Pediatric Dosing: Weight-Based Calculations and Double-Checks for Safer Medication Use

Getting the right dose of medicine for a child isn’t just about following a prescription. It’s about weight-based calculations-and making sure no step gets skipped. A child’s body isn’t a small adult. Their organs, metabolism, and fluid balance work differently. That’s why guessing a dose by age or using adult formulas can be dangerous. In fact, medication errors in kids are one of the leading causes of preventable harm in hospitals. The solution? Precise, weight-based dosing, backed by a second set of eyes.
Why Weight Matters More Than Age
For decades, doctors used age-based dosing for kids. It was simple: give a toddler half the adult dose. But that approach is outdated-and risky. A 10-pound premature infant and a 60-pound 8-year-old are both "toddlers," but their bodies process drugs in completely different ways. Research from the Pediatrics journal in 2022 showed that weight-based dosing cuts medication errors by 43% compared to age-based estimates. Why? Because it accounts for actual body size, not just birthday candles.Body weight directly affects how much medicine stays in the bloodstream. Neonates have about 75% water in their bodies-compared to 60% in adults-so water-soluble drugs like amoxicillin spread differently. Kids with obesity need special consideration too. Their fat stores can trap lipophilic drugs, while their liver and kidneys might not be mature enough to clear them. That’s why modern protocols don’t just use total weight-they sometimes use adjusted or ideal body weight, depending on the drug.
How Weight-Based Dosing Works: The Three-Step Formula
There’s a clear, repeatable method used in nearly every children’s hospital today. It’s not complicated, but it must be followed exactly.- Convert pounds to kilograms-exactly. Use the conversion: 1 kg = 2.2 lb. Never round until the final answer. A child weighing 44 pounds is exactly 20 kg (44 ÷ 2.2). Round too early, and you throw off everything after.
- Multiply weight in kg by the prescribed dose per kg. If the order says 15 mg/kg/day for amoxicillin, and the child weighs 20 kg, the total daily dose is 300 mg (20 × 15).
- Divide by frequency. If it’s given twice a day, each dose is 150 mg (300 ÷ 2).
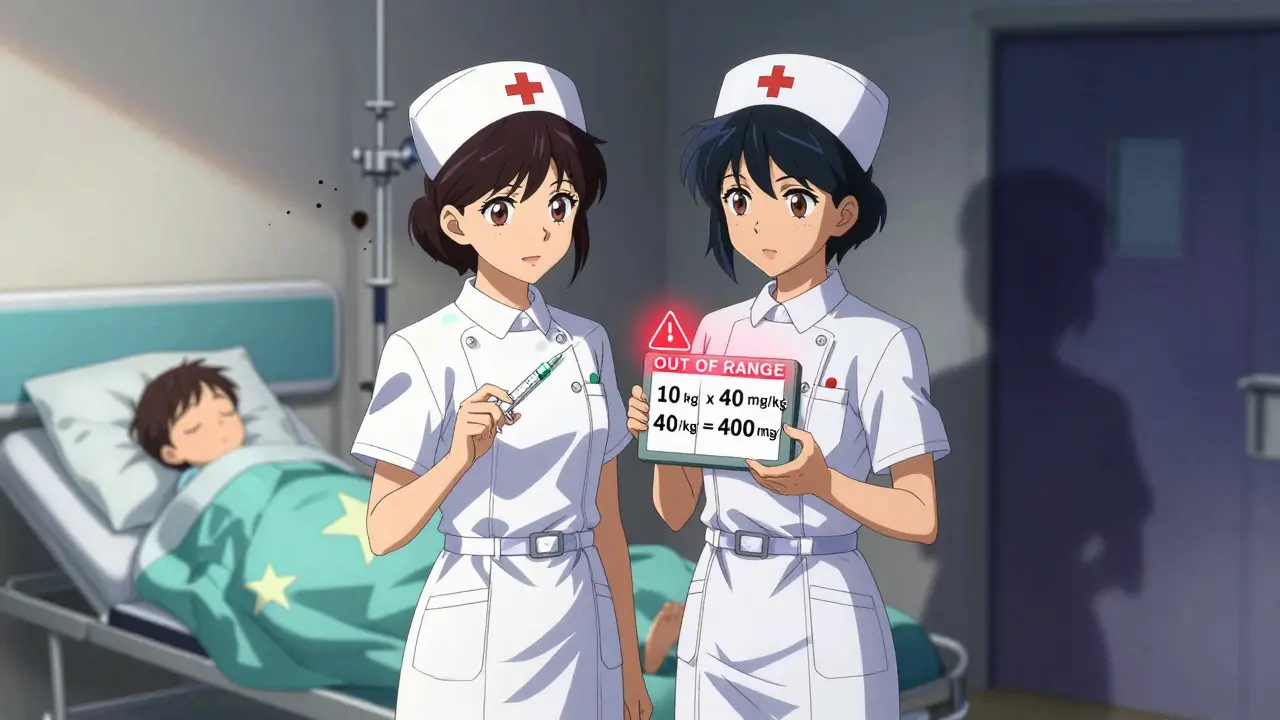
Let’s say a 22-pound child (10 kg) is prescribed 40 mg/kg/day of amoxicillin, divided into two doses. Total daily dose: 400 mg. Each dose: 200 mg. Simple. But only if the weight is accurate and the math is done right.
When Weight Isn’t Enough: Body Surface Area and Special Cases
For some drugs-especially chemotherapy-weight alone isn’t precise enough. That’s where Body Surface Area (BSA) comes in. The Mosteller formula: √(weight in kg × height in cm ÷ 3600) gives a more accurate picture of how the drug will distribute. A 2021 study found BSA dosing improves accuracy by 18% for cancer drugs. But it takes longer: about 47 extra seconds per dose. That’s why it’s reserved for high-risk meds.For obese children, things get trickier. The Pediatric Endocrine Society recommends using adjusted body weight for certain drugs: Ideal Body Weight + 0.4 × (Actual Weight - Ideal Body Weight). This prevents overdosing on drugs that don’t distribute well in fat tissue. About 78% of children’s hospitals now follow this for specific medications like antibiotics or seizure drugs.
The Double-Check: Your Last Line of Defense
Even the best calculator can be fooled by a misplaced decimal or a misread scale. That’s why every children’s hospital requires a double-check for high-alert medications. This isn’t optional. It’s a National Patient Safety Goal from The Joint Commission.Here’s how it works in practice:
- One nurse calculates the dose based on the child’s weight.
- A second nurse independently recalculates it-using the same formula, same scale, same order.
- They compare results. If they don’t match, they stop. No exceptions.
In 2023, a nurse in Colorado caught a 10-fold overdose because the second checker noticed the dose exceeded the maximum safe limit of 40 mg/kg/day. The child was 10 kg-the prescribed dose was 200 mg instead of 20 mg. That’s a life-threatening error. The double-check saved them.
Where Things Go Wrong: The Top 3 Errors
Despite protocols, mistakes still happen. The Institute for Safe Medication Practices tracked over 1,200 pediatric dosing errors in 2022. The biggest culprits?- Unit confusion-38% of errors. A scale reads pounds, but the order is in kg. Some hospitals now put bright red stickers on all scales: "WEIGH IN KG ONLY."
- Decimal errors-27%. Writing 1.0 mg instead of 10 mg. Or misreading 0.5 as 5.0. Electronic systems now flag doses that fall outside expected ranges.
- Ignoring kidney or liver function-19%. A child with renal impairment might need half the dose-even if their weight says otherwise. Neonates and preterm infants often need 40-60% reductions for drugs like aminoglycosides.
One nurse on Reddit shared that she saw three near-misses in one year from using pounds instead of kilograms. Now her hospital requires weight to be documented in kg before any medication is prepared.

Technology Is Helping-But Not Replacing People
Epic Systems and other EHR vendors added pediatric dosing modules in 2023. These tools auto-calculate doses, flag out-of-range amounts, and lock in weight in kg. Over 78% of children’s hospitals now use them. But here’s the catch: technology can’t replace a second pair of eyes.A 2023 study at UCSF Medical Center found that adding a "dose range alert" reduced errors by 52%. But even with alerts, 15% of errors still happened because staff overrode the system without double-checking. The best tech is useless if the culture doesn’t demand verification.
What You Need to Know: Key Takeaways
- Weight-based dosing (mg/kg) is the standard for 87% of pediatric medications.
- Always convert pounds to kilograms using 1 kg = 2.2 lb-round only at the end.
- Double-checks by two qualified staff members are mandatory for high-alert drugs.
- For obese kids, use adjusted body weight for some drugs-don’t rely on total weight.
- Neonates and infants under 6 months often need lower doses due to immature organs.
- Technology helps, but human verification is irreplaceable.
Medication safety for children isn’t about being perfect. It’s about building layers of protection. One mistake can be fatal. But with the right formula and a disciplined double-check, you can make sure it never happens on your watch.
Why can’t I just use age to dose a child’s medication?
Age-based dosing ignores how a child’s body actually processes medicine. Two children of the same age can weigh very differently, and their metabolism, organ function, and body water content vary. Studies show age-based dosing has a 29% error rate for kids at growth extremes. Weight-based dosing reduces errors by 43% because it matches the dose to the child’s actual physiology.
What’s the correct way to convert pounds to kilograms for dosing?
Use the exact conversion: 1 kg = 2.2 lb. Divide the weight in pounds by 2.2. Do not round the result until after you’ve completed all calculations. For example, a 33-pound child is 15 kg (33 ÷ 2.2 = 15), not 15.05 or 14.9. Rounding too early can cause cumulative errors that lead to overdosing.
Do all children’s hospitals use double-checks for medication?
All children’s hospitals accredited by The Joint Commission are required to use independent double-checks for high-alert medications. Compliance is 94% in children’s hospitals, but only 68% in community emergency departments. The practice is non-negotiable in pediatric settings because the margin for error is so small.
What if a child is overweight or obese?
For water-soluble drugs (like antibiotics), use ideal body weight. For fat-soluble drugs (like some seizure meds), use actual body weight. For many others, use adjusted body weight: Ideal Body Weight + 0.4 × (Actual Weight - Ideal Body Weight). This prevents overdosing by accounting for excess fat tissue that doesn’t affect drug distribution the same way as lean mass.
Are electronic systems enough to prevent dosing errors?
No. While EHR systems with built-in dose alerts reduce errors by up to 52%, they don’t eliminate human error. Staff can override alerts, misenter weight, or ignore warnings. The most effective systems combine automated calculations with mandatory double-checks by two trained professionals. Technology supports safety-it doesn’t replace it.
Why do newborns need lower doses even if they weigh the same as older infants?
A newborn’s liver and kidneys aren’t fully developed. They clear drugs like aminoglycosides and sedatives much slower than older babies-even if they weigh the same. For example, preterm infants may need 40-60% lower doses of certain antibiotics. Weight tells you how much drug to give-but developmental stage tells you how fast it will be cleared. Both matter.



Jeanette Jeffrey
Oh wow, another ‘weight-based dosing’ holy text. Let me guess-next you’ll tell us not to use our hands to hold babies? 🙄
Joanne Smith
God bless the nurse in Colorado who caught that 10x overdose. Honestly? That’s the kind of hero we don’t celebrate enough. I’ve seen people override alerts because ‘it’s just a decimal’-and then we get the ‘why didn’t anyone check?’ calls at 3 AM. 🙏
Also, the ‘red sticker on scales’ thing? Genius. I work in a rural ED where someone once dosed a 5-pound preemie with 500mg of amoxicillin because the scale read ‘11’ and they thought it was kg. We had to call poison control. Don’t laugh-it happened.
Prasanthi Kontemukkala
This is such an important reminder for all of us in healthcare. I’ve trained nurses in India where resources are limited, and we often rely on age-based dosing out of necessity. But even with limited tools, we can still double-check, write weights clearly, and pause before administering. Small steps matter.
Thank you for sharing the formulas-this is exactly what we need to make safe care accessible everywhere, not just in fancy hospitals.
Bryan Woods
While the weight-based approach is clearly superior, I would caution against over-reliance on the Mosteller formula for BSA in pediatric oncology. The formula assumes normal body composition, which is often not the case in malnourished or obese children. Some institutions now use predictive algorithms incorporating lean mass-worth considering in high-risk cases.
Ryan Cheng
Love this breakdown. One thing I’d add: always write ‘kg’ after the weight in the chart. I once saw a nurse give a 200mg dose because the chart said ‘20’ and she assumed it was kg-when it was actually lbs. No one had written the unit. Simple fix. Always label.
wendy parrales fong
It’s wild how something so simple can save a life. Just convert, multiply, divide. No magic. No guesswork. Just math and care.
And yeah, double-checks aren’t about distrust-they’re about love. You’re not checking because you think they’re dumb. You’re checking because you care enough to make sure they don’t have to carry the guilt of a mistake.
Shreyash Gupta
😂 I work in a hospital where the EHR auto-converts lbs to kg… but someone typed ‘22.0’ as weight and the system read it as 220 lbs. Got flagged? Nah. Dose went out. Kid was fine. But the nurse cried for an hour.
So yeah… tech helps. But humans? Still the dumbest variable. 🤦♂️
Ellie Stretshberry
so i work in peds and i swear every time i see a new nurse they look at the weight like its a riddle
and then they just guess
and then the pharmacist calls and its like oh wait i meant 12 kg not 12 lbs
we need more stickers. like giant ones. with fire. and screaming
Angela Spagnolo
Thank you… thank you… thank you… for writing this. I’ve seen so many near-misses… and I’ve been the one who caught them… and I’ve also been the one who almost made them…
It’s not about being perfect. It’s about being careful. And that’s hard. And it’s exhausting. But it’s worth it.
Every time I double-check… I think of a child… and I breathe.
And then I do it again.
carissa projo
Let’s be real-pediatric dosing is the only place where math is a life-or-death art form. You’re not just calculating a number. You’re calculating trust.
Every time you convert pounds to kilograms, you’re saying: ‘I see you. I’m not rushing. I’m not guessing. I’m here for this child.’
And when you double-check? That’s not protocol. That’s poetry. Quiet, unglamorous, sacred poetry.
So thank you for reminding us that the most powerful tool in medicine isn’t the algorithm-it’s the human who pauses.
And then pauses again.
josue robert figueroa salazar
Stop pretending this is hard. It’s not. Just use kg. Double-check. Done.
Everything else is noise.
david jackson
Let me tell you about the time I was on call during a snowstorm, the power flickered, the EHR crashed, and we had to dose a 7-month-old with vancomycin using a paper chart, a calculator, and a flashlight…
And I did it. By hand. With a colleague. And we wrote the weight in red marker on the whiteboard. And we didn’t just double-check-we triple-checked. And then we held the child’s hand while the med infused.
And you know what? We didn’t just save a life.
We remembered that medicine is still… human.
And that’s why I still do this.
Even when the system fails.
Even when the lights go out.
Even when no one’s watching.
Jody Kennedy
THIS. THIS IS WHY I STAY IN PEDIATRICS. Not for the pay. Not for the hours. But for moments like this-where a simple math step becomes a shield. A double-check becomes a hug. A red sticker becomes a promise.
Keep sharing this. Keep fighting for the little ones. We’re the only ones who will.
christian ebongue
10kg = 22lb. 40mg/kg = 400mg. 200mg per dose. Done.
Why is this a blog post?