Eye Inflammation & Allergies: Complete Guide to Symptoms, Causes, and Treatments

Allergic Eye Inflammation Symptom Checker
Red, Watery Eyes
Redness and watery discharge are common signs of allergic eye inflammation.
Itching & Tearing
Intense itching and excessive tearing often accompany allergic reactions.
Select your symptoms and click "Check My Symptoms" to get personalized guidance.
Ever woken up with red, itchy eyes and wondered if it’s just a harmless irritation or something that needs medical attention? eye inflammation is a common complaint, especially when allergies are in play. This guide breaks down what’s happening behind those uncomfortable symptoms, how to tell the difference between an allergy flare‑up and an infection, and what you can do right now to feel better.
TL;DR
- Eye inflammation caused by allergies usually shows redness, itching, and watery discharge.
- Key types include allergic conjunctivitis, blepharitis, and dry‑eye‑related inflammation.
- Identify triggers, use antihistamine or mast‑cell‑stabilizing drops, and keep eyelids clean.
- Seek a doctor if pain, vision change, or thick pus appear.
- Prevention: air filters, sunglasses, and regular eyelid hygiene.
What Exactly Is Eye Inflammation?
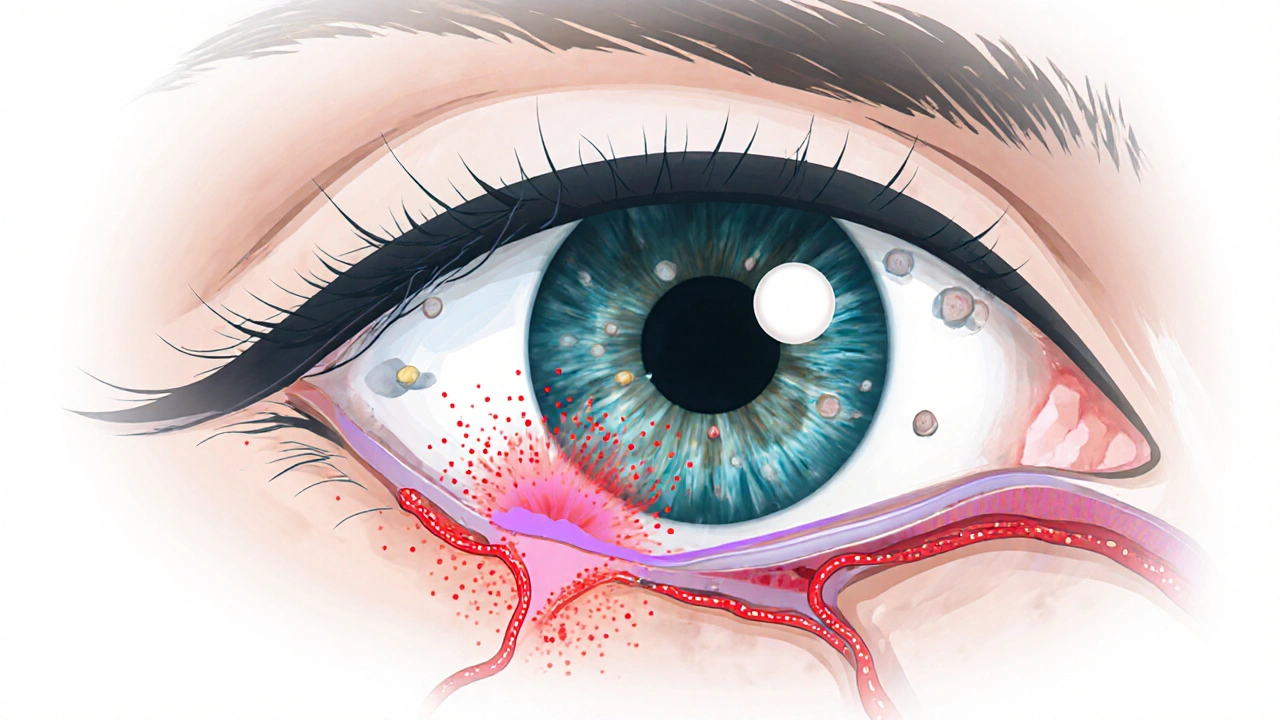
Eye inflammation refers to swelling, redness, and irritation of the ocular surface or its surrounding structures. It can involve the conjunctiva (the thin membrane covering the white of the eye), the eyelid margins, or even the tear film. While infections, trauma, and systemic disease can all cause inflammation, allergens are a top culprit for many people, especially during pollen season.
Allergies and the Eye: How They Connect
When an allergen-like pollen, pet dander, or mold spores-lands on the eye, it triggers the immune system to release Histamine and other inflammatory mediators. Histamine makes tiny blood vessels expand, leading to that classic red “bloodshot” look. It also stimulates the nerves, causing itching and tearing.
Two specialized cells play a starring role: Mast Cells. These cells sit right on the ocular surface and, once activated by an allergen, release a burst of histamine, leukotrienes, and prostaglandins-each contributing to swelling and discomfort.
Common Types of Allergic Eye Inflammation
- Allergic Conjunctivitis: The most frequent allergic eye condition. It shows as redness, itching, and a watery discharge that may look like clear mucus.
- Blepharitis: Inflammation of the eyelid margins, often worsened by an allergic response. Symptoms include crusty eyelashes, gritty feeling, and chronic redness.
- Dry Eye Syndrome with an allergic component: Low tear production or poor tear quality can amplify allergic reactions, leading to burning and redness.
Spotting the Signs: Symptoms Checklist
Knowing what to look for helps you decide whether home care will suffice or a clinician’s eye is needed.
- Redness that starts at the white (sclera) and spreads outward.
- Intense itching-often described as “the urge to scratch the eye.”
- Watery or mucoid discharge (clear or slightly cloudy).
- Swelling of the eyelids or the conjunctiva.
- Gritty or burning sensation, especially after exposure to wind or smoke.
- Blurred vision that clears quickly after blinking (common in dry‑eye‑related inflammation).
When to See a Professional
If any of the following appear, it’s time to schedule an eye exam:
- Severe pain or a feeling of something stuck under the eyelid.
- Thick, yellow or green discharge-signs of bacterial infection.
- Sudden vision loss or double vision.
- Symptoms persisting beyond two weeks despite over‑the‑counter treatment.
Eye doctors may perform a slit‑lamp exam, fluorescein staining, or tear‑film break‑up time test to pinpoint the cause.
Treatment Options: From Quick Relief to Long‑Term Management
Therapy typically follows a three‑step hierarchy: avoid the trigger, use targeted medication, and adopt lifestyle habits.
1. Allergen Avoidance
Even before opening a bottle of drops, reducing exposure can cut the inflammatory cascade.
- Keep windows closed on high‑pollen days; use HEPA filters.
- Wear wrap‑around sunglasses outdoors to shield eyes from airborne particles.
- Shower and change clothes after sports or gardening.
2. Pharmacologic Relief
Here’s where the specialized eye drops come in. The first line is usually Antihistamine Eye Drops. They block histamine receptors, easing itching within minutes.
For longer‑lasting control, many clinicians recommend Mast‑Cell Stabilizers (e.g., cromolyn sodium). These need a few days of twice‑daily use but prevent the release of histamine in the first place.
When inflammation is severe or doesn’t respond to the above, a short course of Steroid Eye Drops may be prescribed. They suppress the whole immune response but are limited to 1‑2 weeks to avoid cataract or pressure‑related glaucoma.
Oral antihistamines (loratadine, cetirizine) can complement drops, especially when systemic allergy symptoms like sneezing or a runny nose are also present.
3. Home and Lifestyle Strategies
- Warm compresses for 5‑10 minutes twice a day can loosen crusts in blepharitis.
- Gentle lid scrubs using diluted baby shampoo or commercial lid‑cleanser wipes keep bacterial overgrowth at bay.
- Artificial tears (preservative‑free) dilute allergens and improve tear film stability.
- Omega‑3 supplements (fish oil) have shown modest benefits for dry‑eye‑related inflammation.
Quick Comparison of Major Allergic Eye Conditions
| Condition | Primary Cause | Key Symptoms | First‑Line Treatment | Typical Duration |
|---|---|---|---|---|
| Allergic Conjunctivitis | Pollen, dust mites, animal dander | Redness, itching, watery discharge | Antihistamine eye drops | Hours to weeks (seasonal) |
| Blepharitis | Staphylococcal overgrowth, meibomian gland dysfunction, allergic component | Crusty lashes, eyelid swelling, gritty feeling | Lid hygiene + topical antibiotics or steroid drops if severe | Chronic, flare‑ups weeks‑months |
| Dry‑Eye‑Related Inflammation | Reduced tear production, poor tear quality, environmental irritants | Burning, blurry vision, mild redness | Artificial tears + anti‑inflammatory omega‑3s | Variable; often chronic |
| Viral Conjunctivitis (non‑allergic) | Adenovirus, enterovirus | Watery discharge, gritty sensation, often starts in one eye | Supportive care; antiviral meds only in severe cases | 7‑14 days |
| Bacterial Conjunctivitis (non‑allergic) | Staphylococcus, Haemophilus, Streptococcus | Thick yellow/green discharge, crusting | Topical antibiotics | 5‑7 days |
Preventive Checklist - Keep Allergic Flare‑Ups at Bay
- Check daily pollen counts; limit outdoor time when levels are high.
- Use air purifiers with HEPA filters in bedroom and living area.
- Keep pets out of the bedroom; wash their bedding weekly.
- Replace eye makeup every three months; avoid sharing cosmetics.
- Schedule regular lid hygiene sessions-especially if you have blepharitis.
- Carry a small bottle of preservative‑free artificial tears for quick relief.
- Visit an optometrist yearly for baseline eye health assessment.
What to Expect During a Clinical Visit
A typical appointment for allergic eye inflammation includes:
- Medical history review - recent exposures, medication use, other allergies.
- Visual acuity test to ensure vision hasn’t been affected.
- Slit‑lamp examination - close‑up view of the conjunctiva, cornea, and eyelids.
- Fluorescein staining - highlights any corneal abrasions or dry‑eye spots.
- Possible allergy testing - skin prick or serum IgE testing if the trigger is unclear.
After assessment, the doctor may prescribe a regimen tailored to severity, ranging from OTC antihistamine drops to a brief steroid course.
Frequently Asked Questions
Frequently Asked Questions
Can I use over‑the‑counter eye drops for allergic conjunctivitis?
Yes, most OTC antihistamine drops (e.g., ketotifen, olopatadine) work well for mild to moderate symptoms. If relief isn’t fast enough, a prescription mast‑cell stabilizer can be added.
Are steroid eye drops safe for long‑term use?
Steroid drops are powerful but carry risks like increased intra‑ocular pressure, cataract formation, and infection. They’re typically limited to 1‑2 weeks and only under close supervision.
How do I differentiate between allergic and viral conjunctivitis?
Allergic conjunctivitis usually produces intense itching, clear watery discharge, and both eyes are affected simultaneously. Viral conjunctivitis often starts in one eye, spreads to the other, and has a thicker, sometimes stringy discharge without itching.
Can diet help reduce eye allergies?
Foods rich in omega‑3 fatty acids (salmon, flaxseed) and antioxidants (vitamin C, lutein) support a healthier tear film and can dampen inflammation. However, diet alone won’t replace proper eye‑care measures.
Is it okay to wear contact lenses during an allergy flare?
It’s best to switch to glasses until symptoms subside. Contacts can trap allergens against the cornea, worsening irritation and increasing infection risk.
Bottom Line
Understanding how allergens spark eye inflammation empowers you to act fast-whether that means grabbing a drop of antihistamine, cleaning your lids, or seeing a specialist. By combining trigger avoidance, targeted medication, and consistent eye‑care habits, most people keep allergic flare‑ups under control and protect their vision for the long haul.



Patrick Culliton
Honestly, most of these “expert” tips are just marketing fluff – you don’t need a whole checklist to stop an itchy eye.
Andrea Smith
While I understand your skepticism, the evidence supporting proper lid hygiene and allergen avoidance is quite robust, and adhering to these measures can significantly reduce symptom severity.
Gary O'Connor
hey, i tried the warm compress thing and it actually helped with the crusty lashes, kinda surprised myself lol.
Justin Stanus
There’s a certain melancholy in watching someone scratch their eyes incessantly, as if the world’s tiny particles have become personal demons.
Claire Mahony
Overall the guide is solid, but the recommendation to use steroid drops without emphasizing the need for ophthalmic supervision feels risky.
Andrea Jacobsen
I agree with Claire; a brief reminder that steroids should only be prescribed after a thorough exam would make this piece even better.
Andrew Irwin
Let’s keep the conversation respectful – everyone’s experience with eye allergies is different, and sharing tips helps us all.
Jen R
Cool guide, but I think most people will just skip the table and grab whatever drop is on sale.
Joseph Kloss
When one contemplates the ocular surface, one must first acknowledge that the eye is not merely a passive canvas for allergens but a dynamic interface orchestrating immunological symphonies. The conjunctiva’s mast cells, upon encountering pollen, release histamine in a cascade that mirrors the philosophical concept of causality – a cause giving rise to effect, effect swirling back to influence cause. This feedback loop, while biologically essential, manifests as redness, itching, and lacrimation, which the layperson merely labels “eye irritation". Yet there is a deeper ontological question: does the experience of itch provoke a purely physiological reflex, or does it also invoke an existential dread of bodily betrayal? In clinical practice, we observe that antihistamine drops provide quick relief, akin to a Socratic dialectic that dispels confusion with concise answers. Mast-cell stabilizers, however, require patience, reminiscent of Aristotle’s golden mean, balancing immediate comfort against long‑term equilibrium. Moreover, the role of environmental control – air filters, HEPA systems, seasonal awareness – parallels the Stoic notion of premeditatio malorum, preparing oneself against foreseeable misfortune. The guide’s emphasis on compresses and lid hygiene is not merely a mechanical recommendation; it is, in fact, an embodiment of the body‑mind unity espoused by Eastern philosophies where smooth circulation mirrors mental clarity. One must not overlook the psychological facet: chronic itching can erode patience, leading to an irritability that echoes the ancient Greek concept of thumos, the spirited part of the soul. Consequently, the prescription of preservative‑free artificial tears is not simply pharmacology but a ritual of self‑care, restoring the tear film’s delicate balance as one would tend to a garden. Finally, the admonition to seek professional evaluation when symptoms persist invokes the principle of epistemic humility, acknowledging that the practitioner’s slit‑lamp examination can uncover hidden pathologies beyond mere allergies. In summation, eye inflammation is a microcosm of broader systemic interactions, and treating it demands an integrative approach that honors both the corporeal and the metaphysical dimensions.
Anna Cappelletti
Great summary! Your friendly tone really makes the information feel accessible.
Dylan Mitchell
Oh, the drama of red eyes! It’s like a theatrical tragedy where the stage is your cornea and the protagonist-your poor, besieged eyelid-is forever battling the villainous pollen. I mean, really, who decided that nature should sprinkle microscopic irritants like confetti at a parade? The swelling, the itching, the endless stream of tears-each symptom a melodramatic monologue demanding applause. And yet, the audience (that’s us, the sufferers) is forced to sit through endless intermissions of cold compresses and lid scrubs, like cheap stand‑up jokes that fall flat. Let’s not even get started on the “preservative‑free artificial tears”-the starring hero who swoops in, caped in sterile saline, only to disappear after a fleeting cameo. The whole guide reads like a soap opera script: *Cue the eye doctor, enter the steroid drops, climax of relief, fade to black.* Honestly, if allergies were a genre, they’d be horror: you never see the monster coming, but when it hits, you’re screaming, “Not again!” And the chorus of “avoid triggers!” is the relentless, ominous soundtrack that haunts every outdoor adventure. So, dear readers, grab your cheap sunglasses, your cheap eye drops, and brace for the next act-because the curtain never truly falls on this ocular saga.
Elle Trent
While the guide is comprehensive, the jargon about mast‑cell stabilizers could be simplified for lay readers.
Jessica Gentle
Hey everyone! If you’re looking for an easy way to keep symptoms at bay, start with a daily lid‑hygiene routine: mix a few drops of baby shampoo with warm water, gently massage the lash line, and rinse. Pair that with preservative‑free artificial tears a few times a day, especially after exposure to wind or screens. For acute itch, over‑the‑counter antihistamine drops like ketotifen work within minutes. Remember, consistency is key-skipping a day can let inflammation rebound. If you notice any pus, pain, or vision changes, schedule an appointment right away. Feel free to ask if you need product recommendations!
Samson Tobias
Don’t let allergies steal your confidence – a few minutes of eye care each morning can keep those red, itchy windows on your face closed for good.
Alan Larkin
Interesting read! I’d add that a proper shield against pollen is a pair of wrap‑around sunglasses – they’re not just a fashion statement, they’re a functional barrier. 😎
John Chapman
One might argue that the guide, while thorough, glosses over the nuanced pharmacokinetics of corticosteroid ophthalmic preparations, thereby under‑informing the discerning reader.
Tiarna Mitchell-Heath
Enough with the polite suggestions – if you’re allergic, stop ignoring the problem and start using those drops NOW, not tomorrow.
Katie Jenkins
While many contributors have provided valuable insights, it’s essential to remember that not every recommendation applies universally; individual variations in tear film composition and allergen exposure levels necessitate personalized treatment plans, and therefore, a one‑size‑fits‑all approach is inadvisable.