Nursing Perspectives: How Nurses Counsel Patients on Generic Medications
Why Nurses Are the Key to Patient Trust in Generic Medications
Most patients don’t know that 9 out of 10 prescriptions filled in the U.S. are for generic drugs. But when they see a pill that looks different-smaller, differently colored, or labeled with a name they’ve never heard-they panic. Generic medications aren’t cheaper because they’re weaker. They’re cheaper because they don’t carry the marketing costs of brand names. Still, patients worry. And that’s where nurses step in.
Nurses aren’t just giving out pills. They’re the ones who sit down with patients after a doctor orders a switch from brand to generic. They answer the unspoken question: Is this going to work like the one I’ve been taking? In hospitals, clinics, and even during home visits, nurses are the frontline educators who turn fear into understanding. And the data shows it works. When nurses properly explain generic drugs, patient adherence jumps by 22% to 37%.
What Nurses Actually Say to Patients
It’s not enough to say, “This is the same medicine.” Patients have heard that before-and they don’t believe it. Nurses use simple, real-world language. They say: “The FDA requires that generic drugs have the exact same active ingredient, in the same amount, and work the same way in your body as the brand name. They’re tested to make sure they’re absorbed into your bloodstream within the same range.”
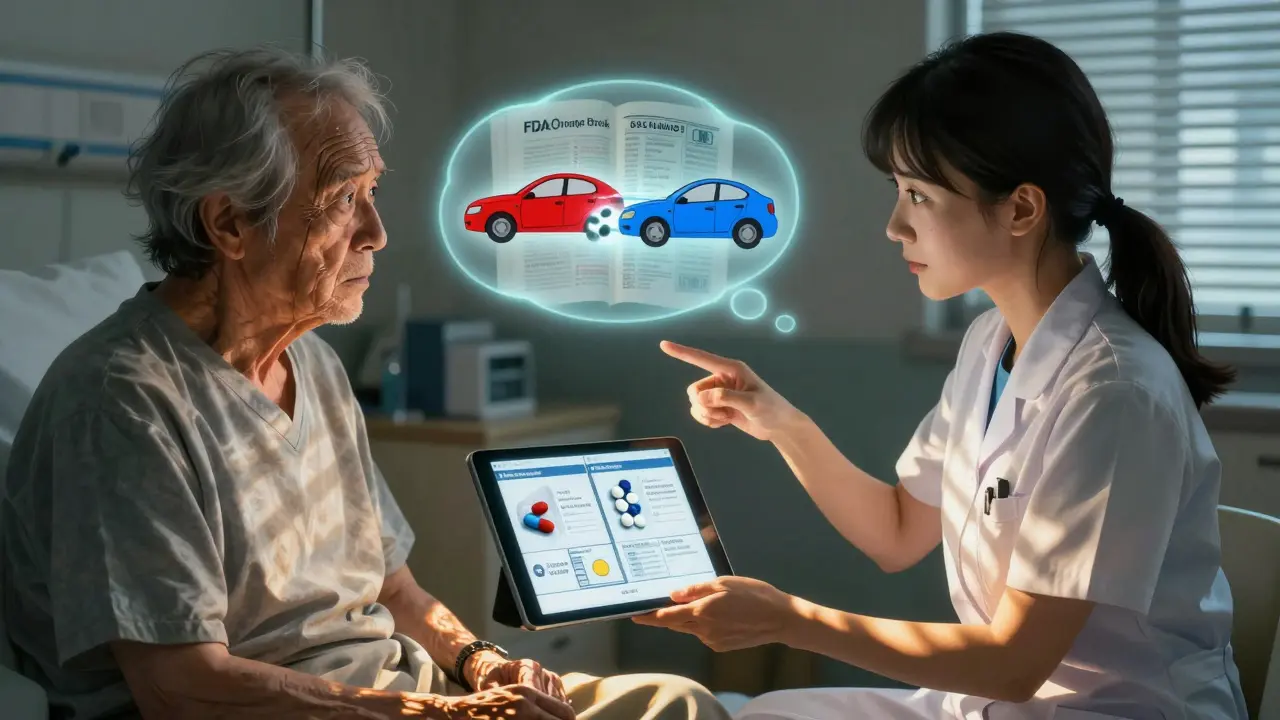
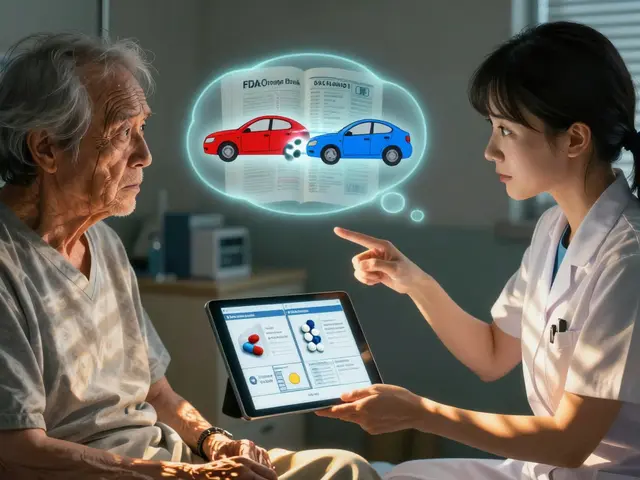
Then they get visual. Many nurses pull up the FDA’s Orange Book on a tablet or show printed pictures of both the brand and generic pills. They point out: “This is the same drug. Just made by a different company. Same rules. Same factory standards.”
One nurse at Johns Hopkins told a patient, “If your brand-name pill was a red car, this generic is a blue car. Different color, same engine, same gas mileage, same safety rating.” That kind of analogy sticks.
The Biggest Misconceptions Nurses Have to Fix
Patients think color changes mean weaker medicine. They think if the pill is smaller, it’s less potent. Some even believe generics are made overseas with lower quality control.
Nurses counter this with facts: All generic manufacturers-whether in the U.S., India, or Germany-must pass the same FDA inspections as brand-name makers. The FDA inspects every single manufacturing facility, and they don’t give a pass just because it’s a generic. In fact, 50% of brand-name drugs are made in the same plants as generics.
Another myth: “My doctor prescribed the brand for a reason.” Nurses explain that doctors often write prescriptions with the brand name out of habit. But unless the drug has a narrow therapeutic index-like warfarin, levothyroxine, or lithium-the switch is safe. Nurses know which drugs require extra caution and make sure patients understand the difference.

How Nurses Check That Patients Really Understand
Just explaining isn’t enough. Nurses use the “teach-back” method. After talking, they ask: “Can you tell me in your own words why we switched you to this pill?”
If the patient says, “Because it’s cheaper,” the nurse knows they didn’t get it. They go back and rephrase. If the patient says, “Because this one has the same medicine inside, just looks different,” then they’ve understood.
Over 90% of Magnet-designated hospitals require this step. It’s not optional. It’s part of the standard of care. And it’s the reason why patients who get counseling from nurses are 44% less likely to worry about generics over time.
When Things Go Wrong-and How Nurses Prevent It
Not every switch goes smoothly. A 68-year-old patient stopped taking levothyroxine after her generic pill changed color. She didn’t tell anyone. Three months later, she was hospitalized with myxedema coma-life-threatening thyroid failure. Her nurse later said, “We told her it was the same. But we didn’t ask her if she believed it.”
That case changed how some hospitals train nurses. Now, they’re taught to never assume understanding. They’re trained to ask: “What are you worried about?” and listen. Sometimes, the fear isn’t about the drug-it’s about losing control. A patient who’s been on the same brand for 10 years feels like they’re being forced into something new.
Nurses now carry visual aids: a small booklet showing side-by-side images of brand and generic versions of common drugs. They also use standardized scripts approved by their pharmacy and therapeutics committee. These scripts cover the eight key points required by national standards: drug name, use, dose, timing, side effects, what to do if missed, storage, and what to expect.
Why Nurses Are Better at This Than Pharmacists
Pharmacists counsel patients when they pick up their prescription. But that’s often a 5-minute conversation at the window. Nurses see patients daily. They’re there when the patient wakes up, takes their meds, and says, “This pill feels different.”
A 2022 study found that while pharmacists had slightly higher comprehension rates (93% vs. 89%), nurses were far better at handling real-time concerns. When a patient asked, “Why is my heart pill now blue?” the nurse could say, “Let me check your chart and explain why we switched you today.” Pharmacists can’t do that.
Nurses also connect the dots between medications. If a patient is on five drugs and three just switched to generics, the nurse can say, “You’re getting three new pills today, but they’re all the same as before. I’ll walk you through each one.” That kind of context matters.

What Nurses Wish More People Knew
Many nurses feel undertrained. A 2023 survey found that 41% of new nurses had never received formal instruction on how to explain generic drugs. That’s changing. The American Association of Colleges of Nursing now requires all nursing graduates to demonstrate competency in therapeutic equivalence.
But training isn’t just about knowledge. It’s about confidence. Nurses need to know the FDA’s bioequivalence range (80-125%) isn’t a loophole-it’s a tight, proven standard. They need to know which 15 drugs require extra care. And they need to know state laws vary: in some places, pharmacies can substitute without doctor approval; in others, they can’t.
One nurse summed it up: “I don’t care if the insurance company wants the cheapest option. If the patient doesn’t trust it, they won’t take it. And that’s more dangerous than any price tag.”
The Future: AI, Biosimilars, and What’s Next
By 2024, nearly half of U.S. hospitals use AI tools that give nurses instant access to FDA Orange Book data right at the bedside. Tap a button, and the screen shows: “This generic is rated AB-therapeutically equivalent to the brand.” No guesswork.
And it’s not just small pills anymore. Biosimilars-complex biologic drugs that mimic expensive cancer or arthritis treatments-are coming fast. By 2028, their use could triple. Nurses will need new training to explain how these work, because they’re not like simple generics. They’re harder to copy exactly.
Some hospitals are already testing something called the “Generic Medication Passport”-a small card patients carry that lists every generic they’ve been switched to, with photos and names. Nurses update it each time. It’s like a medication history book they can show to any provider.
What You Can Do as a Patient
If you’re switched to a generic, ask your nurse: “Is this the same medicine?” Then ask, “Can you show me how it’s the same?” Don’t be shy. Nurses are trained to answer. And if you’re worried, say so. Your concern matters.
Don’t stop taking your meds because the pill looks different. Talk to someone. A nurse, a pharmacist, your doctor. But don’t go silent. That’s how mistakes happen.



Amy Insalaco
The notion that nurses are the linchpin of generic medication adherence is not only reductive but statistically misleading. The 22-37% adherence increase cited is likely confounded by selection bias-patients who receive nurse counseling are already more health-literate or have better access to care. The real driver of adherence is systemic: insurance formularies, pill color psychology, and pharmaceutical lobbying, not some bedside epiphany from a nurse with a tablet. And let’s not romanticize the ‘teach-back’ method-it’s a bureaucratic checkbox, not a therapeutic breakthrough. The FDA’s bioequivalence range of 80-125% is a regulatory loophole disguised as science, and nurses are merely the compliant mouthpieces of a broken system.
kate jones
While the article presents a compelling case for nursing-led patient education, it’s important to contextualize the data. The 44% reduction in long-term worry among patients who received counseling is significant-but it’s also reflective of the trust relationship inherent in nursing, not just the content of the message. Nurses don’t just explain pharmacokinetics; they validate fear. That’s the unquantifiable variable. The ‘Generic Medication Passport’ idea is brilliant. Standardized visual aids, FDA Orange Book integration, and scripted counseling protocols should be mandatory nationwide. This isn’t just clinical practice-it’s patient rights advocacy in action.
Rob Webber
Nurses are being paid to do the job pharmacists should be doing. This whole thing is a cost-cutting scam by hospitals and insurers. You don’t need a nurse to tell you a blue pill is the same as a red one. You need a pharmacist who actually has time to talk. Stop glorifying underpaid staff doing the bare minimum because the system broke.
Yanaton Whittaker
America is falling apart because we let corporations dictate our health. Generic drugs? They're made in China and India by factories that don't even wash their hands before packaging. The FDA is a joke. I've seen pills that crumble in my hand. Nurses? They're just repeating corporate scripts. Wake up, people-your life is being traded for profit margins. 🇺🇸
Kathleen Riley
It is, perhaps, a salutary development that nursing practice has evolved to incorporate therapeutic equivalence education as a formal component of patient care. The epistemological shift-from passive dispensation to active epistemic mediation-is not merely clinical but profoundly ethical. The ‘teach-back’ methodology, in particular, aligns with the principles of hermeneutic pedagogy, wherein understanding is co-constructed through reciprocal dialogue. One must, however, remain cognizant of the ontological asymmetry between the clinician and the layperson; language, even when simplified, remains a vector of power.
Beth Cooper
Wait, so you're telling me the FDA approves generics from India and Germany but won't tell us which factories? And that 50% of brand-name pills are made in the same plants? That's just what they want you to think. The real manufacturers are in hidden labs in Eastern Europe, and the pills are tested on rats that don't even survive. My cousin's aunt's neighbor took a generic and started seeing colors. The nurses? They're paid by Big Pharma to smile and lie. Don't believe the hype.
Gaurav Meena
I'm from India, and I work in pharma manufacturing. Let me tell you-our plants meet FDA standards because we know the world is watching. We take pride in making safe, affordable meds. Nurses in the U.S. are doing amazing work, but they shouldn't carry this burden alone. We need global collaboration-not suspicion. Every pill, whether red or blue, should carry the same promise: healing. 🙏
Katie and Nathan Milburn
The assertion that nurses outperform pharmacists in real-time concern resolution is empirically plausible, given their longitudinal engagement with patients. However, one must interrogate the operationalization of ‘real-time’-is it temporal proximity or relational continuity that confers advantage? The institutional privileging of nursing over pharmacy in this domain may reflect structural hierarchies within healthcare ecosystems rather than inherent superiority of pedagogical technique. A nuanced systems analysis is warranted.
Beth Beltway
Let’s be real: this whole article is a PR campaign disguised as healthcare insight. Nurses aren’t ‘educating’ patients-they’re damage control for a broken system. The fact that 41% of new nurses haven’t been trained on this? That’s not a gap-it’s a crime. And now they want to slap a ‘passport’ on patients like they’re carrying contraband? This isn’t patient empowerment. It’s corporate liability management with a bow tied by nursing schools. Stop pretending this is about care.
Natasha Plebani
The transition from brand to generic is not merely a pharmacological event-it is an ontological rupture in the patient’s relationship with their own body. The pill, once a symbol of continuity, becomes an alien object. The nurse’s role, then, is not to explain equivalence, but to restore narrative coherence. The ‘teach-back’ method is a ritual of reintegration: the patient speaks the truth of their understanding, and in that utterance, the fear is exorcised-not by science, but by voice. The FDA’s 80-125% range? It is not a margin of error. It is a metaphysical allowance for human variability. We are not machines. Neither are our medicines.
Niamh Trihy
This is a beautifully articulated account of nursing’s underappreciated role in medication safety. The emphasis on visual aids and standardized scripts is particularly commendable. In Ireland, we’ve adopted similar approaches with our Community Pharmacy Medication Review service-though we don’t yet have AI integration. One addition I’d suggest: incorporating patient testimonials into training. Hearing a peer say, ‘I was scared too, but this worked,’ can be more powerful than any FDA chart. Also, kudos to the nurse who said, ‘If the patient doesn’t trust it, they won’t take it.’ That’s the core of care, right there.