Generic Drug Safety in Older Adults: What You Need to Know About Age-Related Risks

When you’re over 65, taking medication isn’t just about popping a pill-it’s about surviving a minefield. Your body changes. Your liver slows down. Your kidneys don’t flush things out like they used to. And if you’re on five or more drugs? You’re at an 82% higher risk of a dangerous reaction. That’s not a guess. That’s from a 2023 study in the PMC database. Now, add in generic drugs-cheaper, widely used, and trusted by most doctors-and you’ve got a situation that needs careful handling.
Are Generic Drugs Really the Same?
The FDA says yes. Generic drugs must contain the same active ingredient, strength, and dosage form as the brand-name version. They must also be bioequivalent-meaning they get into your bloodstream at nearly the same rate and amount. That’s the law. And for most people, that’s enough. But for older adults? It’s not always that simple.
Take warfarin, a blood thinner. The brand-name version is Coumadin. The generic is just called warfarin. The FDA says they’re interchangeable. And in lab tests, generic warfarin matches brand-name within 98.7% accuracy. But here’s the catch: warfarin has a narrow therapeutic index. That means even a tiny difference in how your body absorbs it can cause a blood clot-or a bleed. A 2023 study found that 42% of seniors believed generic warfarin was riskier, even though studies show no real difference in safety. That fear isn’t irrational. It’s based on real stories. One woman’s TSH levels went haywire after switching from brand-name Synthroid to generic levothyroxine. It took three dosage changes over six months to stabilize her.
The truth? For most drugs, generics are just as safe. But for a few-like warfarin, digoxin, or phenytoin-switching between brands or generics can cause problems. That’s why doctors often stick with one version for older patients. Consistency matters more than cost.
Why Your Body Reacts Differently After 65
Your body isn’t the same as it was at 40. By 75, your liver may metabolize drugs 30% slower. Your kidneys clear them even less efficiently. Your body fat increases. Water decreases. That changes how drugs spread and stay in your system.
Take a common painkiller like ibuprofen. At 30, your kidneys flush it out in hours. At 75? It lingers. That’s why older adults get stomach bleeds, kidney damage, or high blood pressure from doses that were fine decades ago.
Or consider sleep aids and anxiety meds. Benzodiazepines like diazepam or lorazepam? They’re on the Beers Criteria 2023 list of medications to avoid in older adults. Why? They cause dizziness, confusion, and falls. One fall can mean a hip fracture. A hip fracture can mean losing independence-or your life.
And then there’s insulin. Or sulfonylureas like glipizide. These lower blood sugar. But in older adults, the body doesn’t warn you when it drops too low. No shaking. No sweating. Just sudden confusion… then a fall… then a trip to the ER. Studies show 20-25% of hypoglycemic episodes in seniors lead to falls or brain injury.
The Polypharmacy Trap
Most older adults take multiple medications. Not because they want to-but because they have arthritis, high blood pressure, diabetes, heart disease, and maybe depression. Each condition gets its own pill. And each pill interacts.
Here’s the math:
- 2 drugs? 13% chance of a bad reaction
- 5 drugs? 58% chance
- 7+ drugs? 82% chance
That’s not a typo. It’s from a 2023 study tracking 12,000 seniors. And it’s not just about the drugs themselves-it’s about combinations. Opioids plus benzodiazepines? Overdose risk jumps 154%. Opioids plus gabapentin? Respiratory depression risk up 70%. These aren’t rare. They’re common.
And here’s the kicker: many of these drugs are generics. Amlodipine for blood pressure? Generic. Metformin for diabetes? Generic. Sertraline for depression? Generic. All fine on their own. But together? They pile up. And your body can’t handle it.
The Beers Criteria: Your Secret Weapon
Every three years, the American Geriatrics Society updates the Beers Criteria. It’s a list of medications that are risky for older adults-no matter if they’re brand or generic. It’s not a suggestion. It’s a warning. And it’s backed by data from over 200 clinical studies.
Here’s what’s on the 2023 list:
- Anticholinergics (like diphenhydramine in Benadryl): linked to memory loss and confusion
- Cyclobenzaprine (Flexeril): a muscle relaxant that increases fall risk by 40%
- NSAIDs (ibuprofen, naproxen): kidney damage and stomach bleeds
- SNRIs like venlafaxine: increase fall risk by 37%
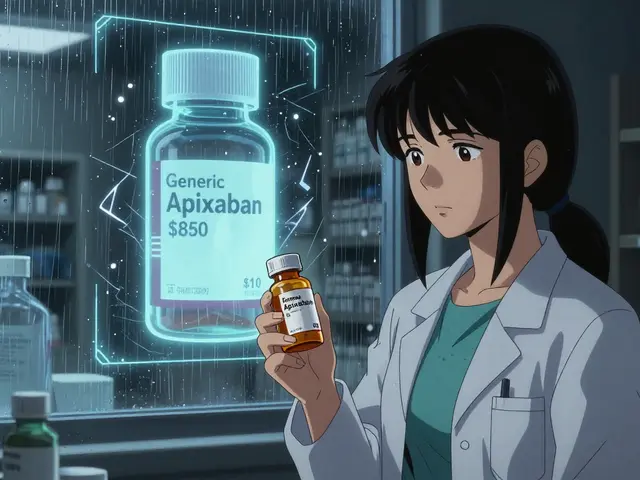
- Direct oral anticoagulants like rivaroxaban: higher bleeding risk in those over 75
Notice something? It doesn’t say “brand-name.” It says “medication.” The risk is in the drug, not the label. So if your doctor prescribes a generic version of one of these, it’s still risky.
The solution? Ask your doctor: “Is this on the Beers Criteria?” If they don’t know, ask for a pharmacist consult. Pharmacists are trained to spot these red flags.
What You Can Do to Stay Safe
Generic drugs aren’t the enemy. But you need to manage them wisely.
1. Get a full medication review every 3 months. A 2022 meta-analysis showed that pharmacist-led reviews cut adverse events by 27%. Bring every pill-prescription, OTC, supplement-to your appointment. Even that ginkgo biloba you take for memory? It can interfere with blood thinners.
2. Use a pill organizer. Color-coded, labeled containers reduce errors by 34%. Automated dispensers that beep when it’s time to take a pill? Even better. One study showed they cut missed doses by 50%.
3. Ask for larger print. Sixty-five percent of seniors have vision problems. If you can’t read the label, you can’t take the pill right. Pharmacies can print bigger labels. Ask for it.
4. Never stop or switch without talking to your doctor. A 2022 study found that 28% of medication errors in seniors came from switching between similar-looking generic pills. One pill looks like another. The name is different. The dose is close. It’s easy to mix up.
5. Know your high-risk drugs. If you’re on warfarin, digoxin, insulin, or any anticoagulant, keep a log. Note your symptoms: dizziness, confusion, bruising, nausea. Report them immediately. Don’t wait for your next appointment.
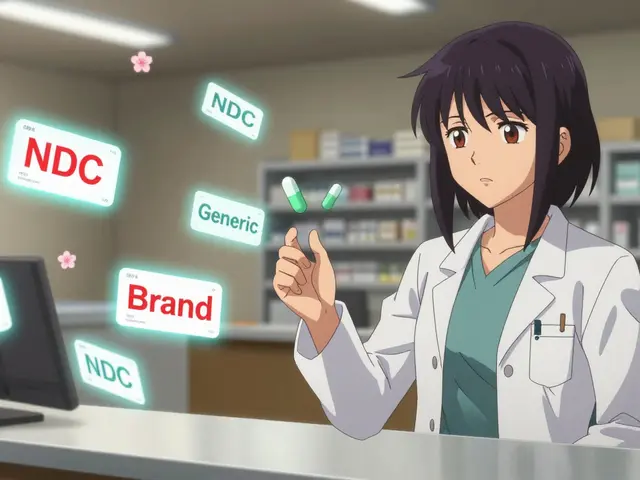
When to Stick With Brand-Name
There’s no rule that says you must take generic. If you’ve been on brand-name warfarin for years and your INR levels are stable? Keep it. If your mother’s TSH levels jumped after switching to generic levothyroxine? Go back. Insurance might push back-but your health comes first.
Some Medicare Advantage plans have tiered pricing. Brand-name drugs cost more. But if your doctor writes a letter saying the generic caused problems, you can appeal. You’re not being difficult. You’re being smart.
And if you’re paying out of pocket? Generic is still cheaper. But not always worth the risk. Ask your pharmacist: “Is this a narrow therapeutic index drug?” If yes, ask if the brand is covered under a patient assistance program. Many are.
The Bottom Line
Generic drugs are safe for most older adults. But safety isn’t just about the pill-it’s about your body, your other meds, your vision, your memory, and your support system. The real danger isn’t the generic label. It’s the assumption that “same drug = same result.”
Older adults aren’t just small adults. Their bodies process medicine differently. And when you’re on five or more pills, even a tiny difference matters.
Do this now: Write down every medication you take. Bring it to your next doctor visit. Ask: “Is this on the Beers Criteria?” “Is there a safer alternative?” “Should I stay on brand?”
You’re not being difficult. You’re being the best advocate for your health. And that’s worth more than any savings on a prescription.
Are generic drugs as safe as brand-name drugs for older adults?
For most medications, yes-generic drugs are just as safe and effective as brand-name versions. The FDA requires them to meet strict bioequivalence standards. But for drugs with a narrow therapeutic index-like warfarin, digoxin, or levothyroxine-even small differences in absorption can cause problems. Older adults, due to slower metabolism and kidney function, are more vulnerable to these small changes. Always consult your doctor before switching.
Why are older adults more at risk for adverse drug reactions?
As we age, our liver and kidneys process drugs more slowly, so medications stay in the body longer. Body composition changes too-more fat, less water-which affects how drugs are distributed. Plus, many seniors take five or more medications, increasing the chance of harmful interactions. The risk of an adverse reaction jumps to 82% when taking seven or more drugs.
What medications should older adults avoid?
The 2023 Beers Criteria lists several high-risk medications, including benzodiazepines (like diazepam), anticholinergics (like diphenhydramine), cyclobenzaprine (Flexeril), NSAIDs (like ibuprofen), and certain anticoagulants like rivaroxaban for those over 75. These drugs increase risks of falls, confusion, bleeding, and kidney damage. Generic versions carry the same risks.
Can switching from brand-name to generic cause problems?
Yes, especially for drugs with a narrow therapeutic index. For example, switching from brand-name Synthroid to generic levothyroxine has caused unstable thyroid levels in some seniors. Warfarin users have reported changes in INR levels after switching generics. If you notice new side effects after a switch-like dizziness, confusion, or unusual bruising-contact your doctor immediately.
How can I reduce my risk of medication errors?
Keep a current list of all medications-including supplements-and review it with your doctor or pharmacist every 3 months. Use a pill organizer. Ask for larger-print labels. Never stop or switch meds without talking to your provider. Consider using an automated dispenser. These steps can reduce errors by up to 50%.


Yash Hemrajani
So let me get this straight - the FDA says generics are bioequivalent, but if you’re over 65 and on warfarin, you might as well be playing Russian roulette with a pill organizer? Classic. I’ve seen grandmas switch to generic levothyroxine and end up in the ER because their TSH went full chaos mode. The system’s not broken - it’s just designed for people who still have kidneys that work.
Rosy Wilkens
Let’s be honest - this isn’t about safety. It’s about corporate greed disguised as cost-saving. The same pharmaceutical conglomerates that made billions off brand-name drugs quietly bought up generic manufacturers and now push them like candy. They know older adults are less likely to fight back. And the FDA? They’re on the payroll. Look at the revolving door between regulators and Big Pharma. This is a slow-motion poisoning, and nobody wants to admit it.
Andrea Jones
Y’all are overcomplicating this. If your grandma’s on five meds and her pill organizer looks like a sci-fi control panel, the problem isn’t the generic label - it’s the sheer volume. I help my mom manage her meds, and the biggest win? Cutting three things she didn’t even need. One was a ‘memory supplement’ that was just ginkgo + sugar. She’s been walking better since we axed it. Sometimes the best drug is no drug.
Justina Maynard
It is not merely a matter of bioequivalence; it is a matter of pharmacokinetic individuality, particularly in the context of age-related alterations in hepatic metabolism and renal clearance. The FDA’s bioequivalence threshold of 80–125% AUC and Cmax is statistically acceptable for a population average - but not for a 78-year-old woman with a creatinine clearance of 35 mL/min. When you compound this with polypharmacy, the margin for error becomes not just narrow - it is nonexistent. This is why clinical vigilance must supersede regulatory compliance.
Clay Johnson
Drugs are just chemicals. The body is just a machine. The system is just a story we tell ourselves to feel safe. You take a pill. It does something. You don’t know why. You trust it. That’s not medicine. That’s faith. And faith doesn’t scale with age.
Jermaine Jordan
STOP. RIGHT. NOW. If you’re over 65 and still taking benzodiazepines, NSAIDs, or anticholinergics - you are not just at risk. You are already in the danger zone. This isn’t a ‘maybe’ - it’s a ticking clock. Your doctor didn’t wake up this morning and say, ‘I hope this person falls.’ They were trained to treat symptoms, not systems. But YOU? You can break the cycle. Ask for a review. Demand a pharmacist. Fight for your independence. Your life is worth more than a $3 co-pay.
Chetan Chauhan
bro this whole post is fearmongering. i take generic metformin and amlodipine and im 72 and still hiking. generics are fine. its the docs who overprescribe. stop blaming the pills. blame the prescriptions. also why is everyone so scared of ibuprofen? i take 800mg daily and my kidneys are fine. maybe you just need to eat less salt?
Phil Thornton
My aunt switched from brand-name Synthroid to generic. TSH went from 2.1 to 8.9. Three months. Three doctor visits. One panic attack. She’s back on brand. Insurance cried. She didn’t. You don’t gamble with your thyroid.
Pranab Daulagupu
For seniors, consistency > cost. If you’ve been stable on brand-name warfarin for 10 years, don’t switch. If your INR is steady, don’t risk it. Generic is great - until it isn’t. And when it isn’t, it’s not just a lab value - it’s a hospital bed, a fall, a loss of dignity. Your pharmacist can help you navigate this. Ask. They’re the unsung heroes.
Barbara McClelland
Hey - I’m a nurse and I’ve seen this too many times. A 76-year-old man on five generics, including gabapentin and sertraline, starts nodding off in his chair. Turns out his daughter switched his meds to save $12 a month. He ended up in rehab after a fall. Don’t let cost be the silent killer. Bring every pill - even the ‘harmless’ ones - to your next visit. Your doctor doesn’t know what’s in your cabinet unless you tell them.
Alexander Levin
They’re watching us. The pills. The scanners. The insurance algorithms that flag ‘high-risk seniors’ and push generics like they’re selling a subscription. I don’t trust any of it. 🤖💊
Ady Young
I used to think generics were just cheaper versions. Then my dad had a bad reaction to a switch in his digoxin. Turns out the filler ingredients vary - and for someone with a sensitive system, that’s enough. Now we stick with the same pharmacy, same batch, same version. It’s not about brand loyalty - it’s about control. And honestly? It’s worth the extra $5.
Travis Freeman
My dad’s from India. He took generic metformin for 15 years. No issues. But when he moved to the US and switched to a different generic, his blood sugar went wild. Turned out the inactive ingredients changed. He’s back on the Indian brand - imported, expensive, but safe. Culture matters. Supply chains matter. Your body remembers what it’s used to. Don’t underestimate that.