How to Teach Family Members to Recognize Overdose Symptoms

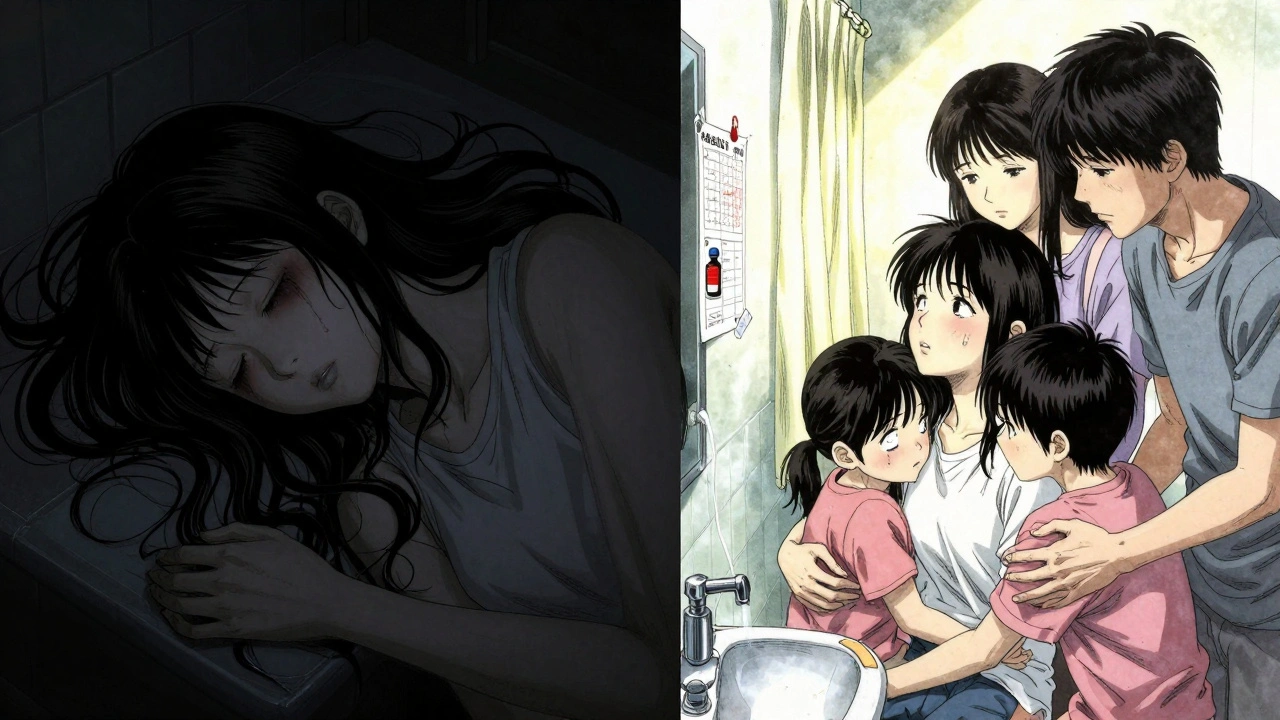
When someone you love is using drugs, you don’t wait for an emergency to learn what to do. You learn how to recognize overdose symptoms before it’s too late. Overdoses don’t always look like what you see on TV. Sometimes, it’s just a person who won’t wake up, breathing too slowly, lips turning gray. And if you don’t know what you’re seeing, you might think they’re just asleep-or high. That delay can cost them their life.
What Overdose Actually Looks Like
Overdose isn’t one thing. It changes based on the drug. But there are clear, consistent signs you can learn in minutes that apply to most cases.For opioids like heroin, fentanyl, or prescription painkillers, look for the opioid triad:
- Unresponsive: Shout their name. Shake their shoulder. Rub your knuckles hard on their sternum (center of chest). If they don’t react at all, that’s a red flag.
- Slow or stopped breathing: Watch their chest. Are they taking fewer than one breath every five seconds? Or worse-no breath at all?
- Blue or gray lips and fingernails: This is cyanosis. On lighter skin, it looks blue or purple. On darker skin, it looks grayish, ashen, or dull. Don’t wait for blue to appear-gray is just as dangerous.
Other signs include:
- Limp body-like a ragdoll
- Clammy, cold skin
- Gurgling or snoring sounds (sometimes called the "death rattle")
For stimulants like cocaine or meth, the signs are different:
- Body temperature over 104°F (40°C)-skin hot to the touch
- Seizures or twitching
- Chest pain or racing heartbeat
- Extreme confusion or paranoia
Key thing to remember: Someone who’s just high will still respond to pain or loud noise. Someone overdosing won’t. That’s the line between panic and action.
Why Family Members Are the First Responder
Most overdoses happen at home. Not in a hospital. Not on the street. In the bedroom, the living room, the bathroom. The CDC says 78% of overdose deaths occur in private residences. That means your family is often the first-and sometimes only-person who can act.Studies show that when a family member recognizes an overdose and acts fast, the chance of survival jumps by up to 40%. Why? Because time is everything. Naloxone (Narcan) can reverse an opioid overdose-if it’s given within 4 minutes of breathing stopping. EMS might take 10, 15, even 20 minutes to arrive. You don’t have to wait.
And here’s the truth: most people who overdose don’t call for help themselves. They’re too unconscious. Too scared. Too ashamed. That’s why you need to be ready-not just for them, but for yourself. You’re not enabling. You’re saving a life.
How to Teach It Without Scaring Everyone
Talking about overdose can feel heavy. Maybe someone in your family thinks it’s "jinxing" things. Maybe they’re afraid to bring it up. That’s normal. But training doesn’t have to be a somber lecture.Use the "Recognize-Respond-Revive" method-it’s used by hospitals and community programs across the U.S. and it works:
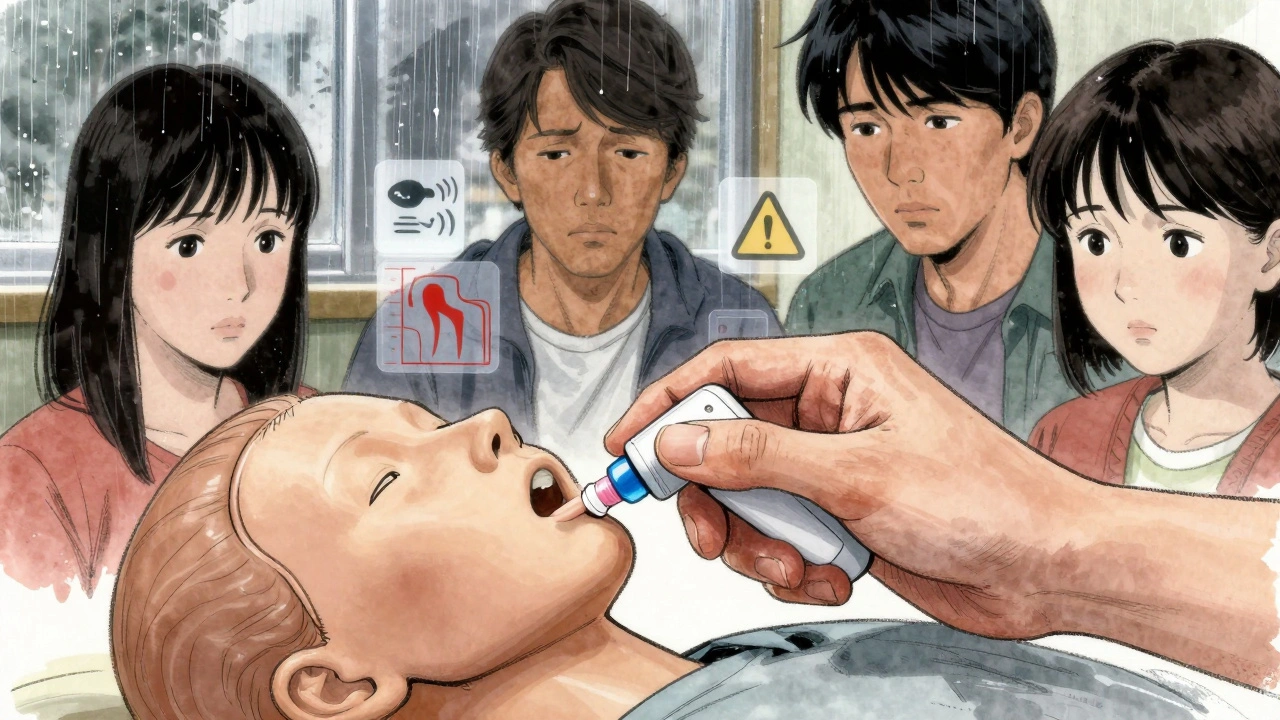
- Recognize: Practice spotting the signs using photos or videos. Show side-by-side images: someone sleeping vs. someone overdosing. Point out the difference in skin color, breathing, posture.
- Respond: Teach what to do next. Call 911. Then, give naloxone. Then, keep doing rescue breathing if they’re not breathing.
- Revive: Practice with a training naloxone device. These aren’t real drugs-they’re dummy sprays that make a clicking sound. Use them on a mannequin or even a pillow. Do it three times. Make it normal.
Keep it short. 20 minutes. One evening. After dinner. No pressure. Say: "I’m not expecting this to happen. But if it does, I want us all to know what to do. Just like knowing CPR."
Use real stories. There’s a Reddit user named RecoveryDad42 who saved his son after practicing with a training kit three times. He said: "I didn’t hesitate. I knew it was real." That’s the goal-not fear. Confidence.
What You Need to Get Started
You don’t need a medical degree. You need three things:- Training naloxone kits: These cost about $35 each. They’re the same size and shape as real Narcan nasal spray, but contain no medicine. You can get them free from many community health centers, harm reduction programs, or online through the Harm Reduction Coalition.
- Skin tone guides: Many people miss overdose signs because they’re taught to look for blue lips-but that doesn’t show up the same on darker skin. Download free color charts from the California Department of Public Health or SAMHSA. Print them. Tape one to the fridge.
- Scenario cards: Write down 5 real-life situations: "They’re snoring loudly and won’t wake up," "Their face is pale and their hands are cold," etc. Pull one out during training and ask: "What do you do?"
Some states let you get naloxone without a prescription. In 31 states, pharmacies can hand it out under a standing order. Ask your local pharmacy. If they say no, ask for the public health department. They’ll point you to free resources.
What to Do If You Suspect an Overdose
If you think someone is overdosing, here’s your step-by-step:- Shout their name and shake them. If no response, move to step two.
- Call 911 immediately. Say: "I think someone is overdosing on opioids." Even if you’re not sure, call. Better safe.
- Give naloxone. Spray one dose into one nostril. If you have a second dose and no response after 2-3 minutes, give it in the other nostril.
- Start rescue breathing. Tilt their head back, pinch their nose, give one breath every 5 seconds. Keep going until they breathe on their own or help arrives.
- Stay with them. Even if they wake up, they can crash again. Don’t let them go to sleep. Wait for EMS.
That’s it. No complicated steps. No medical jargon. Just action.
Why This Matters More Than Ever
Fentanyl is in almost every illicit opioid now. The DEA says 82% of seized pills contain fentanyl. And it’s 50-100 times stronger than morphine. A tiny amount can kill. Someone might think they’re taking heroin or oxycodone-but they’re not. They’re taking something they can’t see, taste, or smell.That’s why training isn’t optional anymore. It’s basic safety-like smoke detectors. You don’t wait for a fire to install one. You install it because you care.
States with family overdose education programs have seen 22% fewer overdose deaths. That’s not a statistic. That’s 22% more people going home to their families. Your family could be one of them.
Where to Find Free Training
You don’t have to figure this out alone. Here’s where to start:- SAMHSA’s National Helpline: 1-800-662-HELP (4357). Free, confidential, 24/7. They’ll send you training materials.
- Overdose Lifeline App: Free download. Includes videos, quizzes, and step-by-step guides. Over 147,000 people have used it.
- Your local health department: Call and ask: "Do you offer free family overdose training with naloxone kits?" Almost all do now.
- YouTube: Search "family overdose recognition training". Channels like Overdose Lifeline and Harm Reduction Coalition have clear, real-world demos.
Don’t wait for a crisis to learn. Do it now. Not because you think it will happen. But because you love someone enough to be ready if it does.
Can I give naloxone to someone who didn’t take opioids?
Yes. Naloxone only works on opioids. If someone didn’t take opioids, it won’t hurt them. It won’t wake them up, but it won’t cause harm either. Always give it if you’re unsure-better safe than dead.
What if I’m afraid to call 911 because of legal trouble?
In all 50 states, Good Samaritan laws protect people who call for help during an overdose. You won’t get arrested for calling 911, even if drugs or paraphernalia are present. The law exists to save lives, not punish. Call anyway.
How long does naloxone last? Can someone overdose again after it wears off?
Naloxone lasts 30 to 90 minutes. Many opioids, especially fentanyl, last longer. That means someone can stop breathing again after naloxone wears off. That’s why you must keep monitoring them and wait for EMS-even if they seem fine.
Do I need training to get naloxone?
In 31 states, you can get naloxone without training. In 19, you need to complete a short training-usually 15-20 minutes. But even in states that require it, the training is free, simple, and often done over the phone or online. Don’t let this stop you.
Is it true that overdoses on darker skin are harder to spot?
Yes. Blue or purple lips are harder to see on darker skin. Instead, look for gray, ashen, or pale skin-especially around the lips, fingernails, and inside the mouth. Training materials now include skin tone guides to help families recognize these differences. Always use them.
Next Steps: What to Do Today
Don’t wait until tomorrow. Here’s your action plan:- Call your local health department and ask: "Where can I get free naloxone training and kits?"
- Download the Overdose Lifeline app. Watch the "Family Overdose Recognition" video.
- Buy or order a training naloxone kit. Keep it in your wallet, purse, or car.
- Have a 15-minute conversation with your family: "I’m getting this. I want you to know what to do too. Can we practice?"
- Print a skin tone guide and tape it to the fridge.
You’re not a hero. You’re a family member. And sometimes, being prepared is the most loving thing you can do.



Paul Dixon
Man, I wish my family had this info five years ago. We lost my cousin to a fentanyl overdose and none of us knew what was happening until it was too late. I keep a training kit in my glovebox now. Just did a quick demo with my niece last weekend-she thought it was a game until I showed her the difference between sleeping and overdosing. Now she knows what to do. That’s all that matters.
Vivian Amadi
Why are you giving out free naloxone like it’s candy? This isn’t a support group for drug users. You’re enabling them. If they wanted to live, they’d quit. Stop treating addiction like it’s a flat tire you can just fix with a spare.
Jimmy Kärnfeldt
There’s something beautiful about preparing for tragedy without expecting it. It’s like locking your door at night-not because you think someone’s coming, but because you love the people inside. This post isn’t about drugs. It’s about showing up for the people you care about when they can’t show up for themselves. I’ve taught my whole family using the Recognize-Respond-Revive method. We did it over pizza. No drama. Just love. And yeah, we’ve got the skin tone chart taped to the fridge.
Ariel Nichole
This is so important. I work in a community center and we’ve handed out over 200 free naloxone kits this year. People are scared to ask for help, but once they see how simple it is, they’re like, ‘Why didn’t someone tell me this sooner?’ Just one person learning this can save a life. And that’s worth every minute.
john damon
Yessss!! 👏👏👏 I got my kit last week and my mom cried when I showed her how to use it. We did it while watching Netflix. She said ‘I thought this was something only hospitals did.’ Nah, ma. It’s something family does. 💙
matthew dendle
so u just want people to carry narcan like its a damn flashlight? what next? free coffee for junkies? people need to stop being so soft. if u wanna die thats ur choice but dont make the rest of us babysit u
Monica Evan
I’m a nurse in rural Ohio and let me tell you-this isn’t theory. Last month, a grandma used the method from this post to save her grandson. She didn’t even know his name was on the DEA’s fentanyl watchlist. She just saw his lips turn gray, remembered the chart, and sprayed. EMS got there in 12 minutes. He woke up at 11. That’s the power of a fridge note and a little courage. You don’t need a degree. You just need to care enough to learn.
Taylor Dressler
One of the most practical, compassionate, and well-researched pieces I’ve read on this topic. The breakdown of opioid vs. stimulant signs is critical. Too many people assume overdose looks the same across all substances. The skin tone guide recommendation alone could prevent dozens of misdiagnoses. I’ve shared this with my entire extended family and our church group. Everyone should have access to this information.
Aidan Stacey
I used to think this was overkill. Then my brother OD’d in the bathroom while I was on the phone with him. I didn’t know what was happening until I saw his face-gray, not blue, because he’s Black-and his chest didn’t move. I screamed. I called 911. I gave the Narcan I’d gotten from the pharmacy after reading a Reddit post like this one. He lived. But I didn’t know what I was doing until it was too late. Don’t wait for your moment to be real. Make it real now.
Jean Claude de La Ronde
so you want us to arm the whole family with narcan like its a survival kit for a zombie apocalypse? next thing you know we’ll be teaching toddlers how to spray nasal spray at their uncle after he ‘falls asleep’ at thanksgiving. i mean… i guess if we’re gonna treat addiction like a weather event, fine. but lets be real-this is just a bandaid on a bullet wound
Jim Irish
Essential information. This should be mandatory in schools and community centers. The fact that we still treat this as a taboo topic is a failure of public education. The statistics speak for themselves. Time is life. Action saves lives. Simple as that.
Mia Kingsley
Wait so now we’re supposed to be drug cops for our own family? What next? Do I have to check my kid’s pockets every night? This is just guilt-tripping people into feeling responsible for someone else’s choices. I’m not babysitting my cousin’s addiction. He’s an adult. Let him deal with it.
Katherine Liu-Bevan
One thing this post doesn’t mention enough: naloxone doesn’t work on stimulant overdoses. That’s crucial. If someone’s seizing from meth, you need cooling, not Narcan. Calling 911 is still the priority. But people might assume spraying Narcan fixes everything. That’s dangerous. The difference between opioid and stimulant signs needs to be drilled into every family’s memory. This guide nails it.
Courtney Blake
Why should taxpayers fund this? These people made bad choices. Now we’re supposed to be their emergency crew? This isn’t healthcare-it’s enabling. If you’re going to destroy your life, don’t drag everyone else into it.
Lisa Stringfellow
Another feel-good post that ignores the real issue. People don’t overdose because they didn’t know the signs. They overdose because they’re addicted. No amount of training will fix that. This is just emotional theater to make people feel like they’re doing something while nothing actually changes.
Kristi Pope
I taught my whole family using the 20-minute method after my sister almost died. We practiced with the dummy spray while eating tacos. My 70-year-old dad got it in three tries. He said, ‘I’d rather be wrong than bury another child.’ We’ve got the chart on the fridge. We’ve got the kit in the glovebox. And we’ve got each other. That’s all you need. Love doesn’t need a medical degree.
Aman deep
From India-just read this and cried. We don’t talk about this here. But my cousin died last year from what we thought was a ‘bad high.’ I’m sharing this with my family tonight. We’ll get the app. We’ll learn. Because love doesn’t care about borders or stigma. If one life is saved because of this, it’s worth it.
Eddie Bennett
My mom used to say ‘If you’re gonna do drugs, at least do them right.’ Now she’s the one teaching her book club how to use Narcan. She got the training kit from the library. No big deal. Just a little prep. I used to roll my eyes. Now I’m the one reminding her to check the expiration date. We’re not heroes. We’re just not going to let fear keep us silent anymore.
Sylvia Frenzel
Why are we giving out free kits? Who’s paying for this? This is just another government handout for people who won’t take responsibility. We’re not babysitters. This isn’t a public service-it’s a moral hazard.