Tiered Copays: Why Your Generic Prescription Might Cost More Than Expected

You picked up your generic levothyroxine at the pharmacy, expecting to pay $5 like last month. Instead, the cashier says $45. You ask why. They shrug. Your doctor says all generics are the same. So why does one cost nine times more?
This isn’t a mistake. It’s by design. And it’s happening to millions of people on Medicare, employer plans, and even Medicaid. The reason? Tiered copays.
How Your Prescription Got Put on a Ladder
Back in the late 1990s, pharmacy benefit managers-companies like CVS Caremark, Express Scripts, and OptumRx-started grouping drugs into tiers. The idea was simple: reward patients for choosing cheaper drugs by making those drugs cheaper to buy. Tier 1 was for the cheapest generics. Tier 2 for preferred brand names. Tier 3 for non-preferred brands. And so on.
By 2025, nearly every health plan in the U.S. uses this system. Medicare Part D plans? 99% use tiers. Employer plans? 98%. The goal wasn’t just to save money for insurers-it was to nudge patients toward drugs that gave the biggest discounts to the middlemen.
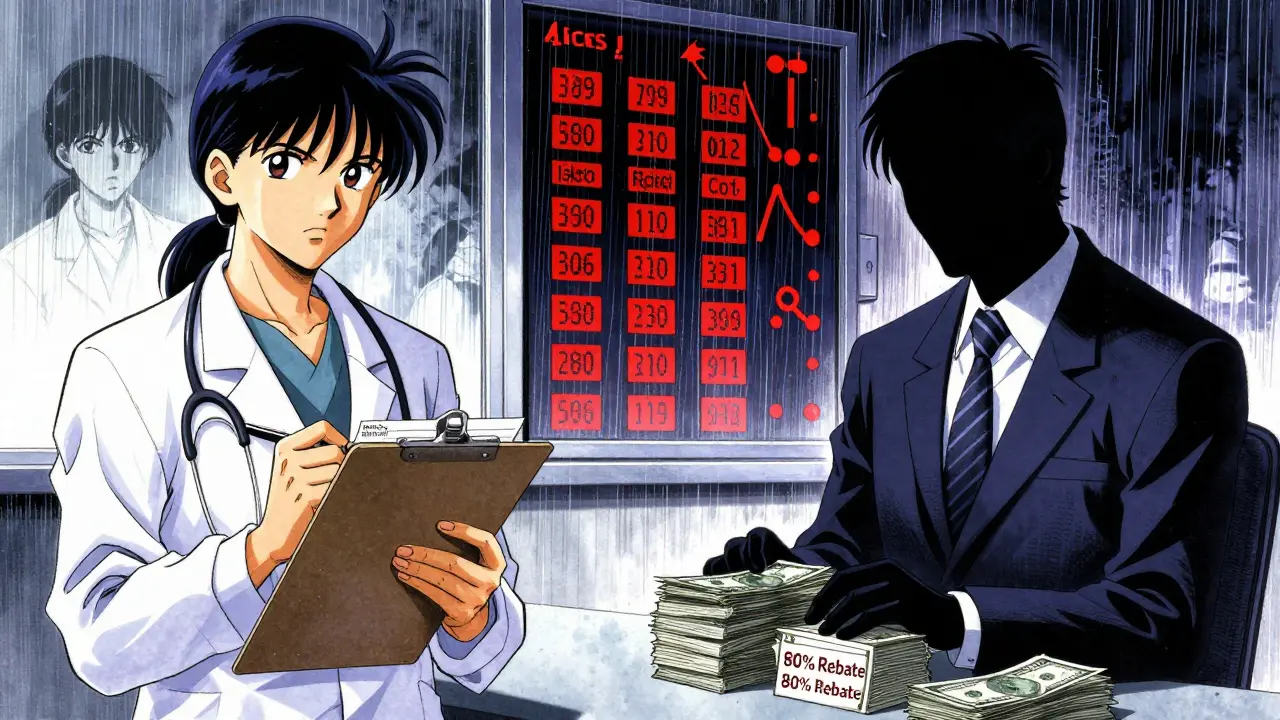
Here’s the catch: the tier a drug lands in has almost nothing to do with how well it works. It’s all about rebates.
Why Your Generic Is in Tier 3 (Even Though It’s the Same Drug)
Let’s say you take a generic version of lisinopril for high blood pressure. There are dozens of manufacturers making it. One company pays the PBM a big rebate-say, 80% off the list price. That drug gets placed in Tier 1: $5 copay.
Another company makes the exact same pill. Same active ingredient. Same FDA approval. But they didn’t offer a big enough rebate. So the PBM puts their version in Tier 2: $25 copay.
That’s not a clinical decision. That’s a business deal. And you’re the one paying the difference.
According to a 2023 analysis by BOC Pharmacy Group, 12-18% of generic drugs are classified as specialty medications-not because they’re complex, but because they cost more than $600 per month to make. Even if they’re chemically identical to cheaper generics, they get shoved into Tier 4 or 5.
And when your plan changes its contracts? Your drug can jump tiers overnight. In early 2024, Express Scripts moved 87 generic drugs to higher tiers because their rebate deals expired. No warning. No notice. Just a higher bill at the counter.
Specialty Generics: The Hidden Trap
Some of the most confusing cases involve generic versions of biologic drugs-like adalimumab (Humira’s generic). These aren’t your typical pills. They’re complex, injectable medications used for rheumatoid arthritis, Crohn’s disease, or psoriasis.
Even though they’re technically generics, they cost $5,000 to $10,000 a month. So insurers don’t use flat copays. They use coinsurance: 25-40% of the total cost.
That means even if you’re on a $500 monthly premium plan, your out-of-pocket for one dose could be $1,250. And you might not know until you get the bill.
Patients often don’t realize they’re paying coinsurance on a generic until they’re already in debt. That’s because the label says “generic.” But the formulary doesn’t.
Why Insurers Won’t Explain It
When people ask why their generic costs more, insurers give vague answers: “It’s not a preferred generic.” “It’s on a different tier.”
They don’t say: “We didn’t get a big enough kickback from the manufacturer.”
A 2023 Patient Advocate Foundation survey found that 41% of insured adults had experienced a generic drug suddenly costing more-with 68% unable to get a clear reason why. Reddit threads like “Why is my generic drug suddenly Tier 3?” are full of frustrated patients who feel tricked.
Doctors often don’t know either. They see “generic” and assume it’s the cheapest option. But the pharmacy’s system tells a different story.
What You Can Do About It
You’re not powerless. Here’s how to fight back:
- Check your formulary every October. That’s when Medicare and many employer plans update their drug lists. Go to your insurer’s website. Look for “Drug List” or “Formulary.” Search your medication by name.
- Use tools like GoodRx or SmithRx. These sites show you exactly what each generic version costs across different tiers. You might find the same drug for $10 less just by switching manufacturers.
- Ask your pharmacist for alternatives. Pharmacists know which generics are in Tier 1. They can often switch your prescription without calling your doctor-if it’s clinically acceptable.
- Request a therapeutic interchange form. If your drug moved to a higher tier, ask your doctor to fill out a form asking for an exception. In 63% of cases, insurers approve these requests if the drug is medically necessary.
- Check manufacturer assistance programs. Many drugmakers offer coupons or free programs for patients who can’t afford their meds-even for generics. Sites like NeedyMeds list them.
One patient on Medicare switched from a Tier 3 generic of metformin to a Tier 1 version using GoodRx. Her monthly cost dropped from $42 to $7. That’s $420 a year saved-just by asking the right questions.

The Bigger Picture
Tiered copays were meant to lower overall drug spending. And they did-by 8-12%, according to studies from Health Affairs. But the savings didn’t go to patients. They went to PBMs and insurers.
Now, with the Inflation Reduction Act capping out-of-pocket drug costs at $2,000 per year for Medicare Part D (starting 2025), pressure is building to simplify these systems. Some lawmakers want to ban tiering for generics entirely.
But for now, the system stays. And the confusion continues.
Don’t assume your generic is cheap. Don’t assume your doctor knows the real cost. And don’t accept a surprise bill without asking: Why is this the same drug costing more?
It’s not about quality. It’s not about safety. It’s about who paid the rebate.
Why is my generic drug more expensive than the brand-name version?
It’s rare, but it happens. Some brand-name drugs are placed in lower tiers because the manufacturer pays a big rebate to the pharmacy benefit manager (PBM). Meanwhile, the generic version may be in a higher tier if its maker didn’t negotiate a good discount. The brand might cost $50 with a $40 rebate, making it cheaper than a generic with no rebate. Always check your plan’s formulary instead of assuming brand = expensive and generic = cheap.
Can my pharmacist switch me to a cheaper generic without asking?
Yes, in many states, pharmacists can substitute a preferred generic even if your prescription says “dispense as written.” But they’re not required to tell you. That’s why you might get a different pill with a higher copay. Always ask your pharmacist: “Is this the same drug my doctor prescribed? What tier is it on?”
Do all generic versions of a drug work the same?
Yes, legally. The FDA requires all generic drugs to have the same active ingredient, strength, dosage form, and bioavailability as the brand. That means they’re just as effective. But inactive ingredients (like fillers or dyes) can vary, and some patients report differences in side effects or how the pill feels. If you notice a change after switching generics, tell your doctor.
How often do drug tiers change?
Most plans update their formularies once a year, usually in October. But 17% of commercial plans made changes between January and June 2023, according to CMS data. If your copay suddenly jumps, it’s likely due to an expired rebate deal between the PBM and the drugmaker-not because your condition changed.
Is there a law that stops insurers from charging more for generics?
Not yet. But bills like the bipartisan Prescription Drug Pricing Reduction Act are being discussed in Congress to limit tiering for generics. Some states, like California and New York, have passed laws requiring insurers to disclose tiering reasons. Federal rules are still catching up. For now, the system remains legal-but increasingly controversial.
What’s Next?
The trend is clear: drug pricing is getting more complex, not less. As specialty drugs and biosimilars grow, insurers will keep using tiered systems to manage costs. But patients are starting to push back.
Next time you’re handed a prescription and told it costs more than expected, don’t just pay it. Ask why. Check the formulary. Talk to your pharmacist. Use GoodRx. File an exception. You’re not just saving money-you’re holding the system accountable.




Cara Hritz
so i just got charged $52 for my metformin and i thought i was getting a deal?? like wtf is this system even??
Art Van Gelder
Let me tell you, this isn’t just about rebates-it’s about power. The whole pharmacy benefit manager ecosystem is a Rube Goldberg machine built to extract money from sick people while pretending to be a cost-saver. You think your doctor’s prescribing you a drug? Nah. They’re prescribing you a product in a contract between a corporation and a middleman who doesn’t even have a license to practice medicine. And we’re supposed to be grateful when we get the ‘cheaper’ version? The version that didn’t bribe the system enough? This isn’t healthcare. It’s corporate theater with a stethoscope.
Ajay Brahmandam
in india we dont have this tiered mess but i know people who pay 200 rupees for levothyroxine and its the same pill. the system is broken everywhere.
Aliyu Sani
yo this is pure capitalism on crack. PBMs are the new loan sharks but instead of debt they weaponize your thyroid. they dont care if you live or die-only if the rebate check clears. i swear if i see one more 'generic' label with a $45 price tag im gonna start a protest outside a CVS with a sign that says 'MY MEDS AREN'T A STOCK OPTION'.
Jamison Kissh
It’s fascinating how the system was designed with good intentions-lower costs through incentives-but evolved into a perverse incentive structure where the most effective drug isn’t the cheapest, but the one that paid the most to the middleman. The FDA certifies bioequivalence, yet the formulary ignores it. The result? A paradox: identical pills, different prices, and patients left to navigate a labyrinth designed to confuse. It’s not incompetence-it’s architecture. And we’re the ones paying rent.
Johnnie R. Bailey
Here’s what nobody tells you: pharmacists know which generics are in Tier 1. They just don’t always tell you unless you ask. I used to get my lisinopril for $40 until I asked my pharmacist, 'Is there a cheaper version?' She switched me to the same pill, different manufacturer, same FDA code-now it’s $7. No doctor visit. No paperwork. Just a question. If you’re paying more than $15 for a common generic, you’re not being smart-you’re being passive. Check GoodRx before you pay. Always. And if your plan changes tiers without notice? File an appeal. They approve 60% of them. The system wants you to give up. Don’t.
Nader Bsyouni
you people are so naive. the real problem is that you think medicine should be affordable. it's not a public good. it's a product. if you can't afford your pills then maybe you shouldn't be sick. also who even uses goodrx? that's for peasants.
Jim Brown
One must consider the moral economy of pharmaceutical distribution. The tiered copay structure is not merely an economic mechanism-it is a symbolic enactment of societal stratification, wherein health outcomes become contingent upon the negotiation power of corporate entities rather than the physiological needs of the individual. To accept this system as inevitable is to abdicate our collective responsibility to redefine health as a right, not a commodity indexed to rebate percentages. The FDA may certify chemical equivalence, but it cannot certify moral equivalence. And therein lies the true crisis.
jenny guachamboza
ok but what if this is ALL a deep state plot to control the population?? 😱 like the same people who run the PBMs also run the CDC and the FDA and they want us dependent on expensive meds so we stay docile and don’t protest?? and they use the ‘generic’ label to trick us?? i read a guy on 4chan who said the real levothyroxine is only made in one lab in Switzerland and the rest are government drones?? 🤯