Bacterial vs. Viral Infections: How to Tell Them Apart and What Actually Works
Every winter, the same thing happens: someone in your house gets sick. Fever. Sore throat. Cough. Runny nose. You grab the thermometer, check the symptoms, and ask: bacterial or viral? The answer matters more than you think - because treating them the wrong way can make things worse, not better.
What’s Really Going On Inside Your Body?
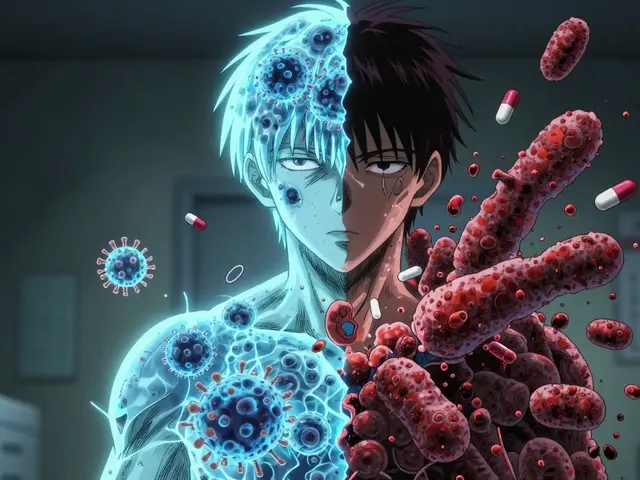
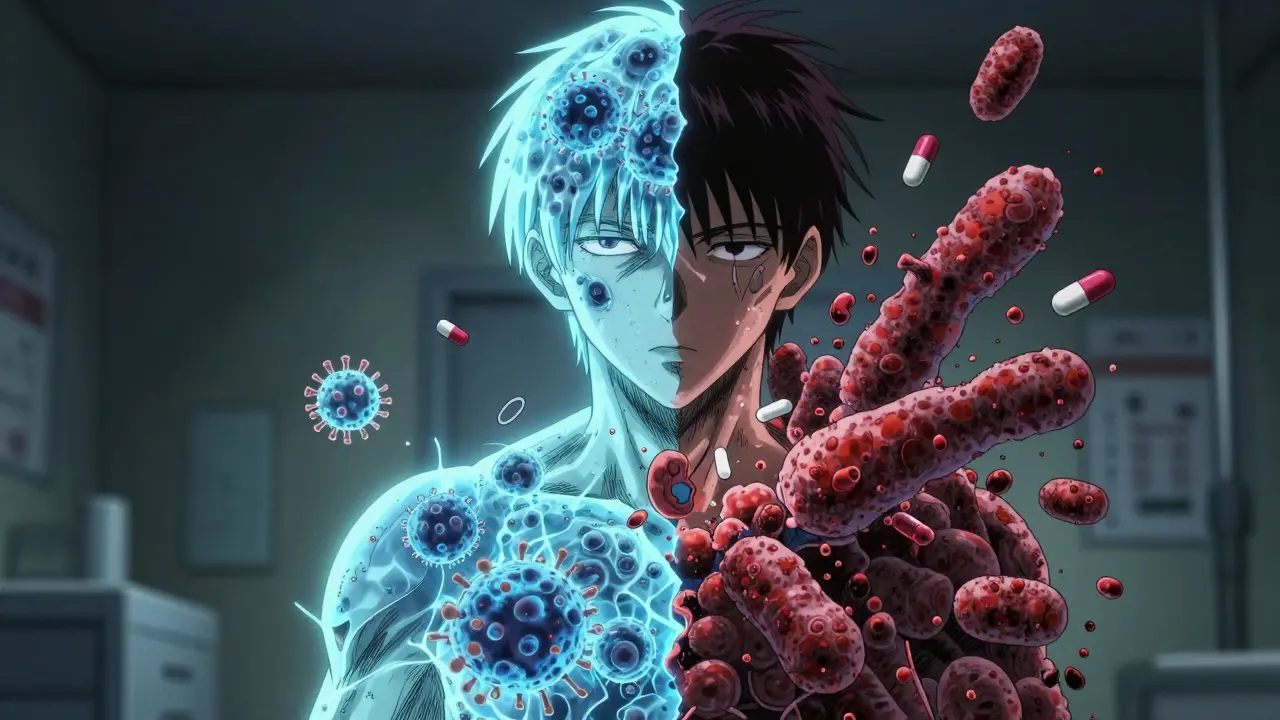
Bacteria and viruses aren’t just different germs - they’re completely different kinds of invaders. Bacteria are single-celled living organisms. They eat, grow, and multiply on their own. You find them everywhere: on your skin, in your gut, even in soil and water. Some are harmless. Some, like the ones causing strep throat or urinary tract infections, can make you sick. Viruses are not alive in the way bacteria are. They’re basically genetic material wrapped in a protein coat. They can’t reproduce by themselves. They need to break into your cells and hijack them to make copies. That’s why you can’t catch a cold from a doorknob unless the virus gets into your body first. This difference is why antibiotics work on bacteria but do absolutely nothing to viruses. Antibiotics attack the machinery bacteria use to survive - their cell walls, their protein factories. Viruses don’t have any of that. They’re just parasites hiding inside your cells. You can’t kill them without hurting your own cells.Common Infections: What’s Bacterial, What’s Viral?
It’s easy to mix them up because they often feel the same. But here’s the real-world breakdown:- Bacterial infections: Strep throat (caused by group A strep), urinary tract infections (UTIs), tuberculosis, some types of pneumonia, and bacterial sinusitis.
- Viral infections: The common cold (rhinovirus), flu (influenza), chickenpox, COVID-19, and most cases of bronchitis and sore throat.
Symptoms: How to Spot the Difference (Without a Lab Test)
There’s no magic symptom that always tells you which one you’ve got. But patterns help. Viral infections usually start fast. You wake up feeling awful - body aches, low-grade fever (under 100.4°F), runny nose, cough. You feel peak sick around day 2 or 3, then start improving by day 5 to 7. That’s the common cold or flu pattern. Bacterial infections often hang on longer. You might feel better for a few days, then get worse again. Or your fever spikes above 101°F and doesn’t budge. A sore throat with white patches on the tonsils? That’s more likely strep. Sinus pressure lasting more than 10 days? Could be bacterial sinusitis. Here’s what doctors look for in the clinic:- Strep throat? Tonsils with pus, swollen neck glands, fever, no cough. That’s the Centor Criteria - a simple scoring system doctors use. Three or more of these signs? You’re 50-55% likely to have strep.
- Flu? Sudden fever, chills, muscle pain, fatigue. Often hits hard and fast. No runny nose? Still possible. Flu can come without congestion.

Testing: How Doctors Know for Sure
You can’t tell by looking. That’s why tests matter. For strep throat, a quick throat swab gives results in minutes. It’s 95% accurate. If it’s negative but the doctor still suspects strep, they’ll send a culture - the gold standard - which takes 24 to 48 hours but is 98% accurate. For viruses like flu or COVID-19, PCR tests are the most reliable. They detect the virus’s genetic material. Accuracy is 90-95% if done within the first 72 hours of symptoms. Rapid antigen tests are faster but less sensitive - they can miss early infections. And now there’s something new: the FebriDx test. Approved by the FDA in 2020, it checks two biomarkers - CRP (a sign of inflammation) and MxA (a protein your body makes only when fighting a virus). It tells you within 10 minutes whether your infection is likely bacterial or viral. One study showed it cut unnecessary antibiotic use by half in doctor’s offices.Treatment: Antibiotics Don’t Work on Viruses - And That’s a Good Thing
If you have a bacterial infection, antibiotics are lifesavers. Penicillin for strep throat. Ciprofloxacin for a UTI. A 10-day course clears the infection. But if you have a virus? Antibiotics won’t touch it. They’re like trying to fix a broken phone with a hammer. You’re not helping - you’re just making noise. And here’s the scary part: every time you take an antibiotic when you don’t need it, you’re helping bacteria become stronger. That’s antibiotic resistance. The WHO calls it one of the top 10 global health threats. In 2019, drug-resistant infections killed 1.27 million people worldwide. By 2050, that number could hit 10 million - more than cancer. In the U.S. alone, doctors prescribe 47 million unnecessary antibiotic courses every year - mostly for viral colds and coughs. That’s not just wasteful. It’s dangerous. For viral infections, treatment is simple: rest, fluids, fever reducers like acetaminophen or ibuprofen. For flu, if you catch it early - within 48 hours - antivirals like oseltamivir (Tamiflu) can shorten your illness by 1 to 2 days. For severe COVID-19, remdesivir can help hospitalized patients recover faster.Why Misdiagnosis Costs Us All
It’s not just about you. It’s about everyone. When people take antibiotics for viral infections, they’re more likely to get sick again - and faster. A 2022 study in JAMA Internal Medicine found that patients who got unnecessary antibiotics were 65% more likely to return to the doctor for the same symptoms within a year. Why? Because antibiotics wipe out good bacteria in your gut and throat, making you more vulnerable to future infections. And then there’s the cost. In the U.S., inappropriate antibiotic use costs the healthcare system $1.1 billion a year. Viral respiratory infections - the colds and flus - cost $45 billion in medical bills and lost workdays. Kids get six to eight viral infections a year. That’s 22 million missed school days and 20 million lost workdays for parents in the U.S. alone. We treat these like emergencies. But most just need time.
What You Can Do Right Now
Don’t pressure your doctor for antibiotics. Ask: “Is this bacterial or viral?” If they say viral, ask: “What can I do to feel better?” That’s the right question. If you have a sore throat with no cough, fever, and swollen glands - get tested for strep. Don’t guess. If you’re sick for more than 10 days and getting worse, see a doctor. That’s when bacterial infections often sneak in. Wash your hands. Get your flu shot. Stay home when you’re sick. These simple things stop viruses from spreading. And if your child has a cold? Resist the urge to reach for antibiotics. Most colds clear up on their own. Let your body do its job.The Future: What’s Coming Next
Scientists are working on better tools. At the University of Queensland, researchers are testing new compounds that target how bacteria stick to human cells - a way to fight resistant strains without killing off good bacteria. Two of these drugs are in Phase II trials as of late 2024. Phage therapy - using viruses that infect bacteria - is showing 85% success in European trials for stubborn infections. It’s not mainstream yet, but it’s promising. And universal coronavirus vaccines? They’re in Phase III trials. If they work, they could prevent future pandemics like COVID-19. The bottom line? We’re not just fighting germs. We’re fighting our own habits. Misusing antibiotics is like pouring gasoline on a fire. The solution isn’t stronger drugs - it’s smarter use.When to See a Doctor
You don’t need to rush in for every sniffle. But call your doctor if:- Your fever stays above 101°F for more than 3 days
- You have trouble breathing or chest pain
- Your symptoms get better, then suddenly get worse
- You have a sore throat with white patches or swollen lymph nodes
- You’re over 65, pregnant, or have a weakened immune system