How to Use a Pill Organizer Safely Without Overdosing: Step-by-Step Safety Guide
Using a pill organizer seems simple-just dump your meds into little compartments and go. But if you’re not careful, it can turn into a dangerous routine. In fact, a 2022 study in the Journal of the American Geriatrics Society found that improper use of pill organizers increases overdose risk by 23% in older adults. That’s not a small number. It’s not a hypothetical. It’s happening in kitchens, bathrooms, and bedrooms across the country every day.
Why Pill Organizers Can Be Risky
Pill organizers work great when used right. They help you remember doses, reduce missed medications, and cut down on accidental doubles. Memorial Sloan Kettering Cancer Center reports that people who use them correctly see a 32% drop in missed doses and an 18% drop in double-dosing. But here’s the catch: if you fill them wrong, they become a hazard. Most people don’t realize that not all pills belong in organizers. Liquid medications, chewables, dissolvable tablets, and soft gel capsules can stick together, break down, or lose potency. Refrigerated drugs like insulin or certain antibiotics? Never put those in a pill box. The heat and humidity from your bathroom or kitchen counter can ruin them. Kaiser Permanente warns that storing pills in a bathroom organizer can speed up degradation by 47% because of steam from showers. And then there’s the biggest mistake of all: putting "as needed" (PRN) meds in your daily compartments. That’s like putting a firecracker in your toolbox and forgetting it’s there. Someone takes their painkiller because they’re scheduled for it at 8 a.m.-but then they take another at noon because their knee hurts again. That’s how overdoses happen. WebMD and Memorial Sloan Kettering both say 38% of accidental overdoses from pill organizers come from mixing PRN meds with scheduled ones.What Kind of Organizer Should You Use?
Not all pill boxes are made the same. A basic weekly organizer with one compartment per day costs under $10. But if you take meds four times a day, you need a 7-day x 4-compartment model-those run $5 to $15. For people who forget doses or live alone, electronic organizers with alarms cost $25 to $100. Some even send alerts to caregivers’ phones. Look for these safety features:- Child-resistant lids (must meet ASTM F3130-15 standards)
- Clear, bold labels for AM, PM, bedtime, or specific times
- Braille or tactile markings for low vision
- Moisture-resistant plastic (not flimsy, cheap plastic that cracks)
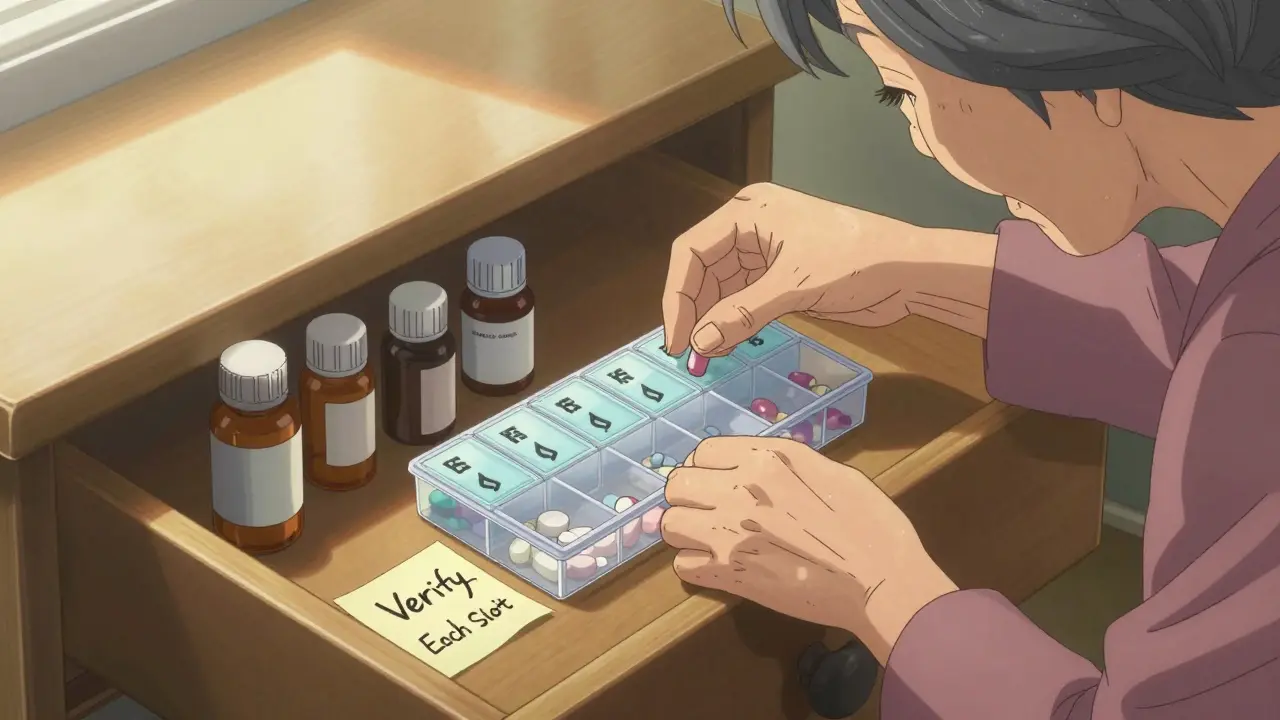
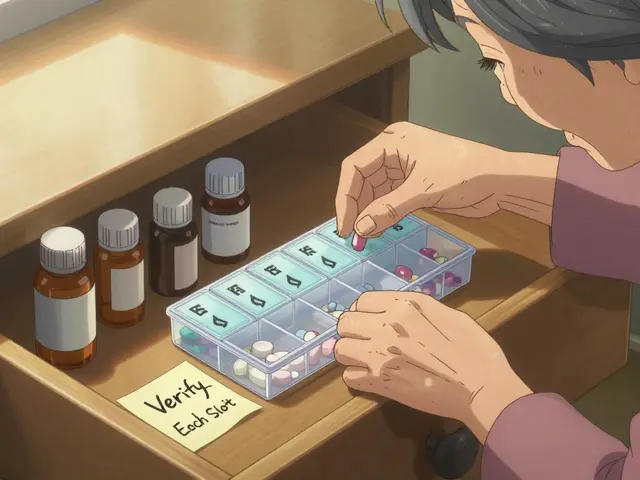
The Five-Step Filling Protocol (No Exceptions)
This isn’t a suggestion. This is the standard used by pharmacists and hospitals. Skip one step, and you’re rolling the dice.- Get your current medication list-not the old one from last month. Check with your pharmacy or doctor. If you’ve added, stopped, or changed a dose, your organizer must reflect that. WebMD says 28% of errors happen when people refill using outdated labels.
- Wash your hands for 20 seconds. Use soap. Dry them. You’re handling medicine, not laundry.
- Keep original bottles out and within sight. Don’t stash them away. Every time you pick up a pill, compare it to the bottle label. Same name. Same dose. Same instructions.
- Fill one medication at a time. Not all at once. Fill all Monday AM doses for all meds first. Then Tuesday AM. Then Wednesday AM. This forces you to focus. Dr. Jane Smith, Chief Pharmacist at Memorial Sloan Kettering, says this reduces double-dosing errors by 63%.
- Verify each compartment. Before you close the lid, look at every slot. Is that the right pill? Is it the right dose? Is it supposed to be there? 31% of overdoses happen because people didn’t check.
When to Fill Your Organizer
Don’t just grab it on a random Tuesday. Pick one day a week-Sunday morning works for most people-and stick to it. Memorial Sloan Kettering found that people who fill on the same day every week have an 87% accuracy rate. That’s because routine builds muscle memory. Set aside 15 minutes minimum. Add 5 extra minutes for every medication beyond your first five. Rushing leads to mistakes. If you’re helping someone else, do it together. Talk through each pill. Say it out loud: "This is metoprolol 25 mg, once daily, for blood pressure. Confirmed by bottle."
What to Never Put in a Pill Organizer
Some meds just don’t belong. Here’s the hard list:- PRN (as-needed) medications-painkillers, anxiety meds, nitroglycerin
- Liquid medications (they leak, mix, and spoil)
- Chewables, dissolvable tablets, or sublingual pills
- Soft gel capsules (they stick together and break open)
- Refrigerated drugs (insulin, some antibiotics, biologics)
- Medications with strict expiration dates (like epinephrine auto-injectors)
Storage Matters More Than You Think
Your organizer should live in a cool, dry place. That means not the bathroom. Not the kitchen near the stove. Not the car. The ideal spot? A drawer in your bedroom, or a shelf in your closet. Temperature should stay under 86°F (30°C) and humidity below 60%. If you live in a humid climate like Wellington, where damp air rolls in off the sea, this is even more critical. Moisture doesn’t just make pills sticky-it can break down active ingredients. Hero Health’s 2022 study showed that pills stored in humid environments lost potency up to 47% faster. Keep the original bottles nearby. Always. Even if you’ve filled the organizer, keep the bottles within arm’s reach. They’re your backup. They have the pharmacy label, expiration date, and dosage instructions. If you’re ever confused, go back to the bottle.How to Avoid Overdose Traps
Here are the top three mistakes that lead to overdoses-and how to stop them:- Mixing PRN meds with scheduled ones: Keep painkillers, sleep aids, or anti-anxiety meds in their own container. Label it clearly: "ONLY IF NEEDED." Never put them in the daily slots.
- Not updating after prescription changes: If your doctor adds a new pill or stops one, change your organizer immediately. Don’t wait. Don’t assume. Update it the same day.
- Ignoring expiration dates: Pills in organizers don’t last forever. Even if the bottle says "expires 2027," once you transfer them, the clock starts ticking. Most experts recommend refilling every 7 to 14 days. If you’re not taking the meds daily, refill weekly.

When to Ask for Help
You don’t have to do this alone. Nearly 68% of U.S. pharmacies now offer free organizer filling with pharmacist verification. Walk in with your bottles and your organizer. They’ll check everything-dosage, interactions, timing-and fill it for you. That cuts errors by 52%. If you’re caring for someone else, ask the pharmacist to explain each medication. Watch them fill it. Ask questions. If they say, "This one’s for pain," but the label says "for heart rhythm," trust the label. Don’t trust the memory. And if you’re ever unsure-call your pharmacist. No question is too small. A quick 5-minute call can prevent a hospital visit.What’s Next for Pill Organizer Safety
Technology is catching up. New smart organizers track when compartments are opened. If someone opens the morning dose twice in three hours, it sends an alert. Some even weigh the pills to make sure the right amount was taken. Pfizer is testing QR codes on lids that link to short videos explaining each med. Medicare now covers smart organizers for people with four or more chronic conditions. That’s a big step. But for now, the safest tool is still the one you use correctly: a simple organizer, filled slowly, verified twice, and stored right.Final Checklist: Your Safety Routine
Before you close your organizer, ask yourself:- Did I use my current medication list, not an old one?
- Did I wash my hands before handling pills?
- Did I keep the original bottles out while filling?
- Did I fill one medication at a time?
- Did I check each compartment visually?
- Did I avoid PRN meds in daily slots?
- Is my organizer stored away from heat and humidity?
- Did I refill it on the same day this week?
Can I put all my pills in one organizer?
No-not all of them. Avoid putting liquid medications, chewables, soft gels, refrigerated drugs, or "as needed" pills in organizers. Only solid, stable oral medications that are taken on a fixed schedule belong in a pill box. Always check with your pharmacist before transferring any medication.
How often should I refill my pill organizer?
Refill weekly for most people. If you take meds daily, refill every 7 days. If you only take some pills a few times a week, refill every 7 to 14 days. Never fill more than 30 days ahead, even if your prescription lasts longer. Pills can degrade, and your regimen might change.
Is it safe to store a pill organizer in the bathroom?
No. Bathrooms are too humid. Steam from showers can damage pills, making them sticky, crumbly, or less effective. Store your organizer in a cool, dry place like a bedroom drawer or closet. Kaiser Permanente and Hero Health both warn against bathroom storage.
What should I do if I accidentally take a double dose?
Call your pharmacist or doctor immediately. Don’t wait for symptoms. Even if you feel fine, some medications build up in your system. Keep your medication list and organizer handy so you can tell them exactly what you took and when. In emergencies, call Poison Control or go to the nearest emergency room.
Can children get into my pill organizer?
Yes-if it’s not child-resistant. Always choose organizers with safety locks that meet ASTM F3130-15 standards. Store the organizer out of reach and sight of children-even if you think it’s "just a few pills." Accidental ingestion is one of the top causes of pediatric poisonings.
Are electronic pill organizers worth the cost?
If you forget doses, live alone, or take complex medications, yes. Alarms, refill reminders, and caregiver alerts can prevent missed or double doses. Medicare may cover them if you have four or more chronic conditions. Even basic models with alarms cost under $30 and can save your life.



Lauren Warner
People think these organizers are magic boxes, but they’re just plastic trays with delusions of grandeur. If you don’t follow the five-step protocol, you’re not organizing-you’re gambling with your liver, your kidneys, your brain. The 23% overdose increase isn’t a statistic-it’s your neighbor, your aunt, your dad. Stop treating meds like cereal.
Craig Wright
The assertion that pill organizers increase overdose risk is misleading. In the UK, such devices are regulated under the Medical Devices Regulations 2002, and their use is embedded within clinical protocols. The real issue is lack of pharmacist oversight, not the organizer itself. This article reads like fearmongering disguised as public health advice.
Lelia Battle
There’s something deeply human about the way we try to impose order on chaos-like filling a pill organizer on Sunday morning, ritualistically, like a prayer. We want to believe that if we arrange these little tablets just right, we can control time, biology, mortality. But the truth is, we’re just trying to remember to be kind to ourselves, one pill at a time.
Darryl Perry
Stop wasting time with organizers. Just use a pill bottle with a daily alarm on your phone. Simpler, cheaper, no risk of mixing meds.
Jose Mecanico
I’ve been using one for five years. Always refill on Sundays. Never put PRN meds in. Keep bottles next to it. It’s not hard. Just don’t rush it.
George Bridges
My mom used one after her stroke. We filled it together every Sunday. She’d say each pill out loud: ‘This is for blood pressure. This is for the heart.’ It wasn’t just about safety-it was about dignity. She felt in control again.
gary ysturiz
You got this. Taking your meds on time is one of the most powerful things you can do for your future self. Don’t let fear stop you-just follow the steps. Sunday morning, wash your hands, check the bottle. You’re doing better than you think.
Jessica Bnouzalim
OMG YES. I used to toss my anxiety meds in there with my blood pressure pills… until I took two at once and felt like I was going to pass out. Now they’re in a separate red container with a big label: "ONLY IF I’M PANICKING." LIFE SAVER.
Sumit Sharma
The 47% degradation rate in humid environments is corroborated by WHO’s 2021 stability guidelines for solid oral dosage forms under accelerated storage conditions (ICH Q1A). Furthermore, the ASTM F3130-15 compliance threshold is non-negotiable in clinical pharmacy practice. Non-compliance constitutes a Class II recall risk under FDA 21 CFR 808.36.
Katherine Carlock
My grandma’s organizer is in her bedroom drawer, labeled in big letters. She even has a sticky note on the fridge: "Did you check the bottle?" We laugh about it now, but it saved her life. You don’t need fancy tech-just consistency and a little love.
beth cordell
❤️❤️❤️ This is the kind of post that makes me cry. My dad passed last year because he mixed his nitroglycerin with his daily pills. I wish I’d seen this sooner. Thank you for writing this. Sharing everywhere.
Daniel Pate
If the organizer is a tool, then the real question is: who controls the tool? The patient? The pharmacist? The algorithm? Or the system that forces people to manage complex regimens alone? We’re treating symptoms, not the structural failure of healthcare access. A pill box won’t fix a broken system.