Thiazide diuretics like hydrochlorothiazide effectively lower blood pressure but can raise uric acid levels, increasing gout risk. Learn who’s most at risk, how to manage it, and safer alternatives.
Gout: What It Is, Why It Happens, and How to Find Relief
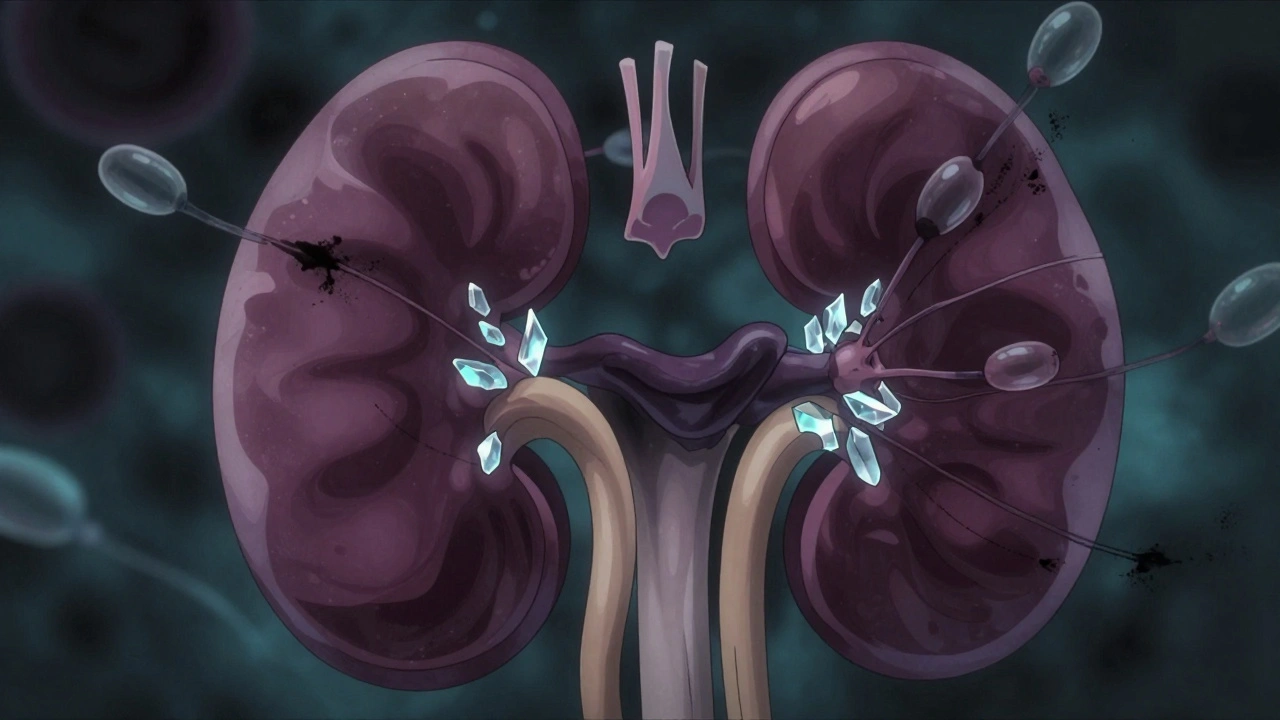
Ever felt a sudden, burning pain in your big toe that seemed to come out of nowhere? That’s a classic gout flare. Gout is a form of arthritis caused by too much uric acid building up in your blood, forming sharp crystals in joints. Those crystals are the real culprits behind the intense pain, swelling, and redness you notice during an attack.
Spotting the Warning Signs
Gout doesn’t always announce itself with a dramatic toe pain. Some people get it in the ankle, knee, or even the fingers. The hallmark signs are:
- A sudden, throbbing joint pain, often at night.
- Warm, red, and tender skin over the joint.
- Limited movement because the joint feels stiff.
- Symptoms that can subside after a few days but return weeks or months later.
If you’ve ever experienced any of these, it’s worth checking your uric‑acid level with a simple blood test.
What Triggers a Gout Attack?
Uric acid builds up when your body breaks down purines – substances found in many foods and drinks. High‑purine foods (like organ meats, sardines, and anchovies) and sugary beverages can push your levels over the edge. Alcohol, especially beer, also interferes with how your kidneys clear uric acid. Even dehydration, sudden weight changes, or a new medication can tip the balance and spark a flare.
For most folks, making a few everyday tweaks can keep attacks at bay. Drinking plenty of water, limiting alcohol, and swapping high‑purine meals for low‑purine options (think dairy, nuts, and most fruits) are practical first steps.
Getting Relief Fast
When a gout attack hits, you want quick relief. Over‑the‑counter NSAIDs (like ibuprofen) can knock down pain and swelling. If those aren’t enough, doctors may prescribe colchicine or a short course of steroids. The key is to start treatment early – the sooner you act, the shorter the flare.
Long‑term, keeping uric acid low is the goal. Medications such as allopurinol, febuxostat, or probenecid help the body either produce less uric acid or excrete more of it. Your doctor will choose the right one based on your health profile and how often you flare.
Everyday Lifestyle Tips
Besides meds, lifestyle habits matter. Aim for at least eight glasses of water a day to help flush uric acid. Keep your weight in a healthy range; excess pounds raise uric‑acid levels. When you’re dining out, ask for grilled or baked proteins instead of fried dishes, and skip the shrimp cocktail if you’re prone to attacks.
Exercise is good, but avoid intense workouts that can temporarily raise uric acid. Light activities like walking, swimming, or cycling keep joints flexible without overloading them.
When to See a Doctor
If you’ve had more than one gout flare, or if the pain doesn’t improve after a few days of OTC treatment, book an appointment. A doctor can confirm the diagnosis, check for kidney stones (a common gout companion), and tailor a medication plan that prevents future attacks.
Remember, gout is manageable. Knowing the triggers, acting fast during flares, and staying on a uric‑acid‑lowering plan can let you live pain‑free. So next time your toe starts hurting, you’ll know exactly what to do.
Curious if your blood pressure meds can affect gout? This in-depth article explains the connection between terazosin and gout, how terazosin may influence uric acid levels, and what patients need to watch for. You'll get science-backed info, real-world tips, and practical guidance to manage both conditions without getting overwhelmed. We clear up common myths and give you the tools to talk with your doctor about terazosin and your risk for gout.