifted’ - like my posture actually changed. Not sure if it’s real or placebo, but I’ll take it.
Biggest takeaway? Get an MRI before you even think about it. If it’s not active, skip it. And if you’re scared? Talk to your physical therapist. They’ll tell you the truth - not the marketing.