Exercise Modifications for Fatigue on Beta-Blockers and Other Drugs

Beta-Blocker Exercise Adjustment Calculator
If you're taking beta-blockers, your heart rate doesn't respond the same way during exercise. This calculator helps you determine your safe exercise intensity using the RPE scale and talk test method. Never use traditional heart rate zones while on beta-blockers.
No Effort
Very Light
Light
Moderate
Moderate
Vigorous
Vigorous
Max Effort
What does this mean for you?
At RPE 14, you should be able to talk comfortably but not sing. Your breathing should be elevated but not labored. This is the safe zone where you can exercise without overexerting your heart while on beta-blockers.
Your Personalized Exercise Plan
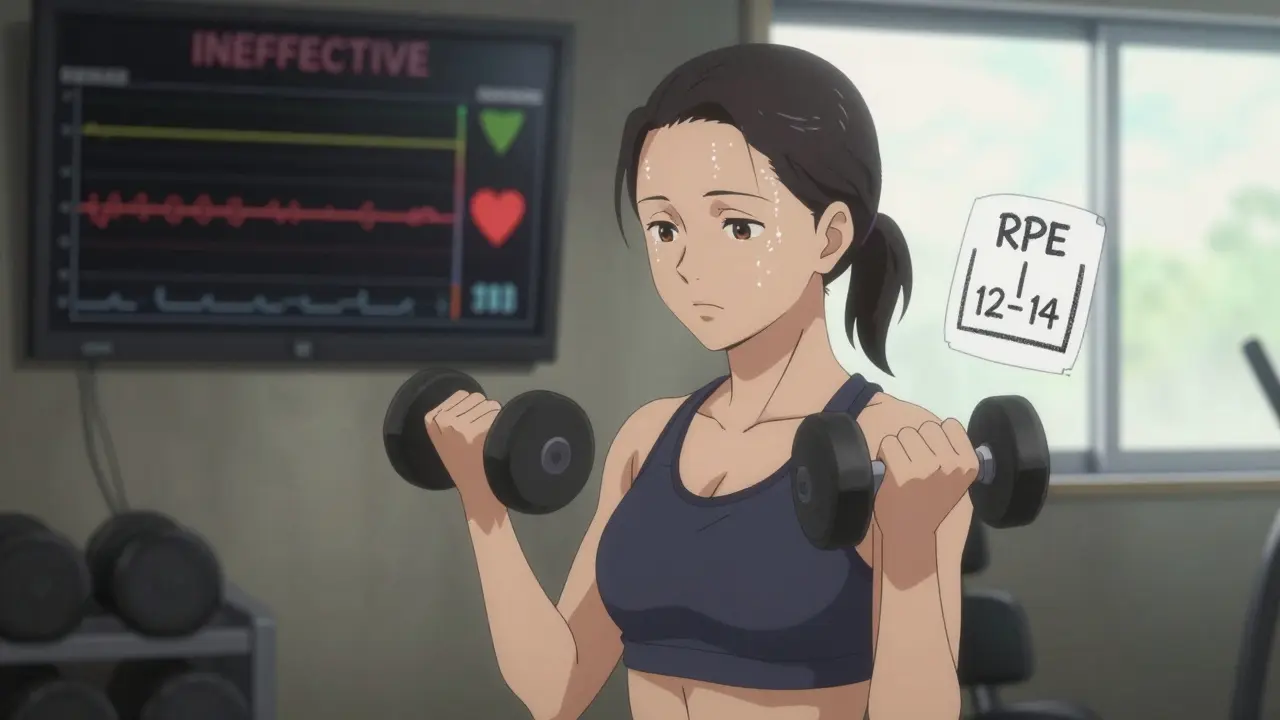
Recommended Intensity: RPE 12-14 (Moderate)
How to Gauge Effort: You should be able to speak in full sentences without gasping for breath.
Weekly Activity Target: 180 minutes
Warm-up: 12 minutes
Exercise Type: Walking, cycling at steady pace, swimming (avoid high-intensity intervals)
Feeling worn out during a walk or struggling to keep up on your usual bike ride? If you're taking beta-blockers-medications like metoprolol, propranolol, or atenolol-you're not alone. Around 33 million Americans take these drugs for high blood pressure, heart rhythm issues, or heart failure. But one of the most common side effects isn’t dizziness or dry mouth-it’s fatigue during physical activity. And it’s not just in your head. Your body is literally being held back by the medicine keeping your heart safe.
Why Beta-Blockers Make You Tire So Fast
Beta-blockers work by blocking adrenaline. That’s good for your heart-it slows your heart rate, lowers blood pressure, and reduces strain. But that same effect makes exercise feel harder. Your heart can’t speed up the way it used to. Studies show your maximum heart rate drops by 20-30%. If you used to hit 170 bpm during a run, you might now max out at 120-130 bpm, even if you’re pushing just as hard.This isn’t about being out of shape. It’s physics. Your body needs oxygen to move. Oxygen delivery depends on how fast your heart pumps and how much it pushes out with each beat. When your heart rate is capped, your body tries to make up the difference by squeezing harder-but it often can’t keep up. That’s why you gasp for air sooner, your legs feel heavy, and you have to stop before you think you should.
VO₂ max-the measure of how much oxygen your body can use during exercise-drops by 10-15% on beta-blockers. That’s like carrying an extra 10 pounds everywhere you go. Other heart meds like ACE inhibitors or calcium channel blockers don’t do this. Diuretics might make you cramp, but they don’t stop your heart from racing. Beta-blockers are unique in how they throttle your cardiovascular response.
Heart Rate Monitors Are Useless (And Dangerous)
You’ve probably seen fitness trackers flashing your target heart rate zone: 60-70% for moderate, 70-85% for vigorous. If you’re on beta-blockers, those numbers are meaningless. Trying to hit them can make you overexert yourself without realizing it. The Mayo Clinic warns: “Exercising to reach an expected heart rate while on beta-blockers may cause overexertion and cause fatigue.”One Reddit user, CardioRunner87, shared that after starting 100mg of metoprolol, his 5K time went from 25:30 to 29:15-even though he felt like he was putting in the same effort. That’s a 15% drop in performance, not from laziness, but from biology. Your heart rate monitor doesn’t know you’re on medication. It just sees a low number and thinks you’re slacking.
What to Use Instead: The Talk Test and RPE Scale
Forget numbers. Start listening to your body.The tell test is simple: if you can talk comfortably but not sing, you’re at the right intensity. If you’re gasping for words, slow down. If you can chat easily, pick up the pace. This method works better than any heart rate zone for people on beta-blockers. The American Heart Association recommends it as the gold standard.
Another tool is the Borg Rating of Perceived Exertion (RPE) scale. It runs from 6 (no effort) to 20 (max effort). For moderate exercise, aim for 12-14. That’s where you feel challenged but not overwhelmed. For vigorous activity, go up to 15-17. Most beta-blocker users need to drop their target intensity by one level. If you used to train at 17, now aim for 14.
Dr. Martha Gulati from UCLA says this isn’t just advice-it’s evidence-based. In a 2022 study, patients who switched from heart rate tracking to RPE saw better adherence and fewer episodes of dizziness or exhaustion.
How to Adjust Your Workout Routine
You don’t have to stop exercising. You just have to change how you do it.- Extend your warm-up to 10-15 minutes. Your heart needs more time to adjust. A quick 5-minute stroll won’t cut it anymore.
- Lengthen your workouts. Since you’re working at lower intensity, you need more time to get the same benefit. Aim for 180-188 minutes of moderate activity per week instead of the standard 150.
- Swap high-intensity intervals for steady-state. HIIT can be risky. Your heart can’t spike fast enough to meet the demand. Instead, try walking uphill, cycling at a steady pace, or swimming. Dr. Sheldon Litwin’s 2021 research found that 2:1 work-to-rest intervals (e.g., 4 minutes walking, 2 minutes rest) improved endurance better than continuous exercise.
- Adjust strength training. Beta-blockers don’t weaken your muscles. You can still lift weights. But lower the load by 15-20%. Keep the reps the same. Focus on control, not speed. This keeps your heart from spiking while still building strength.
Watch for Warning Signs
Fatigue is normal. Danger isn’t.Pay attention to these red flags:
- Resting heart rate below 45 bpm with dizziness or lightheadedness
- Systolic blood pressure dropping below 90 mmHg during exercise
- Not sweating at all during mild activity-this can mean you’re dehydrating without realizing it
- Chest pain, extreme shortness of breath, or fainting
These aren’t normal side effects. They’re signs you need to stop and call your doctor. About 5% of beta-blocker users experience dangerously low heart rates. 3% see dangerous drops in blood pressure during activity. Don’t push through. Your heart is already working hard to stay healthy-don’t make it work harder than it should.

Other Drugs That Cause Exercise Fatigue
Beta-blockers aren’t the only culprits. Other medications can make you feel sluggish during workouts:- Diuretics (like furosemide) can drain your electrolytes, leading to cramps and weakness.
- Statins (for cholesterol) sometimes cause muscle pain or fatigue, especially in older adults.
- Antidepressants (especially SSRIs) can reduce energy levels and motivation.
- Calcium channel blockers (like amlodipine) may cause swelling in the legs, making walking harder.
If you’re on multiple meds and feel constantly tired, talk to your doctor. It might not be just one drug-it’s the combo. A medication review could help you find a better balance.
New Hope: Better Drugs and Smart Tech
The good news? Science is catching up.Newer beta-blockers like nebivolol (Bystolic) cause less reduction in VO₂ max-only 8-10% compared to 15% with older versions. They’re more selective, targeting the heart without affecting other systems as much.
Cardiopulmonary exercise testing (CPET) is becoming more common. This test measures exactly how your body responds to exercise while on medication. It’s the most accurate way to design a safe, effective workout plan tailored to you. Around 65% of U.S. hospitals with cardiac rehab now offer it.
Apple Watch’s latest software (version 9.1, released Sept 2023) now includes beta-blocker-adjusted heart rate zones. It doesn’t replace medical advice-but it’s a step toward tech that understands your body’s limits. Clinical validation is still ongoing, but it’s a sign we’re moving in the right direction.
Real People, Real Results
On the American Heart Association’s Support Network, user HeartWarrior42 switched from tracking heart rate to using the talk test after starting atenolol. She said: “I was ready to quit walking. Now I walk 45 minutes every day without panic. I feel like myself again.”On Drugs.com, 67% of 8,423 beta-blocker users reported exercise fatigue. But those who adjusted their routine-slowing down, listening to their body, ditching the heart rate monitor-reported better energy, better sleep, and more confidence.
You don’t need to be an athlete to benefit from movement. Walking, gardening, swimming, dancing-these count. You’re not failing. You’re adapting. And that’s strength.
Can I still do cardio if I’m on beta-blockers?
Yes, but you need to change how you measure intensity. Skip heart rate monitors. Use the talk test-can you speak in full sentences without gasping? Or use the Borg RPE scale and aim for 12-14 for moderate effort. Walking, cycling, and swimming are excellent choices. Avoid high-intensity intervals unless approved by your doctor.
Why do I feel so tired even when I’m not pushing hard?
Beta-blockers limit how fast your heart can beat, which reduces how much oxygen your muscles get during activity. Even light exercise can feel like a hard effort because your body can’t ramp up its delivery system the way it used to. This isn’t laziness-it’s a direct effect of the medication. Adjusting your pace and duration helps your body adapt.
Should I stop taking my beta-blocker if exercise is too hard?
Never stop or change your dose without talking to your doctor. Beta-blockers protect your heart. Stopping suddenly can cause rebound high blood pressure, rapid heart rate, or even a heart attack. Instead, talk to your provider about adjusting your exercise plan or exploring alternative medications like nebivolol that may cause less fatigue.
Is it safe to use a fitness tracker on beta-blockers?
You can use one, but don’t rely on it for intensity. Your heart rate numbers will be artificially low. Use the tracker only to monitor resting heart rate trends or to ensure you’re moving regularly. Focus instead on how you feel-your breathing, your energy, your ability to talk. Those are better indicators than any screen.
How long does it take to adjust to exercising on beta-blockers?
Most people notice improvement within 4-8 weeks as their body adapts to lower intensity. Your muscles get better at using oxygen, your breathing becomes more efficient, and you learn to read your body’s signals. Be patient. Progress isn’t about speed-it’s about consistency. Even slow movement builds heart health.
Do beta-blockers affect muscle strength?
No. Beta-blockers don’t weaken your muscles. You can still build and maintain strength. Just reduce the weight you lift by 15-20% and focus on controlled movements. Keep the same number of reps. Strength training is important-it helps your heart, too.
What if I still feel exhausted even after adjusting my routine?
Talk to your doctor. You might need a medication review. Could another drug be adding to the fatigue? Are you dehydrated or low on iron? Could your dose be too high? Sometimes, switching from propranolol to metoprolol or nebivolol helps. A simple blood test or CPET can reveal what’s really going on.
If you’re on beta-blockers, your fitness journey looks different now. But it’s not over. It’s just smarter. Slow down. Listen. Adjust. You’re not losing ground-you’re learning a new way to stay strong, healthy, and in control.



Molly Silvernale
It’s funny-how we’ve been taught to chase numbers like they’re holy grails, when the body’s whispering the truth all along… You don’t need a heart rate monitor to know you’re tired-you need silence, and breath, and the courage to slow down. Beta-blockers didn’t break me; they forced me to listen. And honestly? I’m better for it.
Ken Porter
This post is pure garbage. If you’re too lazy to push through, don’t blame the medicine. I’ve been on beta-blockers for 12 years and I still run marathons. Stop making excuses and get back to work.
Manish Kumar
You know, in Indian philosophy, we say that the body is not a machine to be optimized, but a temple to be honored. Beta-blockers are not enemies-they are guardians. They are the quiet voice of your heart saying, ‘Go slower, breathe deeper, live longer.’ The modern world worships speed, but true strength lies in patience. I used to think I had to sweat like a man possessed to prove I was alive-now I walk, I feel the wind, I count my breaths, and I am more alive than ever. The RPE scale? That’s not a tool-it’s a meditation.
Donny Airlangga
I’ve been on metoprolol for three years. I used to think I was failing until I read this. The talk test changed everything. I go for walks now, not runs. I don’t check my watch. I just listen. And you know what? I sleep better, I’m less anxious, and I actually enjoy movement again. Thank you for saying what so many of us feel but never hear.
Lois Li
Thank you for writing this. I’m 68 and on atenolol after a stent. I thought I was just getting old. Turns out I just needed to stop comparing myself to my 40-year-old self. I walk 40 minutes every morning now. No tracker. Just me, the birds, and my breath. I don’t need to be fast anymore. I just need to be here.
christy lianto
Ken, you’re not helping. This isn’t about laziness-it’s about biology. If you’ve been on the same dose for 12 years and still run marathons, great for you. But most of us aren’t you. We’re trying to survive, not compete. This post saves lives. Shut up and read it.
swati Thounaojam
Walk more. Run less. Listen. That’s it.
Annette Robinson
One thing I wish more doctors told patients: You don’t lose fitness when you slow down-you redefine it. I’ve coached cardiac rehab patients for 15 years. The ones who embrace RPE and talk test? They stick with it. The ones who fight it? They quit. Your heart doesn’t care about your pace. It cares that you show up. Keep showing up.
Prakash Sharma
USA is soft. In India, we run with fever, with hunger, with pain. This post is for people who think a 10-minute walk is ‘exercise.’ You want strength? Train harder. Not slower.
Kristina Felixita
Prakash, I hear you-but not everyone has the same body, the same history, the same privilege. My mom had a heart attack at 59. She’s on beta-blockers now. She walks 20 minutes a day. She smiles. She lives. That’s not weakness-that’s wisdom. And if you can’t see that, maybe you need to sit down… and listen.