Proton Pump Inhibitors and Clopidogrel: What You Need to Know About the Drug Interaction
PPI-Clopidogrel Interaction Checker
Check Your PPI Safety
Clopidogrel requires the CYP2C19 enzyme for activation. Some PPIs compete for this enzyme, potentially reducing clopidogrel's effectiveness. This tool helps identify which PPIs are safest to take with your antiplatelet medication.
Select a PPI above to see the interaction risk.
When you’re on clopidogrel to prevent blood clots after a heart attack or stent placement, your doctor might also prescribe a proton pump inhibitor (PPI) to protect your stomach. It seems like a simple combo: one drug keeps your blood from clotting too much, the other prevents dangerous ulcers. But here’s the catch - some PPIs can quietly weaken clopidogrel’s effect, raising your risk of another heart event. This isn’t theory. It’s been shown in clinical trials, FDA warnings, and real-world hospital data. And not all PPIs are created equal.
How Clopidogrel Actually Works
Clopidogrel isn’t active when you swallow it. It’s a pro-drug, meaning your liver has to turn it into something that works. That transformation relies heavily on one enzyme: CYP2C19. If this enzyme is blocked or slowed down, clopidogrel can’t become its active form. And that’s where PPIs come in.
Many PPIs - especially omeprazole and esomeprazole - are also broken down by CYP2C19. When you take them together, they compete for the same enzyme. Think of it like two people trying to use the same narrow hallway at the same time. One gets through slowly, or not at all. In this case, clopidogrel loses the race. Studies show omeprazole can cut the active metabolite of clopidogrel by up to 49% at high doses. That’s not a small drop - it’s enough to reduce antiplatelet effects significantly.
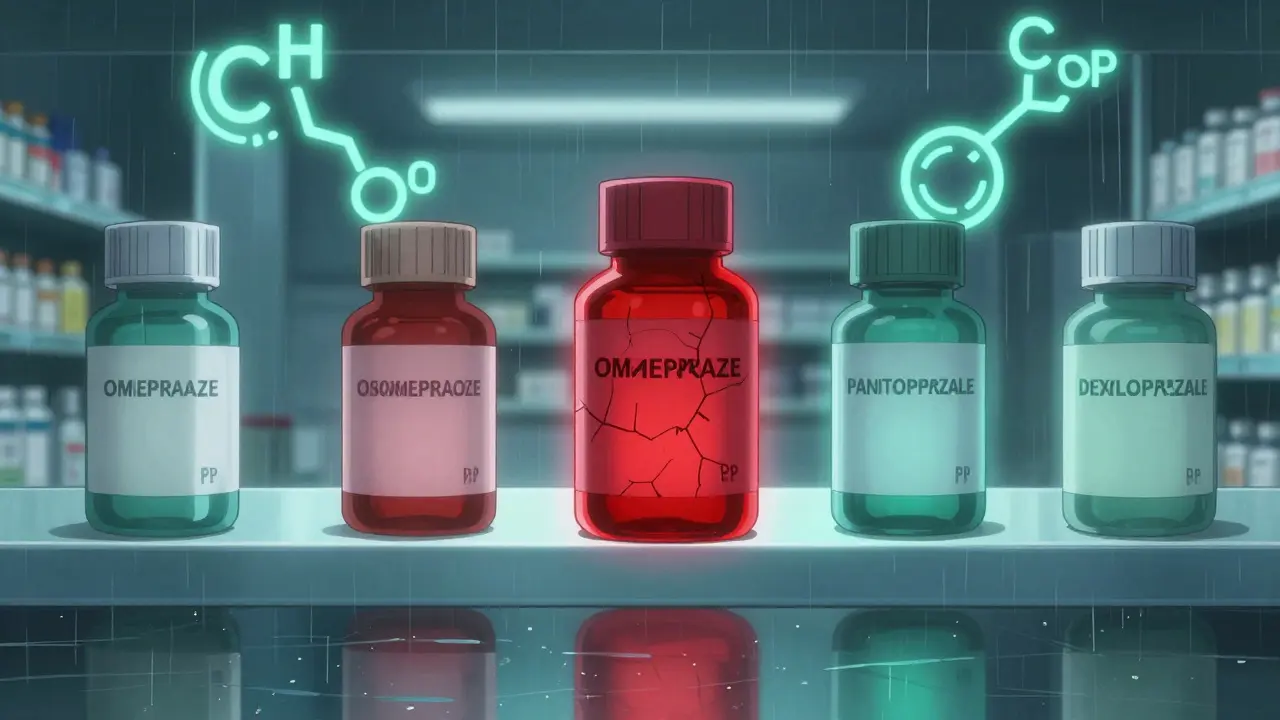
Not All PPIs Are the Same
This is where things get practical. You don’t have to avoid PPIs entirely - you just need to pick the right one.
- Omeprazole and esomeprazole are the worst offenders. They bind tightly to CYP2C19 and sharply reduce clopidogrel’s effectiveness. The FDA even added a black box warning in 2014 advising against this combo.
- Lansoprazole has a moderate effect. It’s not ideal, but sometimes used if alternatives aren’t available.
- Rabeprazole has a mixed profile. It’s less dependent on CYP2C19, but its metabolites can still interfere slightly.
- Pantoprazole and dexlansoprazole barely touch CYP2C19. Studies show pantoprazole reduces clopidogrel activation by only 14% - a difference that doesn’t appear to affect patient outcomes.
That’s why guidelines from the American College of Cardiology (2023) and the European Society of Cardiology now say: if you need a PPI, choose pantoprazole or dexlansoprazole. Avoid omeprazole and esomeprazole like a landmine.
Who’s at Real Risk?
Not everyone on clopidogrel will have problems. But some people are more vulnerable.
First, if you have a CYP2C19 loss-of-function gene variant - about 30% of people do - your body already struggles to activate clopidogrel. Adding omeprazole on top of that can double your risk of stent thrombosis or another heart attack. Genetic testing costs around $350-$500 and is recommended for high-risk patients, especially those who’ve had a stent placed recently.
Second, if you have multiple risk factors for stomach bleeding - like being over 65, taking aspirin or warfarin, having a past ulcer, or testing positive for H. pylori - your need for a PPI is clear. The CURE trial showed dual antiplatelet therapy (aspirin + clopidogrel) increases GI bleeding risk by 50%. In these cases, skipping a PPI is more dangerous than choosing the wrong one.
What Do Doctors Really Do?
There’s a split in the medical community. Some cardiologists swear by the interaction. Dr. Deepak Bhatt, who led the TRITON-TIMI 38 trial, saw a 53% spike in stent clots when patients took omeprazole. Others, like Dr. Marc Cohen from the COGENT trial, argue the effect is too small to matter in real life. His study found no increase in heart attacks or death when PPIs were used.
But real-world data tells a clearer story. After the FDA’s 2014 warning, omeprazole prescriptions with clopidogrel dropped by 24%. Today, 42.7% of clopidogrel users in the U.S. get pantoprazole instead - up from just 15% in 2010. And in hospitals, many have switched their formulary to pantoprazole as the default PPI for cardiac patients.
Still, about 31.5% of Medicare patients on clopidogrel are still getting omeprazole - that’s over 1.8 million people. Why? Cost. Omeprazole costs $0.38 per pill. Pantoprazole? $1.27. For patients on fixed incomes, that difference matters. But when your life is on the line, the cheaper option might not be the safer one.
What Should You Do?
If you’re taking clopidogrel and a PPI:
- Check your PPI name. If it’s omeprazole or esomeprazole, talk to your doctor. Don’t stop it yourself - but do ask if switching is right for you.
- Ask about pantoprazole or dexlansoprazole. These are your safest options. They protect your stomach without weakening your heart medication.
- If you can’t switch PPIs, space out the doses. Take clopidogrel at night, PPI in the morning. This doesn’t eliminate the interaction, but it reduces the overlap in enzyme competition.
- Ask if genetic testing is right for you. Especially if you’ve had a stent, a heart attack, or a family history of clotting problems.
And if you’re not on clopidogrel but are considering it - ask your doctor about alternatives. Ticagrelor and prasugrel don’t rely on CYP2C19. They work faster and more reliably. But they cost over 100 times more than generic clopidogrel. For many, clopidogrel is still the only affordable option - which is why this interaction remains so important.

What’s Changing Now?
Recent studies are adding nuance. A 2024 study in Nature Scientific Reports found no link between omeprazole and stroke risk in over 12,000 patients. That’s encouraging. But another 2024 paper in Circulation Research showed PPIs may reduce nitric oxide - a molecule that helps blood vessels relax. That could mean even the "safe" PPIs have subtle heart effects.
The FDA is currently reviewing new data from the PEGASUS trial, which showed pantoprazole cut GI bleeding by over half without increasing heart events. That could lead to updated labeling and clearer guidance.
Meanwhile, research continues into next-gen antiplatelets that bypass CYP2C19 entirely. But until those become affordable, clopidogrel will remain the backbone of treatment for millions.
Bottom Line
You don’t need to fear PPIs. You need to choose wisely. If you’re on clopidogrel, your stomach protection shouldn’t come at the cost of your heart safety. Omeprazole and esomeprazole are risky. Pantoprazole and dexlansoprazole are not. Ask your doctor which one you’re on. If you’re not sure, check your prescription bottle. Your life might depend on it.





sue spark
So if you're on clopidogrel and your stomach is acting up don't just grab the first PPI you see at the pharmacy
Tiffany Machelski
i just found out my doc gave me omeprazole and i didnt even know there was a problem with it
SHAMSHEER SHAIKH
Dear esteemed colleagues and fellow medical practitioners, I must emphasize with the utmost gravity that the pharmacokinetic interference between clopidogrel and proton pump inhibitors is not merely theoretical, but empirically substantiated across multiple randomized controlled trials and real-world observational cohorts. The CYP2C19 isoenzyme pathway is a critical nexus, and its inhibition by omeprazole and esomeprazole constitutes a clinically significant, potentially life-threatening drug interaction that demands immediate correction in clinical practice.
James Rayner
It's wild how something so simple-like which pill you take for heartburn-can ripple through your whole body like a stone dropped in a pond. We think we're just fixing one problem, but the body's systems are all tangled up. I'm glad we're starting to pay attention to these hidden connections. 🤔
Souhardya Paul
My hospital switched to pantoprazole as the default last year and honestly it was a no-brainer. We had a few patients with stent issues before, and after the change, zero new events in the cardiac unit. Cost is a factor, sure, but safety has to come first. Also, patients are way more likely to stick with a med if they know it's not working against their other meds.
Josias Ariel Mahlangu
People take pills like candy these days. No wonder we have so many problems. If you can't follow basic medical advice about drug interactions, maybe you shouldn't be on so many medications at all.
anthony epps
so pantoprazole is the good one? i thought they were all the same
Andrew Sychev
THIS IS WHY WE CAN'T HAVE NICE THINGS. Doctors are still prescribing omeprazole like it's 2008. People are dying because someone didn't want to spend 90 cents more per pill. This isn't science-it's corporate greed wrapped in a white coat.
Dan Padgett
You know, in my village back home, we used to say, 'The medicine that heals one part may poison another.' This whole thing with clopidogrel and PPIs? It's like that old wisdom turned into a lab report. We're trying to fix one hole in the boat but making another bigger one. Maybe the answer isn't just swapping pills, but asking why we need so many pills in the first place. The body isn't a machine with separate parts-it's a river, and every stone we throw changes the flow.